Query Documentation for Inpatient Services
advertisement

DEPARTMENT: Health Information
Management Services
PAGE: 1 of 8
EFFECTIVE DATE: April 30, 2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
SCOPE: All personnel responsible for performing, supervising or monitoring coding of inpatient
services including, but not limited to:
Facility Health Information Management
Corporate Health Information Management Services
Case Management/Quality Resource Management
Service Centers
Administration
External Coding Contractors
Ethics and Compliance Officer
Physician Advisors
This policy applies to queries initiated for all inpatient services provided in Company-affiliated
facilities (acute care, freestanding psychiatric, and rehabilitation) unless otherwise indicated in a
separate policy. For queries specific to the assignment of ICD-9-CM code of 482.83 (Pneumonia
due to other gram-negative bacteria), refer to Company Policy Memorandum entitled Special
Coding Practices on ICD-9-CM Code 482.83 dated October 20, 2000. For outpatient services,
refer to the Coding Documentation for Outpatient Services Policy, HIM.COD.002. For skilled
nursing services, refer to the Coding Documentation for Skilled Nursing Facilities/Units Policy,
HIM.COD.010. For rehabilitation services, refer to the Coding Documentation for Rehabilitation
Facilities Policy, HIM.COD.013.
PURPOSE: The purpose of this policy is to define when a query will be initiated and outline the
appropriate query processes to be used. Appropriate querying will improve the accuracy, integrity
and quality of patient data; minimize variation in the query process; and improve the quality of the
physician documentation within the body of the medical record to support code assignments. A
query is an established mechanism of communication between coders and physicians to clarify
ambiguous, incomplete or conflicting documentation in the medical record in order to facilitate
complete, accurate and consistent coding practices. The Company has developed and approved
standardized query forms. The selection of the appropriate standardized form will be determined
based on the type of query being initiated. The approved and required standardized query forms
are attached to this policy.
POLICY: When the documentation necessary to assign an ICD-9-CM code for an inpatient case is
not clearly stated within the medical record or is conflicting or ambiguous, a query is required
(unless otherwise indicated in a separate Company Policy Memorandum). Company facilities will
follow the Official Guidelines for Coding and Reporting diagnoses and procedures published in
AHA Coding Clinic for ICD-9-CM, Fourth Quarter, 1999 and Fourth Quarter, 2002 and/or the
most current AHA Coding Clinic for ICD-9-CM Guidelines.
4/2005
DEPARTMENT: Health Information
Management Services
PAGE: 2 of 8
EFFECTIVE DATE: April 30, 2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
PROCEDURE:
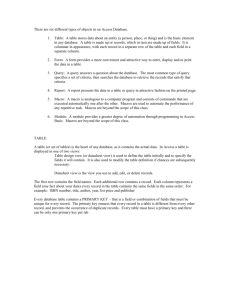
1. The Query Process
The coder is required to query the physician participating in the care of the patient once a
diagnosis or procedure has been determined to meet the AHA Coding Clinic for ICD-9-CM
official coding guidelines for reporting but has not been clearly stated within the medical
record, or when conflicting or ambiguous documentation is present. Additional guidance
regarding implementation and use of appropriate queries can be found in the HCA HIMS
Query Handbook, which is located on the Company’s Intranet site on the Health Information
Management Services page.
a. Query Documentation
The query documentation must include:
(1)
the name of the individual submitting the query;
(2)
the patient’s name;
(3)
the patient’s medical record number;
(4)
the patient’s account number;
(5)
the date the query was submitted;
(6)
an itemization of clinical findings and/or medical record documentation
pertinent to the condition/procedure in question including the source
document(s) from the medical record supporting the query; and
(7)
the statement of the issue in the form of a question.
b.
4/2005
Query Format
i) If a query is necessary to clarify ambiguous or conflicting documentation in the
medical record in order to facilitate complete, accurate and consistent coding
practices, the query must be documented on one of the approved separate query
forms.
ii) A question on the query form must be posed to elicit only one answer about a
condition and/or types of conditions.
iii) It is appropriate to ask the physician multiple questions if there are multiple
conditions that require clarification, however, each question must be on a separate
query form.
iv) The approved query forms include all of the required query elements and are attached
to this policy.
v) The selection of the approved query form will be determined based upon the specific
type of query that is being initiated. The determination of the appropriate method or
approach to the query must be based on the following:
(1) Pneumonia:
i. If the physician has documented pneumonia in the medical record and there
is a positive sputum culture, use query form A to determine if further
specificity related to the type of pneumonia can be obtained.
DEPARTMENT: Health Information
Management Services
PAGE: 3 of 8
EFFECTIVE DATE: April 30, 2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
ii. If the physician has documented pneumonia in the medical record and there
is not a positive sputum culture, do not query. However, if there are
extensive clinical indications of aspiration pneumonia, see iii immediately
below.
iii. If there are extensive clinical indications of aspiration pneumonia, use query
form B as a means to clarify if aspiration pneumonia is or is not present. By
extensive, it is meant that the physician has substantially described
aspiration pneumonia but has not made the specific or particular diagnosis.
iv. If the purpose of the query is not included as one of the above conditions,
use query form F.
