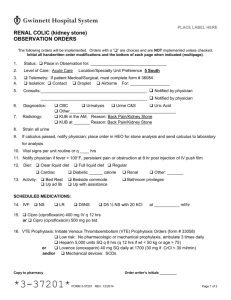
(DVT) and Pulmonary Embolism (PE) Treatment Orders
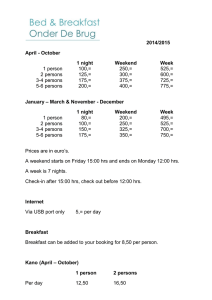
advertisement

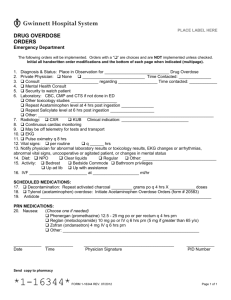
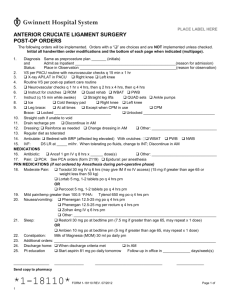
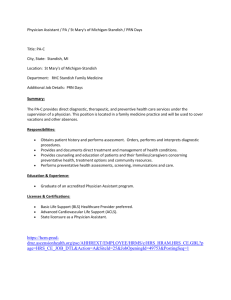
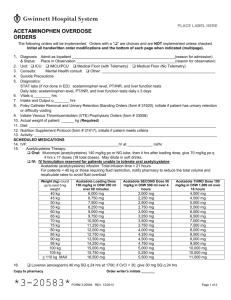
PLACE LABEL HERE DEEP VEIN THROMBOSIS (DVT) and PULMONARY EMBOLISM (PE) TREATMENT ORDERS The following orders will be implemented. Orders with a “” are choices and are NOT implemented unless checked. Initial all handwritten order modifications and the bottom of each page when indicated (multipage). 1. Is this a CMS inpatient only procedure? Yes, admit as inpatient, proceed to # 3 No, proceed to # 2 2. Do you expect that the patient’s condition will require a hospital stay that will cross two midnights (includes the time spent in outpatient- ED, surgery, OBS) and the patient has medical necessity for an inpatient admission? Yes, admit as inpatient, proceed to # 3 No, place in observation 3. If admitted as inpatient, Inpatient Physician Certification: Diagnosis: ________________________________________________________________________________ Level of Care: Critical Intermediate Acute Care Location/Specialty Unit Preference___________ 4. Telemetry: If patient Medical/Surgical, must complete form # 36084 5. Isolation: Contact Droplet Airborne For: _________________ 6. Consult with: Nurse: Instruct patient about subcutaneous self injections Coumadin (warfarin) teaching if patient on warfarin Social Services consult: Outpatient anticoagulation therapy and monitoring 7. Diagnostics, if not done in ED: EKG, Reason: suspected DVT/PE, Read by: __________________ PA/lat CXR, Reason: suspected DVT/PE Portable CXR, Reason: suspected DVT/PE ECHO Reason: suspected DVT/PE, Read by: __________________ TTE TEE 8. Labs, if not done in ED: On admission: CBC, CMP, PT/PTT, UA BNP Troponin CBC q 3 days while receiving Heparin or Lovenox (enoxaparin) PT/INR now (baseline), then daily while receiving Coumadin (warfarin) 9. Vital signs: q 8 hrs q ______ hrs 10. Intake and output: q 8 hrs q ______ hrs 11. O2 per Protocol (form # 34431) 12. Diet: NPO Regular Cardiac Diabetic ______ calorie Renal Other: ___________ 13. Activity: Bedrest Bathroom privileges Out of bed to chair Up ad lib Other: ___________ 14. Foley Catheter Removal and Voiding Assessment/Interventions Standing Orders (form # 31620) 15. Oral Nutrition Supplement Standing Order (form # 31417), initiate if patient meets criteria SCHEDULED MEDICATIONS 16. IVF: ______________________________________________________________________________ 17. Pulmonary Embolism: No contraindications to Tissue Plasminogen Activator (Activase), listed on back of this order. Tissue Plasminogen Activator (Activase) 100 mg IV over 2 hrs. Thrombolytic therapy is a consideration in patients with syncope, hypoxemia/respiratory failure, or hemodynamic instability. Avoid IM injections and arterial punctures if possible. Every 1 hr neurochecks x 24 hrs post Activase administration Hold anticoagulant therapy if Tissue Plasminogen Activator (Activase) is to be given Check PTT after Tissue Plasminogen Activator (Activase) has infused and q 4 hrs thereafter Start Heparin Infusion when PTT is < 76 Heparin Infusion Protocol: HIGH Intensity, NO initial Bolus (form # 28554) Order writer’s Initials _______ *4-1181* 2 FORM 4-1181 REV. 11/2015 WHITE: Medical Record CANARY: Pharmacy Page 1 of PLACE LABEL HERE DEEP VEIN THROMBOSIS (DVT) and PULMONARY EMBOLISM (PE) TREATMENT ORDERS OR See next page for Anticoagulation order options Order writer’s Initials _______ *4-1181* 2 FORM 4-1181 REV. 11/2015 WHITE: Medical Record CANARY: Pharmacy Page 2 of DEEP VEIN THROMBOSIS (DVT) and PULMONARY EMBOLISM (PE) TREATMENT ORDERS Reference Page CONTRAINDICATION TO THROMBOLYTICS *Physician to use professional judgment 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Age less than 18 years.