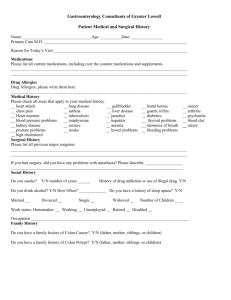
COMMONWEALTH GASTROENTEROLOGY, PLC

NOTHERN VIRGINIA GASTROENTEROLOGY, P.C
Gastroenterology History Form
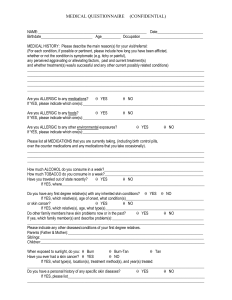
Name: _______________________________________________________ Date: __________________
Referring Physician/ Primary Care Physician: ________________________________________________
Date of Birth: _____________
Reason for Visit:
___________________________________________
____________________________________________________
____________________________________________________
____________________________________________________
____________________________________________________
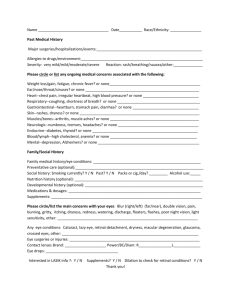
Medical History: Please check any of the conditions that represent a significant problem for you
GENERAL
Fever
YES GASTROINTESTINAL
Abdominal pain
YES MUSCULOSKELETAL
Recent Fractures
YES
Chills
Night Sweats
Recent Weight Changes
EYES
Glasses
Contacts
Glaucoma
Nausea
Vomiting
Heartburn
YES Indigestion
Pain with Swallowing
Difficulty Swallowing
Diarrhea
Muscle Aches/Pains
Arthritis
ENDROCRINE
Heat intolerance
Cold intolerance
Hot flashes
Excessive thirst
YES
Eye dryness
Eye redness
Irregular heart beat
Heart attack or failure
Heart murmur
Heart valve problems
Blood clots
Leg /Ankle swelling
Constipation
Blood in Stool
Eye pain Pain with having a BM
EARS, NOSE, MOUTH YES Gallbladder Problems
Nose bleeds
Sinus problems
Earache
RESPIRATORY
Cough
Wheezing
YES
Loss of appetite
Gas/Bloating
Black Stool
GENITOURINARY
Painful urination
Urinary Urgency
Shortness of breath
Asthma
Blood in urine
Recurrent bladder infections
CARDIOVASCULAR YES Abnormal vaginal bleeding
Chest pain Sexual problems
Heart palpitations Menstrual problems
Flushing
Changes in body hair
SKIN
Rash
Dryness
Itching
Jaundice
YES Easy bruising
Psoriasis
Eczema
Pigment changes
NEUROLOGIC
Numbness
Dizziness
Paralysis
PYSCHIATRIC
Depression
Anxiety
OTHER
YES
YES
YES
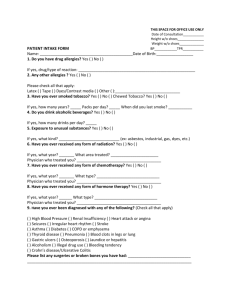
Please list all of your medications, including over the counter medications (If you need additional space, please bring a list to your appointment.) Include Medication Name, Dosage and Number of times per Day
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
Please list all allergies including medications, food, and environmental
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
Past Medical History: Please list any medical conditions you have been diagnosed with or are being treated for:
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
________________________________________ ____________________________________________
Number of Pregnancies ________ Number of Live Births _______
Pneumonia Vaccine __________________Flu Shot ____________________
Hepatitis A Vaccine _______________ Hepatitis B Vaccine __________________ TB Skin Test ________________
Please list any past surgeries
Date Surgeries
Family History (If a relative has had cancer, please specify type)
Relative Age Living Deceased Disease or Cause of death
Social History:
Marital Status: Single ___ Divorced ___
Married ___ Widow/Widower ____Other __
Do you smoke? Yes __
No __
If yes, how many packs per day?_________________________________
Did you smoke? Yes __
No __
If yes, when did you quit? ______________________________________
Do you drink alcohol? Yes ___
No ___
If yes, indicate on average how much and circle day, week, or month:
_______Beer per: Day __
Week ___
Month ___
_______Glasses of wine per: Day ___
Week ___
Month __
_______Mixed drinks per: Day ___
Week ___
Month ____
Do people get annoyed by your drinking? Yes __
No ___
Do you feel guilty about drinking? Yes __
No ___Do you drink alcohol in the morning? Yes __
No __
Do you or have you ever-used intravenous (IV Drugs)? Yes __
No __
Do you have Tattoos? Yes __No __
DO YOU HAVE ANY OTHER PROBLEMS YOU WANT TO DISCUSS? Yes ___
No ____
Caffeine Use: Please indicate how much of caffeine you consume below:
(Caffeinated beverages include coffee, tea, green tea, sodas, chocolate, energy drinks)
Caffeinated beverages per: Day_____ Week_____
Patient signature_______________________________________________ Date ___________________________
Physician signature _____________________________________________Date ___________________________