(2) Septicemia and Sepsis
The Official Guidelines for Coding and Reporting of Coding of septicemia,
SIRS, sepsis, severe sepsis and septic shock were updated in the AHA
Coding Clinic (4Q 2003 79-80, 113-115). Septicemia is now defined as a
systemic infection that is more clinically significant than bacteremia, but has
not progressed to a generalized sepsis. The medical record must be
reviewed to determine whether sufficient clinical indicators are present to
support a query for a more specified condition, and/or requires a link
between the documented condition, and a positive blood culture. The
following scenarios must be considered in order to select the most
appropriate query form:
i. If the physician has recorded the diagnosis of sepsis and there is no positive
blood culture, a query is not necessary and sepsis should be reported based
on physician documentation.
ii. If the physician has documented sepsis in the medical record and there is a
positive blood culture, use query form C to determine if further specificity
related to the type of sepsis can be obtained.
iii. If the physician has documented septicemia in the medical record and there
is a positive blood culture, but not extensive clinical indicators for sepsis,
use query form H to determine a link between the septicemia and positive
blood culture. Extensive clinical indicators are defined by the AHA
Coordination and Maintenance Committee as two or more clinical indicators
that describe the clinical picture for a generalized sepsis. The clinical
indicators for generalized sepsis are outlined on query form D.
iv. If the physician has documented a localized infection (e.g., urinary tract
infection, cellulitis) or a systemic infection (septicemia) and there are
extensive clinical indicators of a generalized sepsis, use query form D. By
extensive, it is meant that the physician has substantially described the
clinical condition of sepsis, using two or more clinical indicators that
describe the clinical picture of a generalized sepsis, but has not made the
4/2005
DEPARTMENT: Health Information
Management Services
PAGE: 4 of 8
EFFECTIVE DATE: April 30, 2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
specific or particular diagnosis. Extensive clinical indicators of sepsis
include fever or hypothermia, tachypnea, tachycardia, increased white blood
cell count (WBC)>12,000/mm3 or < 4,000mm 3 or > 10% immature
neutrophils) leukocytosis, shock, altered mental status, metabolic acidosis,
oliguria and positive blood cultures. Physicians should not be queried for
generalized sepsis based on documented septicemia alone. There must be
two or more clinical indicators as listed above in order to substantiate the
need for clarification based on clinical indicators of a symptomatic systemic
infection (sepsis).
v. If the physician has documented a localized infection (e.g., urinary tract
infection, cellulitis) or a systemic infection (septicemia) and there are not
extensive clinical indicators of a generalized sepsis (two or more clinical
indicators that describe the clinical picture of a generalized sepsis), a query
is not warranted and the code assignment should be reported to the highest
level of specificity based upon the physician documentation in the medical
record.
vi. If the physician has documented urosepsis and there are extensive clinical
indicators of a generalized sepsis and clarification is needed to determine
whether this is a localized urinary tract infection or a generalized sepsis, use
query form E.
vii. If the purpose of the query is not included as one of the above conditions,
use query form F.
(3) Acute Blood Loss Anemia
i. If the physician has recorded the diagnosis of unspecified anemia and there
is no documentation of an acute blood loss, a query is not necessary and
anemia should be reported based on physician documentation.
ii. If the physician has documented anemia in the medical record and there is
documentation of an acute blood loss, use query form G to determine if
further specificity related to the type of anemia can be obtained.
iii. If the physician has documented extensive clinical indicators of acute blood
loss anemia, use query form G. By extensive, it is meant that the physician
has substantially described the clinical condition of anemia, but has not
made the specific or particular diagnosis.
iv. If the physician has documented blood loss and there are not extensive
clinical indicators of an acute blood loss anemia, a query is not warranted
and the code assignment should report the highest level of specificity based
upon the physician documentation in the medical record.
v. If the purpose of the query is not included as one of the above conditions,
use query form F.
4/2005
DEPARTMENT: Health Information
Management Services
PAGE: 5 of 8
EFFECTIVE DATE: April 30, 2005
(4)
c.
4/2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
Any Other Queries
For any other query that is required to clarify ambiguous, incomplete or
conflicting information contained in the medical record, use query form F.
