Chest Pain
advertisement

Chest Pain
Chest pain is a common symptom, accounting for about 1% GP visits, 5% A&E department visits and
40% emergency hospital admissions.1
The cause of chest pain is rarely certain, but clues can be taken from the history - cardiac pain is often
heavy, pressing and tight, pleuritic pain is likely to be worse with breathing whilst musculoskeletal pain is
usually a diagnosis of exclusion. Risk factors should be used to help prioritize and guide investigations.
Risk factors
Cause of chest pain
Risk factors
Age >40
IHD
Male or postmenopausal female
Hypertension
Cigarette smoking
Hypercholesterolaemia
Diabetes mellitus
Ethnicity
Truncal obesity
Family history
Sedentary lifestyle
Cocaine use
PE
Immobilization
Recent surgery
History of DVT or PE
Pregnancy
Oestrogen therapy (OCP / HRT)
Pro-thrombotic tendency and
hypercoagulable states
Trauma (especially lower
extremity, pelvis)
Obesity
Malignancy
Aortic dissection
Atherosclerosis
Uncontrolled hypertension
Coarctation of the aorta
Valvular disease
Marfan syndrome
Ehlers-Danlos syndrome
Pregnancy
Smoking
Pneumothorax
Tall/thin stature
Young (20-40 years) males
Trauma
Chronic lung diseases (COPD,
asthma, CF)
Lung cancer
Marfan syndrome
Infection
AIDS
Drug use
Transthoracic medical procedures
Presentation
Initial assessment
General appearance/status:
o Confused
o Highly anxious
o Short of breath
o In severe pain and distress
o Pale or sweaty
o Vomiting
ABC & vital signs - if any of the following are present in conjunction with chest pain, treat as an
emergency and arrange urgent transfer to hospital:4
o Respiratory rate is <10 or >29/min
o O2 sats<93%
o Pulse<50 or >120/min
o Systolic BP<90 mmHg
o Glasgow coma score<12
The aim is to exclude a life-threatening cause which needs immediate treatment from other causes of
chest pain.
Where a patient telephones acutely unwell with chest pain and a cardiac cause is suspected
or the cause is not clear, arrange a 999 ambulance in advance of, or instead of, visiting, as
time to treatment is critical for survival and subsequent myocardial function and should not be
delayed. (The exception is in remote regions where pre-hospital thrombolysis is sometimes
administered by GPs.)
History
Pain:
o
o
o
o
o
o
Site
Radiation
Nature (type, freq, severity)
Onset
Duration
Variation with time
o
o
Modifying factors e.g. exercise, rest, eating, breathing or medication
Previous episodes
Visceral chest pain originates from deep thoracic structures (heart, blood vessels,
oesophagus) and is often (but not always) described as dull, heavy or aching in nature. It is
transmitted via the autonomic system but may be referred via an adjacent somatic nerve
e.g. referred cardiac pain felt in the jaw or left arm. Somatic chest pain arises in the chest
wall, pericardium and parietal pleura and is characteristically sharp in nature and more
easily localised (usually dermatomal).
Associated symptoms:
o Anorexia
o Nausea
o Vomiting
o Breathlessness
o Excessive sweating (diaphoresis)
o Cough
o Haemoptysis
o Palpitations
o Dizziness
o Syncope
Risk factors for IHD and other causes of chest pain
Recent trauma
Past medical history
Current medications
Previous ECGs for comparison and any prior cardiac investigations (where available)
Exclude thrombolysis contraindications if AMI suspected
Screen for panic disorder:
o "In the past 6 months, did you ever have a spell or an attack when you suddenly
felt anxious or frightened or very uneasy?"
o "In the past 6 months, did you ever have a spell or an attack when for no
apparent reason your heart suddenly began to race, you felt faint or couldn't
catch your breath?"
