File - Wk 1-2
advertisement

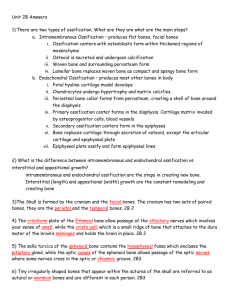
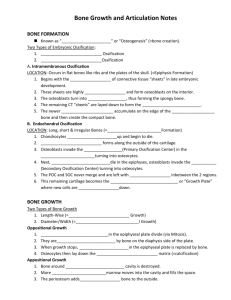
Development of the Musculoskeletal System 1. Describe the process of bone ossification and of the growth, development, maturation and common development variations of the lower limb 2. Outline the progressive development of ossification centres with age Ossification = osteogenesis = the process of bone formation In embryos, ossification leads to formation of the bony skeleton. Later bone growth enables the body to continue to increase in size, goes on until early adulthood. Ossification in adults is mainly for remodeling and repair. Formation of the bony skeleton Before wk 8, the skeleton of the embryo is fibrous membrane and hyaline cartilage. Then after this, bone tissue begins to develop. Bones that develops from fibrous membrane is involved in transmembranous ossification and the bone is called membrane bone. Bone development that replaces hyaline cartilage is called endochondral ossification. Intramembranous ossification Results in the formation of the skull and the clavicles. All bones become flat bones. This is a four step process: 1. 2. 3. 4. Ossification centre appears in the fibrous connective tissue membrane Bone matrix (osteoid) secreted within the fibrous membrane Woven bone and periosteum form Bone collar of compact bone forms and red marrow appears Endochondral Ossification Except for the clavicles, all bones below the base of the skull form by endochondral ossification. The process begins in the 2nd month of development. Uses the hyaline cartilage formed earlier as models or patterns for bone construction. It is a complex process (more than intramembranous ossification) because hyaline cartilage needs to be broken down as ossification proceeds. a. The formation of a long bone begins in the centre of the hyaline cartilage shaft at a region called the primary ossification centre b. The perichondrium covering the hyaline cartilage is infiltrated with blood vessels and converts it to vascularised periosteum c. Due to an increase in nutrients, the underlying mesenchymal cells specialize into osteoblasts. Now ossification can begin. Steps in Ossification: 1. Bone collar forms around the diaphysis of the hyaline cartilage model a. Osteoblasts of the periosteum secrete osteoid against hyaline cartilage, encasing it in a bone collar 2. Cartilage in the centre of the diaphysis calcifies then cavitates a. Chondrocytes in the shaft enlarge and signal surrounding cartilage matrix to calcify. Calcified matrix is impermeable to diffusing nutrients so chondrocytes die and the matrix begins to deteriorate, opening up cavities. However the hyaline cartilage model is still stabilsed by the bone collar. The cartilage continues to grow elsewhere because it is still healthy so the bone continues to elongate. 3. The periosteal bud invades the internal cavities and spongy bone is formed a. Happens in month 3. The cavities are invaded by periosteal bud consisting of nutrient artery, vein, lymphatics, nerve fibres, red marrow elements, osteoblasts and osteoclasts. Osteoclasts partially erode the calcified matrix and the osteoblasts secrete osteoid around fragments of hyaline cartilage forming bone covered cartilage trabeculae. 4. The diaphysis elongates and a medullary cavity forms a. The primary ossification centre enlarges, osteoclasts breakdown the newly formed spongy bone and opens up a medullary cavity in the centre of the diaphysis b. Throughout the foetal period the epiphyses are entirely cartilage. This enables the hyaline cartilage model to continue to elongate by division of viable cartilage cells. c. Cartilage is calcifying, being eroded and then replaced by bony spicules on the epiphyseal surfaces facing the medullary cavity; ossification follows cartilage formation along the length of the shaft. 5. Ossification of epiphyses a. Shortly before or after birth secondary ossification centres appear in one or both epiphyses and they gain bony tissue. The large long bones form secondary ossification centres in both epiphyses, small long bones form only one secondary ossification centre. b. The cartilage in the centre of the epiphyses calcifies and deteriorates, making cavities where a perosteal bud can entre. Bony trabeculae appear. c. Secondary ossification reproduce the same events as primary ossification except: i. Spongy bone in interior is retained ii. No medullary cavity forms d. When secondary ossification is complete, hyaline cartilage exists only in 2 places: i) epiphyseal surfaces (articular cartilages) ii) epiphyseal plates. Postnatal Bone Growth During infancy and youth, long bones lengthen by interstitial growth of the epiphyseal plates (growth from within the bone) All bones grow in thickness by appositional growth (growth from outside). Most bones stop growing in adolescence however bones of the nose and lower jaw continue to grow throughout life. Growth in length of long bones – mimics endochondral ossification. Epiphyseal plate side facing epiphysis, the cartilage is quiescent (inactive). Epiphyseal plate side facing diaphysis, the cartilage is organized into a pattern that allows fast, efficient growth. Here the cartilage cells form tall columns like a stack of coins. The cells at the top of the stack (facing epiphysis) divide quickly, pushing the epiphysis away from the diaphysis, causing lengthening (growth zone). The chondrocytes closer to the diaphysis (transformation zone) hypertrophy, lucanae erode and enlarge therefore the surrounding cartilage matrix calcifies, these chondrocytes die and deteriorate. This leaves long spicules of calcified cartilage at the epiphyseal-diaphyseal junction. This now becomes part of the osteogenic zone which is invaded by marrow elements from the medullary cavity. The cartilage spicules are partly eroded by osteoclasts but quickly recovered by osteoblasts, forming spongy bone. During growth the epiphyseal plate maintains a constant thickness because