Maintenance of the Query Form
i) The coding query process can be conducted and documented on a concurrent (predischarge), retrospective (post-discharge) or post initial billing basis.
ii) The query may be posed verbally or in writing; the query (whether verbal or in
writing) must be documented on one of the approved and required standardized
query forms; and maintained in the body of the medical record.
iii) The facility must ensure that the reimbursement received by the facility is appropriate
based upon the acceptable medical record documentation.
iv) If the purpose of the query process is not for clarifying ambiguous or conflicting
documentation for coding purposes, e.g., certification for insurance purposes, follow
the applicable facility policies regarding the maintenance of this information.
a. Concurrent - A concurrent query is defined as one that is initiated before the
patient has been discharged from the facility. The concurrent query is initiated
to clarify documentation for the purpose of final code assignment.
b. Retrospective – A retrospective query is defined as one that is initiated after the
patient has been discharged from the facility, but before the claim has been
billed.
c. Post Initial Billing - The post initial billing query is defined as a query that is
executed as a result of additional documentation (e.g., discharge summary)
being added to the record or findings during a retrospective coding review
(internal or external) that occurs after the claim has been billed.
i. Query initiation for post initial billing can only occur within 12-months of
the discharge date.
ii. The physician response to post initial billing the query must be obtained
within 2 weeks (14 calendar days) of the query initiation and must also be
within 12 months of the discharge date. If the physician’s response to the
post initial billing query generated is not obtained within 2 weeks, the query
is neither considered nor acceptable for supporting the code/DRG
assignment.
iii. If a chart needing the post initial billing query is beyond 12 months from the
discharge date, a query should not be initiated.
iv. If the physician’s response substantiates a lower weighted DRG, the claim
must be rebilled following Company overpayment rebilling guidelines.
v. If the physician’s response substantiates a higher weighted DRG, the claim
should be rebilled if it is within the appropriate rebilling timeframe (60 days
from the remittance advice date).
DEPARTMENT: Health Information
Management Services
PAGE: 6 of 8
EFFECTIVE DATE: April 30, 2005
d.
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
Query Response
The query response from the physician that will be used to support a code assignment must
be documented by the physician in the body of the traditional medical record and/or, at a
minimum, on the query form (which must be kept as a permanent part of the medical
record). The traditional medical record is defined as the customary forms, based on the
patient type, which are contained in the medical record to furnish documentary evidence of
the course of the patient’s illness and treatment during each hospital admission.
For retrospective and post-billing queries:
i) The response to a query (including the physician’s documentation of the condition
or procedure) must be documented in the body of the medical record by the physician
and be signed and dated with the date that the information is added to the medical
record.
ii) The response must be in the form of a late entry progress note, an addendum to a
dictated report (e.g., discharge summary, H&P, consultation), or as an inclusion in the
dictated discharge summary or, at a minimum, the response must be on one of the
approved and required coding query forms.
iii) If the local Quality Improvement Organization (QIO) is requiring the query response to
be documented in the body of the traditional medical record, the response must be in
the form of a late entry progress note, an addendum to a dictated report (e.g., discharge
summary, H&P, consultation), or as an inclusion in the dictated discharge summary.
e. Billing and Delinquent Record Count for a Chart with a Query
i) Any chart awaiting a response to a query must not be final abstracted (final billed)
until the physician’s response is documented on the query form and/or in the body of
the traditional medical record or the physician has responded that no addition to or
clarification of the medical record is necessary.
ii) Any query requiring a physician response must be included in the incomplete and
delinquent record count until the response is received and documented in the
appropriate place in the medical record, or the physician has responded that no
addition to/ clarification of the medical record is necessary. This requirement must
be reflected in the medical staff bylaws or rules and regulations.
f. Medical Staff Approval Process
If medical staff approval is necessary, the Health Information Management (HIM) Director
must submit the standardized query forms for approval following the process outlined in
hospital policy or medical staff bylaws or rules and regulations for adding forms to the
medical record.
g. Query Education and Tracking
i) All facilities should educate their physicians on the importance of concurrent
documentation within the body of the medical record to support complete, accurate
and consistent coding.
ii) Communication should be provided to the medical staff that coders or representatives
4/2005
DEPARTMENT: Health Information
Management Services
PAGE: 7 of 8
EFFECTIVE DATE: April 30, 2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
of HIM and/or Quality Resource Management will query physicians when there are
questions regarding documentation for code assignment.
iii) Communication must clarify that the query will be documented in writing and that the
physician response must be included on the query form and/or, based on QIO
requirements, within the body of the traditional medical record.
iv) Queries must be tracked in order to facilitate improved documentation and
appropriate release of the claim for billing purposes.
v) Administration and medical staff leadership must support this process to ensure its
success.
2. Query Guidelines
In order to achieve consistency in the coding of diagnoses and procedures, coders must:
a. Follow procedures that result in complete, accurate and consistent coding and accurately
represent the patient’s diagnoses and procedures for the relevant episode of care;
b. Adhere to all official coding guidelines as stated in this policy;
c. Assess physician documentation to ensure that it supports the diagnosis and procedure
codes selected;
d. Consult physician for clarification and additional documentation prior to final code
assignment when there is conflicting or ambiguous data in the medical record;
e. Not use the word “possible” in a query unless specified in the physician documentation;
f. Assist and educate physicians and other clinicians by advocating proper documentation
practices, further specificity, resequencing or inclusion of diagnoses or procedures when
needed to more accurately reflect the patient’s episode of care;
g. Follow the procedures as outlined in this policy to document an appropriate query; and
h. Query the physician if the physician has substantially described a clinical condition but has
not made a diagnosis. The query must be documented on the appropriate approved and
required query form attached to this policy.
