Adult & Pediatric Allergist of Central Jersey
advertisement

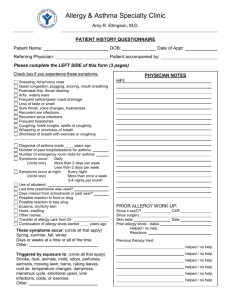
Practice Logo Dr. A. Best Anywhere, USA Phone, Email, Fax Initial Visit Name: DOB: Age: Sex Male/ Female Date: Patient: Usual Physician: Referred by: CC: THE MAIN PROBLEMS FOR COMING HERE ARE: Yes/No Itchy or watery eyesNasal Congestion or runny noseSneezingSnoring or breathing thought the mouthDrainage down the throatFrequent yellow or green nasal drainageDo you have asthma?Diagnosis of asthma made ____ yrs agoCoughingWheezing or shortness of breathNumber nights wheezing/ coughing per week___ Number nights wheezing/coughing per month___ Number of past hospitalizations for asthma___ Number of past emergency visits for asthma___ Days of school or work missed in past year___ Possible reaction to food or drug___ Bee sting reactionsRashesFrequent infectionsNumber of ear infections in the past year___ Number of sinus infections in the past year___ Number of pneumonias during lifetime___ HeadachesVomiting/DiarrheaAbdominal PainOther (explain)THESE SYMPTOMS OCCUR: Spring [ ] Summer [ ] Fall [ ] Winter [ ] Days or weeks at a time [ ] All the time? [ ] At home [ ] Which room? ________________ ______________________________ Physician Notes: ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ SYMPTOMS GET WORSE OR IMPROVE Outdoors [ ] Indoors [ ] At work or school [ ] All day [ ] Night or morning [ ] Patient’s Name: ________________________________________ SYMPTOMS ARE MADE WORSE BY: [ [ [ [ [ [ [ ] Colds/Infection [ ] Cigarette smoke [ ] Mowing grass [ ] Raking leaves [ ] Perfumes or scents [ ] Dusting or cleaning [ ] Food [ ] Cats/Dogs ] Weather changes ] Windy days ] Damp areas ] Heat ] Cold ] Other ALL CURRENT MEDICINES number mg, tab, caps, or inhaler puffs ___________________________________ ___________ ________ Times per day ___________________________________ ___________ ________ Times per day ___________________________________ ___________ ________ Times per day ___________________________________ ___________ ________ Times per day ___________________________________ ___________ ________ Times per day PREVIOUS ALLERGY OR ASTHMA MEDICATIONS(INCL. OTC): ____________________ [ ] helped [ ] no help [ ] drowsy [ ] jittery ____________________ [ ] helped [ ] no help [ ] drowsy [ ] jittery ____________________ [ ] helped [ ] no help [ ] drowsy [ ] jittery CURRENT ENVIRONMENT (X IF PRESENT): Home/Apt ______________ Length of occupancy ____________ How old is the building? ________ Yrs Yes/No Yes/No Cats Baseboard Heat Forced air heat Dogs Birds Air conditioning Humidifier Other pets Lots of houseplants Feather pillows Damp baseball Down comforter Mold growth Carpets or rugs Roaches Air cleaner Cigarette smoke Improvements on trips PAST ALLERGY HISTORY: (Use space at right if needed) Yes/No Previous allergy testing? If yes then answer the questions below: Testing done by Dr. ____________ in 19 __ Previous allergy shots Still on allergy shots Shots are received every ____ week now Allergy shots helped Only minor reaction with the shots If major reactions then explain: ______________________________________ ______________________________________ ______________________________________ ______________________________________ PAST MEDICAL HISTORY Hospitilizations: Age or Year ____ for ________________________________ ____ for ________________________________ ____ for ________________________________ Surgeries: ____ for ________________________________ ____ for ________________________________ ____ for ________________________________ Emergency Visits: ____ Times in past year ____ Times in past five years Drug Allergies: Symptoms: _________________Caused_______________________________ _________________Caused_______________________________ _________________Caused_______________________________ Immunizations up to date for the age: Y[ ] N [ ] Immunization Adverse Reactions: _________________Caused_______________________________ Other Chronic Health Conditions: Age or Year ___________________________Since______ ___________________________Since______ ___________________________Since______ Notes: Family History ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ Allergies Asthma Freq. coughing Freq. Infections Father Mother Brother(s) Sister(s) Grandfather(s) Grandmother(s) Uncle(s) Aunt(s) Cousin(s) Other chronic conditions such as cystic fibrosis, emphysema, recurrent hives or swelling, lupus, rheumatoid arthritis, etc.; ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ Patient’s Name: ________________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ ______________________________________ Social History Primary Residence for the patient is: [ ] [ ] One Home Split between homes Current occupation is: ________________________________ Occupational exposures: ______________________________ __________________________________________________ Smoking: Y [ ] N [ ] If yes, years____ packs/day____ Use of Recreational Drugs Smoked_______ Intranasal_______ Other________ Drink Alcohol? Y [ ] N [ ] Number of drinks per day_____ Other relevant social factors:___________________________ __________________________________________________ Review of Systems: (check if present) Fever Weight loss Skin problems besides eczema Joint swelling or pain Blood count problems (anemia, ect.) Eye problems Throat infections Heart problems, high blood pressure or palpitation Stomach upset Urinary or bladder problems Nerve or psychiatric problems Hormone problems (such as hot flashes, etc.) Other Comments: _____________________________________________________________________________________________ _____________________________________________________________________________________________ Name of person filling out this history form (please print): _____________________________________________ Relationship if not the patient: ___________________________________________________________________