S. pneumo Blood Cx - Navy Emergency Medicine
advertisement

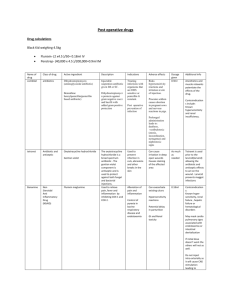
ED Management of Positive Blood Culture for Streptococcus Pneumoniae in Infants and Children Positive Bld Cx S. pneumoniae Yes Toxic-appearing1? Repeat Bld Cx LP, IV Abx2 Consider CXR Admit Immunocompromised? Serious focal infection3? No No Fever? (T > 38 C. rectal) Oral Abx4 Repeat Bld Cx5 Yes Repeat Bld Cx Consider LP 6 Ceftriaxone7 Eval 24 hrs8 Notes: 1 Toxicity=altered mental status, poor eye contact, inappropriate response to stimuli, abnormal vital signs, poor skin perfusion, cyanosis, grunting 2 IV Abx=Ceftriaxone 50-75 mg/kg/day Q24H OR Cefotaxime 60 mg/kg/dose IV Q8H, add Vancomycin 60 mg/kg/day div Q6H if CSF gm stain + for GPC 3 Serious focal pneumococcal infection=meningitis, pneumonia, septic arthritis, osteomyelitis, pericarditis, endocarditis. The risk of serious focal infections or sepsis has been estimated to be 6% for S. pneumoniae. 4 Oral Abx=Amoxicillin 80 mg/kg/day div BID X 7-10 days, if PCN-allergic use Biaxin 15 mg/kg/day div Q12H X 7-10 days 5 Repeat blood culture only if antibiotics not received at first visit because these patients are at high risk for persistent bacteremia. 6 Assess for symptoms/signs of meningitis, which may be subtle or absent in patients who have been partially treated with antibiotics. Perform LP in any 1 Guideline for Management of Positive Blood Culture for S. pneumoniae in Children patient in whom meningitis is suspected. Consider LP in patients < 12 months even if asymptomatic. 7 Ceftriaxone 50 mg/kg IM/IV (max 1 gm) 8 Outpatients with continued fevers should be admitted for parenteral antibiotic therapy and evaluation of secondary sites of infection. References: Bratton L, Teele DW, Klein JO: Outcome of unsuspected pneumococcemia in children not initially admitted to the hospital. J Pediatr 1977;90:703-706 [In a review of 97 episodes of pneumococcal bacteremia (PB), PB was found in 2 of 46 children treated with an antibiotic at the initial evaluation and in 13 of 51 untreated patients (3 with a new diagnosis of pneumonia and 1 with meningitis; P = .007). One of the 15 patients with PB was afebrile (an untreated patient). Of the 46 treated patients, 31 (67 %) were followed as outpatients and all did well. Of the 51 untreated patients, 20 (40%) were managed as outpatients and 1 developed meningitis (this patient was 1 of 5 patients not prescribed any antibiotics at the second visit)] Bass JW, Steele RW, Wittler RR et. al: Antimicrobial treatment of occult bacteremia: a multicenter cooperative study. Pediatr Infect Dis J 1993;12:466-473 [In a prospective trial of antibiotic treatment of occult PB (amoxicillin/clavulanate versus ceftriaxone), none of the 33 ceftriaxone-treated patients had fever at the 24-hour followup visit compared with 4 of 18 oral antibiotic treated patients. None of the patients in either group had PB, and most patients were continued on an oral antibiotic for 7-10 days] Korones DN, Shapiro ED: Occult pneumococcal bacteremia: what happens to the child who appears well at reevaluation? Pediatr Infect Dis J 1994;13:382-386 [Of outpatient children reevaluated for PB who were well-appearing and afebrile, 76% had received an antibiotic (65% oral; 11% parenteral) at the initial visit when the blood cx was drawn. Of four (3.6%) of these well-appearing, afebrile children with persistently culture-positive invasive pneumococcal infections (3 with bacteremia and 1 with meningitis), 3 patients had been treated with an oral antibiotic before the reevaluation and 1 patient had not received any antibiotic therapy. 19 patients with PB who were afebrile but ill-appearing at reevaluation did not have any new focus of infection or PB] Kuppermann N: Occult bacteremia in young febrile children. Pediatr Clin North Am 1999;46:1073-1109 [Repeat blood cultures are likely unnecessary for well-appearing children who were treated with empiric antibiotics and are afebrile at follow-up. For children who are illappearing or febrile at follow-up, a complete evaluation including lumbar puncture should be performed and hospitalization should be strongly considered] 2 Guideline for Management of Positive Blood Culture for S. pneumoniae in Children Bachur R, Harper M: Reevaluation of outpatients with Streptococcus pneumoniae bacteremia. Pediatrics 2000;105:502-509 [All patients with PB need prompt evaluation. The majority of children with PB can be managed as outpatients. Those not receiving antibiotics at the initial evaluation and those who remain febrile are at highest risk for persistent bacteremia. Use of an antibiotic at the initial visit did not confuse the management of any patient with meningitis] 3 Guideline for Management of Positive Blood Culture for S. pneumoniae in Children