3. Facility Query Compliance Monitoring
Internal facility-directed (which includes coding supervisors) or certified external vendor
(which excludes Corporate HIMS and Independent Review Organization coding quality
reviews must be completed semi-annually (or more frequently as directed by facility
leadership) by each facility.
a. Reviews must include review of the query process to determine query appropriateness and
accurate code assignment with comparison to the UB-92 claim electronic vendor bill,
and/or remittance advice to determine accurate billing.
b. Findings from these reviews must be utilized to improve the query process, coding and
medical record documentation practices and for coder and physician education, as
appropriate.
4/2005
DEPARTMENT: Health Information
Management Services
PAGE: 8 of 8
EFFECTIVE DATE: April 30, 2005
POLICY DESCRIPTION: Query Documentation
for Inpatient Services
REPLACES POLICY DATED: April 1, 2001;
June 1, 2002; Dec. 15, 2002, May 31, 2004
REFERENCE NUMBER: HIM.COD.012
4. Company-Wide Query Compliance Monitoring
Compliance with this policy will be monitored by the Corporate Health Information
Management Services Department.
a. It is the responsibility of each facility’s administration to ensure that this policy is applied
by all individuals involved in the coding and querying of medical record documentation in
inpatient records.
b. Employees who have questions about a decision based on this policy or wish to discuss an
activity observed related to application of this policy should discuss these situations with
their immediate supervisor to resolve the situation.
c. All day-to-day operational issues should be handled locally; however, if confidential advice
is needed or an employee wishes to report an activity that conflicts with this policy and is
not comfortable speaking with the supervisor, employees may call the toll-free Ethics Line
at 1-800-455-1996.
For any questions regarding this policy, please contact the HIMS P&P Helpline 615-344-6115 or by
the e-mail address: HIMS P&P Helpline.
REFERENCES:
Coding Documentation for Outpatient Services Policy, HIM.COD.002
Coding Documentation for Skilled Nursing Facilities/Units Policy, HIM.COD.010
Coding Documentation for Rehabilitation Facilities Policy, HIM.COD.013
Special Coding Practices on ICD-9-CM Code 482.83 Policy
HCA HIMS Query Handbook (found on ATLAS intranet)
Coding Clinic for ICD-9-CM is the official publication of ICD-9-CM coding guidelines and advice
as designated by four cooperating parties: American Hospital Association (AHA), American
Health Information Management Association (AHIMA), Centers for Medicare and Medicaid
Services (CMS), and the National Center for Health Statistics (NCHS).
Practice Brief on Data Quality, American Health Information Management Association
(AHIMA), Chicago, Illinois, February 1996.
AHIMA Standards of Ethical Coding, American Health Information Management Association
(AHIMA), Chicago, Illinois, Revised December 1999.
Health Information Management Compliance, A Model Program for Healthcare Organizations,
Sue Prophet, Chicago, Illinois, 2000 Edition.
CMS memorandum to the Peer Review Organization entitled “Use of the Physician Query Forms”
dated January 22, 2001.
CMS memorandum to the Peer Review Organizations entitled “Use of Physician Query Form” with
Policy Clarification of Temporary Suspension of January 22, 2001, dated March 21, 2001.
ICD-9-CM Coordination and Maintenance Committee Meeting Minutes, December 6, 2002,
Attachment 1-Sepsis & Septic Shock
4/2005
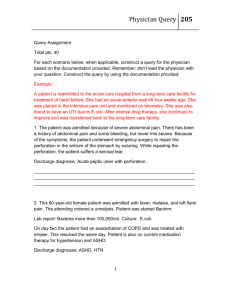
Query Form A – Pneumonia, effective date 04/30/2005
PNEUMONIA
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: _________________________ Coder’s Phone #: _____________________________
Patient Name: ________________________________________________________________
Admit Date: _____________________ Discharge Date: ___________________
MR#:
___________________ Acct #: ______________________________________
The medical record reflects the diagnosis of pneumonia in the (progress notes, dictated report, history and
physical)__________________________________________________________________________
and the sputum culture shows (specify organism identified in the sputum culture(s) ________________
________________________________________________________________________________.
Please respond to the following questions and take the appropriate action based on your response:
Based on the above information, can you identify the specific organism responsible for this
patient’s pneumonia?
If yes, please document the responsible organism in the space below and/or in the medical record (progress
notes, dictated report or as an addendum to a dictated report). If providing your response on this query
form, please sign and date below.
______________________________________
No- [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine – [If so, please initial in or check the box, and sign and date below. This
form will need to be maintained with the medical record. ]
_______________________________
PHYSICIAN SIGNATURE
_________________________
DATE
Attachment to HIM.COD.012
Query Form B – Aspiration Pneumonia, effective date 04/30/2005
ASPIRATION PNEUMONIA
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is
asked does not imply that any particular answer is desired or expected. Thanks in advance for your clarification
on this issue.