A positive screen ('yes' to either question) is highly sensitive for panic disorder but should
not preclude cardiac testing in patients with risk factors.5
Examination
Vital signs including BP both arms
Detailed cardiovascular & respiratory examinations looking particularly for signs of cardiac
failure or dysrhythmia
Chest wall looking for localised tenderness and evidence of trauma
Also examine the abdomen (possible GI cause), legs (oedema or possible DVT) and skin
(rash)
Differential diagnosis
Cardiac:
o
o
o
o
o
o
o
IHD - AMI, angina (stable/unstable)
Arrhythmias
Aortic dissection
Aortic stenosis / Mitral valve disease
Pericarditis
Vasospasm secondary to illicit drug use
HOCM
Respiratory:
o
o
o
o
Pneumothorax (tension or otherwise)
PE
Pneumonia
Pleurisy
Chest wall / Musculoskeletal:
o Costochondritis
o Rib pain
o Non-specific musculoskeletal pain
o Bone metastases
o Radicular pain
o Breast disease
Gastrointestinal:
o Oesophageal rupture
o Oesophageal spasm
o Peptic ulcer disease
o Cholecystitis
o Pancreatitis
o Gastrooesophageal reflux / Gastritis
Neurogenic:
o Herpes zoster
o Psychological e.g. panic disorder
Others:
o Sickle cell crisis
o Diabetic mononeuritis
o Tabes dorsalis
Investigations
Within primary care, non-acute chest pain:
FBC (to exclude anaemia)
U&Es and creatinine
TFTs
Creatinine kinase
CRP
Fasting lipids and glucose
Resting ECG (note, a resting ECG is normal in over 90% patients with recent symptoms of
angina.6 If an urgent ECG is considered necessary on clinical grounds, admission to hospital
is usually required.)
Additional tests if non-cardiac cause suspected e.g. CXR, LFT and amylase, abdominal
ultrasound
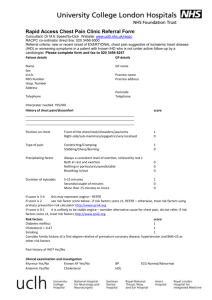
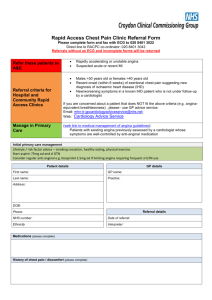
Referral to a rapid access chest pain clinic is now usual for exercise ECG and review
With acute chest pain, in a hospital setting:
Bloods:
o
o
o
o
o
FBC
U&E and creatinine
LFT and amylase
Coagulation screen
Serial myocardial markers7 - Troponin I or T (Creatinine kinase is much less
commonly used now)
Serial ECG
CXR
Second line investigations, as indicated, include:
Echocardiography
CT
V/Q scan
Coronary or pulmonary angiography
Exercise testing
Myocardial perfusion scan
Management
Management will be dependent on diagnosis:
1.
Is this an emergency? Resuscitate and admit as an emergency:
o
o
o
o
o
o
2.
3.
Summon help, arrange 999 ambulance
High flow O2via face mask
IV access
Analgesia
Cardiac monitoring (when available)
Specific therapy according to diagnosis
Is this cardiac chest pain?
o
Is it suggestive of an acute MI or ACS? If so, arrange urgent admission to
hospital or prehospital treatment where provision exists.
o
If the chest pain is suggestive of stable angina, arrange referral for exercise
tolerance testing and investigate/treat risk factors.
Is this non-cardiac chest pain?
o
If the patient is acutely unwell or a life-threatening cause (e.g. PE,
pneumothorax) is suspected, arrange emergency transfer to hospital.
o
o
Has a cardiac cause been satisfactorily excluded?
What is the diagnosis? Uncertainty is high in patients where they are told they
do not have cardiac chest pain but feel no satisfactory diagnosis is given in its
place. Often investigation beyond this point is limited and treatment of noncardiac chest pain patchy. GORD has the highest prevalence as cause of noncardiac chest pain, and some advocate the empirical trial of a PPI or endoscopy
as a legitimate next step.2 Psychological treatment may also be helpful with
some patients.8
Pitfalls
Diagnosis of chest pain is difficult:
Clinical features may not be as reliable as we hope in the diagnosis of acute, undifferentiated
chest pain. For example, the site and nature of pain, the presence of nausea and vomiting
and diaphoresis were not found to be predictive of ACS in one study. 9
ACS is often atypical (without chest pain). There is some evidence to suggest that this occurs
more frequently in women,10 particularly premenopausal women.11
More than one cause may exist.
A perennial problem for frontline doctors is the exclusion of IHD. Remember that a normal
resting ECG does not exclude ACS or IHD.
Response to nitrates or antacids does not prove diagnosis, as angina and GORD may
appear to be relieved by both. ACS pain can be intermittent and appear to 'settle', providing
false reassurance. If in doubt as to whether a patient's chest pain could represent AMI or
unstable angina, admit as further monitoring and investigation (serial ECGs and cardiac
enzymes) is required.