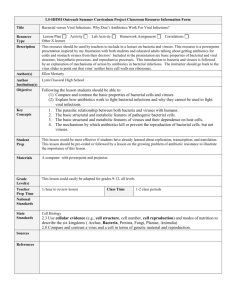
CHAPTER 34 - Nursing Pharmacology FrontPage
advertisement

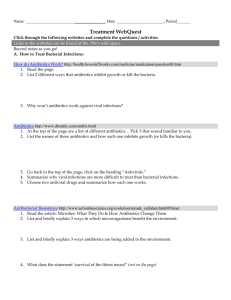
CHAPTER 34 DRUGS FOR BACTERIAL INFECTIONS LEARNING OUTCOME 1 Distinguish between the terms pathogenicity and virulence. Concepts 1. Pathogens are organisms that can cause disease by bypassing the body’s defenses. Examples of some pathogens are bacteria, viruses, fungi, intracellular organisms, and multicellular animals. Pathogens generally cause disease by one of two basic mechanisms: invasiveness or toxin production. Invasiveness is the ability of a pathogen to grow extremely rapidly and cause direct damage t o surrounding tissues by their sheer numbers. The second mechanism is the production of toxins. Even very small amounts of some bacterial toxins may disrupt normal cellular activity and, in extreme cases, result in death. 2. Pathogenicity is the ability of an organism to cause infection. Virulence is the ability of a microbe to produce disease when present in minute numbers. LEARNING OUTCOME 2 Explain how bacteria are described and classified. Concepts Bacteria are described by their shape—bacilli (rod shape), cocci (spherical), or spirilla (spiral); their ability to utilize oxygen—aerobic (with oxygen) or anaerobic (without), and by their staining characteristics— LEARNING OUTCOME 3 Compare and contrast the terms bacteriostatic and bacteriocidal. Concepts 1. Anti-infective drugs are known as antibacterial, antimicrobial, or antibiotic. They are classified by their chemical structures (e.g., aminoglycoside, fluoroquinolone) or by their mechanism of action (e.g., cell-wall inhibitor, folic-acid inhibitor). (See Table 34.1 for a look at bacterial pathogens and disorders.) 2. Anti-infective drugs act by affecting the target organism’s unique structure, metabolism, or life cycle. The goal is to eliminate the pathogen by bactericidal properties (to kill bacteria) or bacter iostatic properties (to slow the growth of bacteria). (See Figure 34.1 for Mechanisms of action of antimicrobial drugs.) LEARNING OUTCOME 4 Using a specific example, explain how resistance can develop to an anti-infective drug. Concepts 1. Acquired resistance occurs when a pathogen acquires a gene for bacterial resistance, either through mutation or from another microbe. Through mutation, the antibiotics destroy sensitive bacteria, and insensitive (mutated) bacteria remain. Mutations are random and occur during cell division; mutated bacteria multiply. It is important to remember that antibiotics do not create mutations. Acquired resistance Adams Ch 34-1 can also be caused by another microbe when resistant bacteria are passed to others. 2. The widespread use of antibiotics has not caused resistance, but overprescribing of antibiotics has worsened the problem because it results in loss of antibiotic effectiveness. Practitioners should only prescribe when necessary. Long-time use increases resistant strains. Nosocomial infections are often resistant. Prophylactic use is sometimes appropriate. The nurse should instruct the patient to take the full dose. (See Figure 34.2 for an illustration of acquired resistance.) LEARNING OUTCOME 5 Describe the nurse’s role in the pharmacologic management of bacterial infections. Concepts 1. The role of the nurse in the pharmacologic management of bacterial infections involves careful monitoring of a patient’s condition and providing education as it relates to the prescribed drug treatment. Obtain baseline medical, surgical, and drug history; lifestyle and dietary habits, including use of herbal or alternative therapies; and a detailed description of symptomology and current therapies. Obtain specimens for culture and sensitivity prior to the start of antibiotic therapy. Monitor for indications of response to therapy, including reduced fever, normal WBC count, improved appetite, and absence of symptoms such as cough. After parenteral administration, observe the patient for possible allergic reactions for 30 minutes, especially with the first dose. Monitor for superinfections. Replacement of natural colon flora with probiotic supplements or cultured dairy products such as yogurt or buttermilk may help to alleviate symptoms. Teach patients to wear medic alert bracelets if allergic to antibiotics, to report any symptoms of an allergic reaction, and to not stop taking the drug until the complete prescription has been taken. 2. Drug therapy with penicillins: Assess previous drug reactions to penicillin. If the patient has a history of a severe penicillin allergic reaction, also avoid cephalosporins. Monitor for hyperkalemia and hypernatremia. Monitor cardiac status, including ECG changes. 