Coder’s Name: __________________________ Coder’s Phone #: _____________________________
Patient Name:
____________________________________________________________________
Admit Date: _________________
MR#: ______________
Discharge Date: __________________
Acct #: _______________________
The patient must have extensive clinical indicators of aspiration pneumonia present prior to querying. By
extensive clinical indicators, it is meant that the physician has substantially described the clinical condition about
which the coder will inquire but has not made the specific or particular diagnosis. The medical record
reflects the following clinical findings suggestive of aspiration pneumonia.
Check Here if indicator
is present
Clinical indicator
Location in the medical record which
reflect the clinical findings
Impaired gag reflex
Esophageal disorder (obstruction,
cancer, stenosis, varices)
Dysphagia
Positive swallowing study
Positive Infiltrate on Chest x-ray
Current aspiration and/or recent
vomiting.
Please respond to the following question:
Based on your medical judgement of the clinical indicators outlined above, are
you treating this patient for a known or suspected aspiration
pneumonia?
If yes, please document the specific diagnosis in the space below and/or in the medical record
(progress notes, dictated report or as an addendum to a dictated report). If providing
your response on this query form, please sign and date below.
______________________________________________
No – [If no, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record].
Unable to determine– [If so, please initial in or check the box, and sign and date below.
This form will need to be maintained with the medical record.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form C – Sepsis with Positive Blood Cultures, effective date 04/30/2005
SEPSIS with POSITIVE BLOOD CULTURES
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked
does not imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: _______________________ Coder’s Phone #: ________________________________
Patient Name: ________________________________________________________________
Admit Date: ___________________
Discharge Date: ____________________
MR#: ___________________
Acct #: ___________________
The medical record reflects the diagnosis of sepsis in the (medical record location(s)
___________________________________________________ and the blood culture shows (insert
organism)______________________________________________________________.
Please respond to the following question:
Based on the above information, can you identify the known or suspected specific
organism responsible for this patient’s sepsis?
If yes, please document the responsible organism (if applicable) in the space below and/or in the
medical record (progress notes, dictated report or as an addendum to a dictated report). If
providing your response on this query form, please sign and date below.
_______________________________
No- [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine- [If so, please initial in or check the box, and sign and date below. This
form will need to be maintained with the medical record.]
_______________________________
PHYSICIAN SIGNATURE
_________________________
DATE
Attachment to HIM.COD.012
Query Form D – Generalized Sepsis, effective date 04/30/2005
GENERALIZED SEPSIS
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
XXX-XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked
does not imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: ____________________________Coder’s Phone #: _____________________________
Patient Name:
______________________________________________________________________
Admit Date: ______________________
MR#: __________________
Discharge Date: _________________________
Acct #: __________________________
The physician must have documented a localized or systemic infection and the patient must have extensive clinical
indicators of a generalized sepsis present prior to querying. By extensive clinical indicators, it is meant that the
physician has documented two or more of the clinical indicators outlined below, therefore substantially describing the
clinical condition about which the coder will inquire but not having made the specific or particular diagnosis.
The medical record reflects the following clinical findings suggestive of sepsis.
Check Here if indicator
is present
Clinical indicator
Location in the medical record which
reflect the clinical findings
Fever or hypothermia
Tachypnea
Tachycardia
WBC count > 12,000/mm3 or
<4000/mm3 or 10% immature
neutrophils
Oliguria
Hypotension
Metabolic acidosis (elev lactate level,
anion gap or reduced blood pH)
Acute onset of confusion associated
with disease process/Altered Mental
Status
Shock
Positive Blood Culture - _________
Please respond to the following question:
Based on your medical judgement of the clinical indicators outlined above, are you
treating this patient for a known or suspected generalized sepsis?
If yes, please document the specific diagnosis (and responsible organism, if applicable) in the space
below and/or in the medical record (progress notes, dictated report or as an addendum to a
dictated report). If providing your response on this query form, please sign and date below.
______________________________________
No – [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record].
Unable to determine – [If so, please initial in or check the box, and sign and date below. This
form will need to be maintained with the medical record].
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form E – Urosepsis, effective date 04/30/2005
UROSEPSIS
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
XXX-XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is
asked does not imply that any particular answer is desired or expected. Thanks in advance for your clarification
on this issue.
Coder’s Name: ___________________________ Coder’s Phone #: ____________________________
Patient Name:_________________________________________________________________________
Admit Date:____________________ Discharge Date: ______________________
MR#: __________________________
Acct #:___________________
The physician must have documented urosepsis and the patient must have extensive clinical indicators of a
generalized sepsis present prior to querying. By extensive clinical indicators, it is meant that the physician has
documented two or more of the clinical indicators outlined below, therefore substantially describing the clinical
condition about which the coder will inquire but - not having made the specific or particular diagnosis.