the rate of cartilage growth is balanced by replacement of bony tissue. As adolescence ends, the chondroblasts of the epiphyseal plate divide less and less, the plate becomes thinner until eventually they are replaced entirely by bone tissue. Longitudinal bone growth ends when bone of the epiphysis and diaphysis fuse = epiphyseal plate closure. Happens at 18yo for female, 21 yo for males. Adult bones can still increase in diameter and thickness via apposition growth if stressed by excessive muscle activity or weight. Bone Homeostasis: Remodelling and Repair Every week we recycle 5-7% of our bone mass and as much as ½ g of calcium may enter or leave the adult skeleton each day. Spongy bone is replaced every 3-4years. Compact bone is replaced every 10 years. When bone remains in place for long periods, the calcium crystallizes and becomes brittle, easily leading to fractures. Bone remodeling This is bone deposition and bone resorption at the surface of the periosteum and the surface of the endosteum. This is regulated by osteoblasts and osteoclasts. In healthy people (young adults in particular), total bone mass remains constant, suggesting that bone deposition and resorption are equal. Remodelling does not occur uniformally. E.g. distal part of the femur is replaced fully every 5-6mths where as the shaft is replaced much more slowly. Bone deposit occurs where bone is injured or added bone strength is required. Optimal bone deposit requires a diet rich in proteins, Vit C, D, A and minerals (Calcium, phosphate, magnesium, manganese). New bone matrix deposits by osteocytes is marked by the presence of osteoid seams – an unmineralised band of bone matrix. Between the osteoid seam and the older mineralized bone there is an abrupt transition called the calcification front. It appears that osteoid needs to mature for about 1wk before it can calcify. It is unknown what triggers this calcification. However it is influenced by the local concentration of calcium and phosphate ions. When these products reach a certain level, they catalyse further crystallization of calcium salts in the area. Other factors include matrix proteins that bind and concentrate calcium and the enzyme alkaline phosphatase (shed by osteoblasts) – essential for mineralization. Bone resorption involves osteoclasts which arise from the same haematopoietic stem cells that differentiate into macrophages. Osteoclasts move along a bone surface, digging grooves called resorption bays as they break down the matrix. The part of the osteoclast that touches the bone is highly folded to form a ruffled membrane enabling it to cling to the bone tightly and also seals off the area of bone destruction. The ruffled membrane secrets: i) lysosomal enzymes (digest organic matrix) ii) hydrochloric acid that converts calcium salts into soluble forms that pass easily into solution. Osteoclasts may also phagocytise the demineralised matrix and dead osteocytes. The digested matrix end products and dissolved minerals are transported across the osteoclast and released at the opposite side where they enter interstitial fluid and then the blood. How are osteoclasts activated? It is unclear however T-cells are important. Control of Remodelling 1. Negative feedback hormonal mechanism that maintains Ca²⁺ homeostasis in the blood 2. Responses to mechanical and gravitational forces acting on the skeleton. Calcium is important for Transmission of nerve impulses Muscle contraction Blood coagulation Secretion by glands and nerve cells Cell division More than 99% of the body’s calcium is present in bone minerals. The hormonal loop maintains blood Ca²⁺ within the range of 9-11mg per 100ml of blood. Calcium requirements: 400-800mg from birth – 10 years old 1200-1500mg from 11-24 years old. Hypercalcemia can lead to undesirable deposits of calcium in the blood vessels, kidneys and other soft organs, impairing their function. Response to Mechanical Stress The bone’s response to mechanical stress (muscle pull) and gravity keeps the bones strong where stressors are acting. Wolff’s law – a bone grows or remodels in response to the demands placed on it. Bones have different stressors e.g. weight bearing, pulling, and compression. This tension (load) usually bends it – compressing on one side, stretching on the other and these forces cancel each other out at the centre, so that’s why bones can have a hollow centre. Bones are thickest midway along the diaphysis Curved bones are thickest where they are likely to buckle Trabeculae of spongy bone form trusses or struts along lines of compression Large bony projections occur where heavy, active muscles attach. Bedridden people have atrophied bones due to disuse. The mechanism of how bone responds to mechanical stimuli is largely unknown. Deforming a bone produces as electrical current. Stretch regions are oppositely charged. Hormonal loop determines whether and when remodeling occurs (in response to changing Ca²⁺ blood levels). Mechanical stress determines where it occurs. Common development variations of the lower limbs Bow legs (Genu Varum) – common up to 2yo. Bowing at the tibia, usually goes away. If there is bowing in only one leg, should investigate. Knock knees (Genu Valgum or a Valgus deformity) – affects children between 2-7yo. Usually corrects itself by 7yo. No treatment really necessary. Obese children over 12yo may require treatment. Rolling in of the ankles – due to joint laxity. No treatment necessary as it usually corrects itself. Flat feet – normal for younger age because children have low arches and loose and flexible joints. Common in preschoolers. Present in <10% of teenagers Accessory navicular bone – temporary discomfort, relived by wearing arch supports for a period of a year or two. Rarely requires surgery to remove. Curly middle toe – third toe curls inwards under the 2nd toe. This is acceptable until 2 years of age. In toe gait (pigeon toe) is common. Caused by inset hips, internal torsion of the tibia and metatarsus adductus.