3. Cephalosporin therapy: Assess for the presence or history of bleeding disorders because cephalosporins may reduce prothrombin levels through interference with vitamin K metabolism. Assess renal and hepatic function. Avoid alcohol; some cephalosporins cause a disulfiram (Antabuse)–like reaction when alcoholic beverages are consumed. 4. Tetracycline therapy: This is contraindicated for use with patients who are pregnant and lactating because of the drug’s effect on linear skeletal growth of the fetus and child. Tetracycline therapy is also contraindicated in children less than 8 years of age because of the drug’s ability to cause permanent mottling and discoloration of the teeth. Tetracyclines decrease the effectiveness of oral contraceptives, so advise female patients to use an alternate method of birth control while taking the medication. Use with caution in patients with impaired kidney or liver function. Tetracyclines cause photosensitivity. Do not take these medications with milk products, iron supplements, magnesium containing laxatives, or antacids. 5. Macrolide therapy: Assess for the presence of respiratory infection. Examine the patient for history of cardiac disorders, because macrolides may exacerbate existing heart disease. Monitor hepatic enzymes with certain macrolides, such as erythromycin estolate. Multiple drug–drug interactions occur with macrolides. 6. Aminoglycoside therapy: Monitor for ototoxicity and nephrotoxicity during the course of therapy. Hearing loss may occur after therapy has been completed. Neuromuscular function may also be impaired. Increase fluid intake, unless otherwise contraindicated, to promote excretion. 7. Fluoroquinolone therapy: Because these agents may decrease leukocytes, monitor the WBC count. Carefully monitor patients with liver and renal dysfunction, because the drug is metabolized by the liver Ch 34-2 Adams and excreted by the kidneys. Inform the patient that these drugs may cause dizziness and lightheadedness and advise against driving or performing hazardous tasks during drug therapy. Inform patients receiving norfloxacin (Noroxin) that photophobia is possible. Some fluoroquinolones, such as ciprofloxacin (Cipro), may affect tendons, especially in children. 8. Sulfonamide therapy: Assess for anemia or other hematological disorders, because sulfonamides may cause hemolytic anemia and blood dyscrasias. Assess renal function, because sulfonamides may increase the risk for crystalluria. Avoid administering these agents in patients with a history of hypersensitivity to sulfonamides, because this can induce a skin abnormality called Stevens–Johnson syndrome. Avoid exposure to direct sunlight; use sunscreen and protective clothing to decrease the effects of photosensitivity. 9. Antituberculosis therapy: Assess the patient for a history of alcohol abuse, AIDS, liver disease, or kidney disease, because many antituberculosis drugs are contraindicated in those conditions. Use caution in patients with renal dysfunction, those who are pregnant or lactating, or those with a history of convulsive disorders. Assess for gouty arthritis. Because some antituberculosis drugs interact with oral contraceptives and decrease their effectiveness, female patients with childbearing potential should use an alternate form of birth control while using these medications. If taking isoniazid, avoid foods containing tyramine, such as aged cheese, smoked and pickled fish, beer and red wine, bananas, and chocolate. LEARNING OUTCOME 6 Explain the importance of culture and sensitivity testing to anti-infective chemotherapy. Concepts 1. Careful selection of the correct antibiotic, through the use of culture and sensitivity testing, is essential for effective pharmacotherapy and to limit adverse effects. Broad-spectrum antibiotics are effective for a wide variety of bacteria. Narrow-spectrum antibiotics are effective for a narrow group of bacteria. 2. Culture and sensitivity testing is examination of a specimen for microorganisms. The specimen is grown in the lab and identified. It is tested for sensitivity to different antibiotics. Bacteria may take several days to identify. Viruses may take several weeks to identify. Broad-spectrum antibiotics may be started before the lab culture is completed. LEARNING OUTCOME 7 Identify the mechanism of development and symptoms of superinfections caused by anti-infective therapy. Concepts 1. Multidrug therapy may be affected by antagonism, which occurs when combining two drugs decreases the efficacy of each of the drugs. Use of multiple antibiotics increases the risk of resistance. Multidrug therapy can be used when multiorganisms cause the infection, for the treatment of tuberculosis, for the treatment of HIV. 2. Superinfections are secondary infections that may occur during antibiotic therapy if too many host flora are killed by an antibiotic. Host flora prevent the growth of pathogenic organisms. Pathogenic microorganisms have a chance to multiply when they can opportunistically take advantage of a suppressed immune system. Signs and symptoms include diarrhea, bladder pain, painful urination, or abnormal vaginal discharge. 