The medical record reflects the following clinical findings:
Check Here if indicator
Clinical indicator
is present
Fever or hypothermia
Tachypnea
Tachycardia
WBC count > 12,000/mm3 or
<4000/mm3 or 10% immature
neutrophils
Oliguria
Hypotension
Metabolic acidosis (elev lactate level,
anion gap or reduced blood pH)
Acute onset of confusion associated
with disease process/Altered Mental
Status
Shock
Positive Blood Culture - _________
Location in the medical record which reflect
the clinical findings
Please respond to the following question:
Official Coding Guidelines maintain that in order to ensure accurate coding practices, the physician should be
asked if the diagnosis of urosepsis with clinical indications of sepsis is intended to mean: (1) generalized sepsis
or (2) urine contaminated by bacteria, bacterial by-products, or other toxic material but without other findings.
When using the terminology of “urosepsis,” do you mean:
Sepsis or a Localized Urinary Tract Infection – [Please document the specific diagnosis {and responsible organism, if
applicable} in the space below and/or in the medical record (progress notes, dictated report or as an
addendum to a dictated report). If providing your response on this query form, please sign and date below.
_____________________________
PHYSICIAN SIGNATURE
________________
DATE
Attachment to HIM.COD.012
Query Form F – General, effective date 04/30/2005
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: ___________________________Coder’s Phone #:_________________________________
Patient Name: _____________________________________________________________________
Admit Date: __________ ___________
Discharge Date: ____________________
MR#: _______________________
Acct #: ___________________
The medical record reflects the following clinical findings (include reference to source document):
Please respond to the following question:
PHYSICIAN RESPONSE:
If yes, please document your response (i.e., condition, procedure, organism) in the space below and/or
in the body of the medical record (progress notes, dictated report or as an addendum to a dictated
report). If providing your response on this query form, please sign and date below.
____________________________________________________________________________________________
____________________________________________________________________________________________
____________________________________________________________________________________________
____________________________________________________________________________________________
No – [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine – If so, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form G - Acute Blood Loss Anemia, effective date 04/30/2005
ACUTE BLOOD LOSS ANEMIA
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
(XXX) XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: ______________________________ Coder’s Phone #: _______________________________
Patient Name:
____________________________________________________________________
Admit Date: ______________________
MR#: ______________________________
Discharge Date: ________________
Acct #: ________________________________
The medical record reflects the following clinical findings suggestive of acute blood loss anemia.
Check Here if indicator
is present
Clinical indicator
Location in the medical record which
reflect the clinical findings
Anemia
Significant drop in H&H
Hypotension
GI Bleed
Transfusion(s)
Acute Bleed – other sites
Tachycardia
Please respond to the following question:
Based on your medical judgment of the clinical indicators outlined above, are you treating
this patient for a known or suspected acute blood loss anemia?
If yes, please document the specific diagnosis in the space below and/or in the medical record (progress notes,
dictated report or as an addendum to a dictated report). If providing your response on this query form,
please sign and date below.
____________________________________________________________________________________________
____________________________________________________________________________________________
____________________________________________________________________________________________
No – [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine – [If so, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form H – Septicemia with Positive Blood Cultures, effective date 04/30/2005
SEPTICEMIA with POSITIVE BLOOD CULTURES
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
XXX-XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: _______________________ Coder’s Phone #: ________________________________
Patient Name: ________________________________________________________________
Admit Date: ___________________
Discharge Date: ____________________
MR#: ___________________
Acct #: ___________________
The medical record reflects the diagnosis of septicemia in the (medical record location(s)
___________________________________________________ and the blood culture shows (insert
organism)______________________________________________________________.
NOTE - Per Coding Clinic guidelines, septicemia is defined as a systemic infection that is more clinically significant
than bacteremia, and requires a link between documented septicemia and a positive blood culture when the positive
blood culture is considered the responsible organism.
Please respond to the following question:
Based on the above information, can you identify the known or suspected specific organism
responsible for this patient’s septicemia?
If yes, please document the specific type of organism that was treated and was responsible for the septicemia in the
space below and/or in the medical record (progress notes, dictated report or an addendum to a dictated report). If
providing your response on this query form, please sign and date below.
______________________________________
No- [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine- [If so, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record.]
_______________________________
PHYSICIAN SIGNATURE
_________________________
DATE
Attachment to HIM.COD.012
Query Form A – Pneumonia, effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
PNEUMONIA
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: _______________________ Coder’s Phone #: _______________________________
Patient Name: ________________________________________________________________
Admit Date: ________________ Discharge Date: _______________________
MR#:
___________________
Acct #: ______________________________________
The medical record reflects the diagnosis of pneumonia in the (progress notes, dictated report, history and
physical)__________________________________________________________________________
and the sputum culture shows (specify organism identified in the sputum culture(s) ________________
________________________________________________________________________________.
Please respond to the following questions and take the appropriate action based on your response:
Based on the above information, can you identify the specific organism responsible for this
patient’s pneumonia?
If yes, then per the QIO guidelines please document the responsible organism in the body of the medical record
(progress notes, dictated report or as an addendum to a dictated report).