* Active internal bleeding. Known bleeding abnormalities, including but not limited to: Platelet count less than 100,000 Administration of heparin within 48 hours and has an elevated PTT Current/recent use of oral anticoagulants, INR greater than 1.5 Major surgery within 14 days. Intracranial surgery, serious head trauma, or recent previous stroke within 3 months. Recent arterial puncture at a noncompressible site.* Uncontrolled hypertension at time of treatment (greater than 185mm Hg systolic and/or greater than 110 mmHg diastolic). History of intracranial hemorrhage or known AVM, aneurysm, or intracranial neoplasm.* Patients at risk for left heart thrombus, acute pericarditis, or subacute bacterial endocarditis.* Diabetic hemorrhagic retinopathy or other hemorrhagic ophthalmic conditions.* Pregnancy* FORM 4-1181 REV. 11/2015 REFERENCE PAGE PLACE LABEL HERE DEEP VEIN THROMBOSIS (DVT) and PULMONARY EMBOLISM (PE) TREATMENT ORDERS The following orders will be implemented. Orders with a “” are choices and are NOT implemented unless checked. Initial all handwritten order modifications and the bottom of each page when indicated (multipage). 18. Anticoagulant therapy: Patient weight __________ kg Lovenox (enoxaparin), round dose to nearest syringe size, max 180 mg. 1 mg/kg SQ q 12 hrs, CrCl < 30, 1 mg/kg q 24 hrs 1.5 mg/kg SQ q 24 hrs, CrCl < 30, 1 mg/kg q 24 hrs or Heparin infusion Protocol, High intensity, (form # 28554) No initial bolus and Coumadin (warfarin): _____ mg po daily, beginning on ____ Requires 5 day overlap with parenteral anticoagulation and INR > 2.0. 19. Anticoagualtion using only oral agents (do not use with parenteral anticoagulation) Eliquis (apixaban) 10 mg po bid x 7 days, then 5 mg po BID. DC Eliquis if CrCl < 30 ml/min and contact physician for new order. DO NOT use concurrently with other anticoagulants, DC Coumadin (warfarin), Lovenox, Heparin if ordered. or Xarelto (rivaroxaban) 15 mg po BID. DC Xarelto if CrCl < 30 ml/min and contact physician for new order. DO NOT use concurrently with other anticoagulants, DC Coumadin (warfarin), Lovenox, Heparin if ordered. PRN MEDICATIONS (See policy 520-06 for range orders and pain intensity guidelines) 20. Electrolyte Replacement Protocol (form # 21340) 21. Mild Pain, Temp >100.5F, HA: Tylenol (acetaminophen) 650 mg po or PR q 4 hrs prn 22. Moderate Pain: Norco (HYDROcodone/acetaminophen) 5/325 mg or 10/325 mg 1 tab po q 4 hrs prn. DC if Percocet ordered. or If patient cannot take tablet, Hycet elixir (HYDROcodone/acetaminophen 7.5/325 mg/15 ml) 15 ml po q 4 hrs prn instead of Norco. DC if Percocet ordered. or Percocet (oxyCODONE/acetaminophen) 5/325 mg or 10/325 mg 1 tab po q 4 hrs prn. DC if Norco ordered. and/or Toradol (ketorolac) 30 mg IV (or IM if no IV access) q 6 hrs prn (15 mg if CrCl 31-50, > 65 y/o old or < 50 kg) or 10 mg po q 6 hrs prn (max combined duration of IV and po ketorolac is 5 days). DC if CrCl < 30. 23. Severe Pain (Begin when Epidural or PCA has been discontinued) Morphine 1-2 mg IV q 3 hrs prn, DC if CrCl < 30. Hold for excessive sedation. DC if Dilaudid ordered. or Dilaudid (HYDROmorphone) 0.25-0.5 mg IV q 3 hrs prn. If CrCl < 30, dose at 0.25 mg. Hold for excessive sedation. DC if Morphine ordered. 24. Nausea/Vomiting: Zofran (ondansetron) 4 mg IV or po q 6 hrs prn If N/V persists, add Reglan (metoclopramide) 10 mg IV q 6 hrs prn (5 mg if > 65 y/o) 25. Sleep: Ambien (zolpidem) 5 mg (female or males ≥ 65 y/o) or 5-10 mg (male < 65 y/o) po at HS prn 26. Indigestion: Maalox XS (aluminum/magnesium/simethicone) 30 ml po four times daily prn 27. Stool Softener: Colace (docusate) 100 mg po bid prn; if patient has not had a bowel movement 28. Constipation: Milk of Magnesia (MOM) 30 ml po daily prn If no BM after 48 hrs, Dulcolax (biscodyl) 10 mg per rectum daily prn and/or Senokot-S (docusate/senna) 2 tablets po at bedtime nightly 29. Cough: Robitussin (guaifenesin) 15 ml po q 4 hrs prn 30. Sore Throat: Chloraseptic (phenol/sodium phenolate) throat spray q 2 hrs prn ________________ Date FORM 4-1181 REV. 11/2015 _______________ Time _________________________________ Physician Signature WHITE: Medical Record CANARY: Pharmacy ___________ PID Number Page 2 of 2