No- [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine – [If so, please initial in or check the box, and sign and date below. This
form will need to be maintained with the medical record. ]
_______________________________
PHYSICIAN SIGNATURE
_________________________
DATE
Attachment to HIM.COD.012
Query Form B – Aspiration Pneumonia,
effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
ASPIRATION PNEUMONIA
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
XXX-XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is
asked does not imply that any particular answer is desired or expected. Thanks in advance for your clarification
on this issue.
Coder’s Name: ______________________________ Coder’s Phone #: _________________________
Patient Name:
____________________________________________________________________
Admit Date: ______________________
Discharge Date: ________________
MR#: ______________________________
Acct #: ________________________________
The patient must have extensive clinical indicators of aspiration pneumonia present prior to querying. By
extensive clinical indicators, it is meant that the physician has substantially described the clinical condition about
which the coder will inquire but has not made the specific or particular diagnosis.
The medical record reflects the following clinical findings suggestive of aspiration
pneumonia.
Check Here if indicator
is present
Clinical indicator
Location in the medical record which
reflect the clinical findings
Impaired gag reflex
Esophageal disorder (obstruction,
cancer, stenosis, varices)
Dysphagia
Positive swallowing study
Positive Infiltrate on Chest x-ray
Current aspiration and/or recent
vomiting
Please respond to the following question:
Based on your medical judgement of the clinical indicators outlined above, are you
treating this patient for a known or suspected aspiration pneumonia?
If yes, then per the QIO guidelines please document the specific diagnosis in the body of the medical
record (progress notes, dictated report or as an addendum to a dictated report),
No – [If no, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record].
Unable to determine– [If so, please initial in or check the box, and sign and date below.
This form will need to be maintained with the medical record.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form C – Sepsis with Positive
Blood Cultures, effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
SEPSIS with POSITIVE BLOOD CULTURES
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is
asked does not imply that any particular answer is desired or expected. Thanks in advance for your clarification
on this issue.
Coder’s Name: ___________________________ Coder’s Phone #_____________________________
Patient Name: ________________________________________________________________
Admit Date: ______________________
Discharge Date: _____________
MR#: ________________ ____________ Acct #: _______________________________
The medical record reflects the diagnosis of sepsis in the (medical record location(s)
___________________________________________________ and the blood culture shows (insert
organism)______________________________________________________________.
Please respond to the following question:
Based on the above information, can you identify the known or suspected specific
organism responsible for this patient’s sepsis?
If yes, then per the QIO guidelines please document the specific organism that was treated and was
responsible for the sepsis in the body of the medical record (progress notes, dictated report or as an
addendum to a dictated report).
No- [If no, please initial in or check the box, and sign and date below. This form will need
to be maintained with the medical record.]
Unable to determine- [If so, please initial in or check the box, and sign and date below.
This form will need to be maintained with the medical record.]
_______________________________
PHYSICIAN SIGNATURE
_________________________
DATE
Attachment to HIM.COD.012
Query Form D – Generalized Sepsis, effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
GENERALIZED SEPSIS
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
XXX-XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked
does not imply that any particular answer is desired or expected Thanks in advance for your clarification on this issue.
Coder’s Name: _____________________________Coder’s Phone #: ____________________________
Patient Name:
______________________________________________________________________
Admit Date:___________________
Discharge Date: _______________
MR#:______________________________
Acct #: ___________________
The physician must have documented a localized infection or systemic infection and the patient must have extensive
clinical indicators of a generalized sepsis present prior to querying. By extensive clinical indicators, it is meant that the
physician has documented two or more of the clinical indicators outlined below, therefore substantially describing the
clinical condition about which the coder will inquire but not having made the specific or particular diagnosis.
The medical record reflects the following clinical findings suggestive of sepsis.
Check Here if indicator
is present
Clinical indicator
Location in the medical record which
reflect the clinical findings
Fever or hypothermia
Tachypnea
Tachycardia
WBC count > 12,000/mm3 or
<4000/mm3 or 10% immature
neutrophils
Oliguria
Hypotension
Metabolic acidosis (elev lactate level,
anion gap or reduced blood pH)
Acute onset of confusion associated
with disease process/Altered Mental
Status
Shock
Positive Blood Culture - __________
Please respond to the following question:
Based on your medical judgement of the clinical indicators outlined above, are you treating
this patient for a known or suspected generalized sepsis?
If yes, then per the QIO guidelines please document the specific diagnosis (and responsible organism, if
applicable) in the body of the medical record (progress notes, dictated report or as an addendum to a
dictated report).
No – [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record].
Unable to determine – [If so, please initial in or check the box, and sign and date below. This
form will need to be maintained with the medical record].
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form E – Urosepsis, effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
UROSEPSIS
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
XXX-XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked
does not imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: ____________________________Coder’s Phone :_______________________________
Patient Name:_________________________________________________________________________
Admit Date:________________________
Discharge Date: ________________________
MR#: _________________
Acct #:___________________
The physician must have documented urosepsis and the patient must have extensive clinical indicators of a generalized
sepsis present prior to querying. By extensive clinical indicators, it is meant that the physician has documented two or
more of the clinical indicators outlined below, therefore substantially describing the clinical condition about which the
coder will inquire but not having made the specific or particular diagnosis.
The medical record reflects the following clinical findings:
Check Here if indicator
Clinical indicator
is present
Fever or hypothermia
Tachypnea
Tachycardia
WBC count > 12,000/mm3 or
<4000/mm3 or 10% immature
neutrophils
Oliguria
Hypotension
Metabolic acidosis (elev lactate level,
anion gap or reduced blood pH)
Acute onset of confusion associated
with disease process/Altered Mental
Status
Shock
Positive Blood Culture - ________
Location in the medical record which reflect
the clinical findings
Please respond to the following question:
Official Coding Guidelines maintain that in order to ensure accurate coding practices, the physician should be asked if
the diagnosis of urosepsis with clinical indications of sepsis is intended to mean: (1) generalized sepsis or (2) urine
contaminated by bacteria, bacterial by-products, or other toxic material but without other findings.
When using the terminology of “urosepsis,” do you mean:
_________Sepsis – [If so, please document the specific diagnosis (and responsible organism, if applicable) in the medical record
(progress notes, dictated report or as an addendum to a dictated report) per QIO guidelines.]
________ Localized UTI – [If so, please sign and date below.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form F – General, effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: __________________________Coder’s Phone #:__________________________________
Patient Name: _____________________________________________________________________
Admit Date:___________________
Discharge Date: ____________________
MR#: _______________ Acct #:___________________
The medical record reflects the following clinical findings (include reference to source document):
Please respond to the following question:
PHYSICIAN RESPONSE:
If yes, then per QIO guidelines please document your response (i.e., condition, procedure, organism), in
the body of the medical record (progress notes, dictated report or as an addendum to a dictated report).
No – [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine – If so, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form G – Acute Blood Loss Anemia, effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record.
ACUTE BLOOD LOSS ANEMIA
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Please return this form by fax to:
(XXX) XXX-XXXX
Dear Dr. ____________________________:
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: ______________________________ Coder’s Phone #: _______________________________
Patient Name:
____________________________________________________________________
Admit Date: ______________________
Discharge Date: ________________
MR#: ______________________________
Acct #: ________________________________
The medical record reflects the following clinical findings suggestive of acute blood loss anemia.
Check Here if indicator
is present
Clinical indicator
Location in the medical record which
reflect the clinical findings
Anemia
Significant drop in H&H
Hypotension
GI Bleed
Transfusion(s)
Acute Bleed – other sites
Tachycardia
Please respond to the following question:
Based on your medical judgment of the clinical indicators outlined above, are you treating this
patient for a known or suspected acute blood loss anemia?
If yes, then per the QIO guidelines please document the specific diagnosis in the body of the medical record (progress
notes, dictated report or as an addendum to a dictated report).
No – [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record].
Unable to determine– [If so, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record.]
____________________________
PHYSICIAN SIGNATURE
______________________
DATE
Attachment to HIM.COD.012
Query Form H – Septicemia with Positive Blood Cultures,
effective date 04/30/2005
For use when the facility’s QIO requires physician
documentation in the body of the traditional medical record
SEPTICEMIA with POSITIVE BLOOD CULTURES
PHYSICIAN QUERY FORM
THIS FORM IS A PERMANENT PART OF THE MEDICAL RECORD
Date: _______________________________
Dear Dr. ____________________________:
Please return this form by fax to:
XXX-XXX-XXXX
In responding to this query, please exercise your independent professional judgment. The fact that a question is asked does not
imply that any particular answer is desired or expected. Thanks in advance for your clarification on this issue.
Coder’s Name: ___________________________ Coder’s Phone #_____________________________
Patient Name: ________________________________________________________________
Admit Date: ______________________
Discharge Date: _____________
MR#: ________________ ____________ Acct #: _______________________________
The medical record reflects the diagnosis of septicemia in the (medical record location(s)
___________________________________________________ and the blood culture shows (insert
organism)______________________________________________________________.
NOTE - Per Coding Clinic guidelines, septicemia is defined as a systemic infection that is more clinically significant
than bacteremia, and requires a link between documented septicemia and a positive blood culture when the positive blood
culture is considered the responsible organism.
Please respond to the following question:
Based on the above information, can you identify the known or suspected specific organism
responsible for this patient’s septicemia?
If yes, then per the QIO guidelines please document the specific organism that was treated and was responsible for the
septicemia in the body of the medical record (progress notes, dictated report or as an addendum to a dictated report).
No- [If no, please initial in or check the box, and sign and date below. This form will need to be
maintained with the medical record.]
Unable to determine- [If so, please initial in or check the box, and sign and date below. This form will
need to be maintained with the medical record.]
_______________________________
PHYSICIAN SIGNATURE
_________________________
DATE
Attachment to HIM.COD.012