3. Host factors such as immune-system status, local conditions at the infection site, allergic reactions, age, pregnancy status, and genetics influence the choice of antibiotic. Adams Ch 34-3 LEARNING OUTCOME 8 For each of the drug classes listed in Drugs at a Glance, know representative drug examples, and explain their mechanism of action, primary actions, and important adverse effects. Concepts 1. Penicillin. Prototype drug: penicillin G (Pentids). Mechanism of action: to kill bacteria by disrupting their cell walls. Primary use: as the drug of choice against streptococci, pneumococci, and staphylococci organisms that do not produce penicillinase; also a medication of choice for gonorrhea and syphilis. Adverse effects: diarrhea, nausea, and vomiting; superinfections; and anaphylaxis. (See Table 34.2.) 2. Cephalosporin. Prototype drug: cefotaxime (Claforan). Mechanism of action: to act as a third-generation cephalosporin with a broad spectrum of activity against gram-negative organisms. Primary use: to be effective against many bacterial species that have developed resistance to earlier-generation cephalosporins—serious infections of the lower respiratory tract, central nervous system, genitourinary system, bones, blood, and joints. Adverse effects: hypersensitivity, anaphylaxis, diarrhea, vomiting, nausea, and pain at the injection site. (See Table 34.3.) 3. Tetracycline. Prototype drug: tetracycline HCL (Achromycin, others). Mechanism of action: to be effective against a broad range of gram- positive and gram-negative organisms. Primary use: for chlamydiae, rickettsiae, and mycoplasma. Adverse effects: superinfections. Tetracycline irritates the GI mucosa and may cause nausea, vomiting, epigastric burning, diarrhea, discoloration of the teeth, and photosensitivity. (See Table 34.4.) 4. Macrolide. Prototype drug: erythromycin (E-Mycin, Erythrocin). Mechanism of action: to act as a spectrum similar to that of the penicillins and to be effective against most gram-positive bacteria. Primary use: as the preferred drug for infections of Bordetella pertussis (whooping cough), Corynebacterium diphtheriae, and most gram-positive bacteria. Adverse effects: nausea, abdominal cramping, and vomiting. The most severe adverse effect is hepatotoxicity. (See Table 34.5.) 5. Aminoglycoside. Prototype drug: gentamicin (Garamycin). Mechanism of action: to act as a broad-spectrum, bacteriocidal antibiotic. Primary use: for serious urinary, respiratory, nervous, or GI infections when less-toxic antibiotics are contraindicated. It is often used in combination with other antibiotics or when drugs from other classes have proven ineffective. It is used parenterally, or as drops (Genoptic), for eye infections. Adverse effects: ototoxicity and nephrotoxicity. (See Table 34.6.) 6. Fluoroquinolone. Prototype drug: ciprofloxacin (Cipro). Mechanism of action: to inhibit bacterial DNA gyrase, thus affecting bacterial replication and DNA repair. Primary use: to be more effective against gram-negative than gram-positive organisms. It is prescribed for respiratory infections, bone and joint infections, GI infections, ophthalmic infections, sinusitis, and prostatitis. Adverse effects: nausea, vomiting, diarrhea, phototoxicity, headache, and dizziness. (See Table 34.7.) 7. Sulfonamide. Prototype drug: trimethoprim-sulfamethoxazole (Bactrim, Septra). Ch 34-4 Adams Mechanism of action: to kill bacteria by inhibiting bacterial metabolism of folic acid, or folate. Primary use: for urinary tract infections. It is also approved for the treatment of Pneumocystis carinii pneumonia, for shigella infections of the small bowel, and for acute episodes of chronic bronchitis. Adverse effects: skin rashes, nausea, vomiting, agranulocytosis, or thrombocytopenia. (See Table 34.8.). 8. Miscellaneous. Examples of miscellaneous antibiotics are clindamycin (Cleocin)—used for oral infections caused by bacteriocides. An adverse effect associated with clindamycin is pseudomembranous colitis. Metronidazole (Flagyl) is used to treat H. pylori infections of the stomach; vancomycin (Vancocin)—effective for MRSA infections; adverse effects include ototoxicity, nephrotoxicity, and red man syndrome. Some of the new miscellaneous antibiotics are: Oxazolidinones— linezolid (Zyvox) is as effective as vancomycin against MRSA; Cyclic lipopeptides—daptomycin (Cubicin) is used to treat serious skin infections; Carbapenems—imipenem (Primaxin) has some of the broadest spectrums; Ketolides— telithromycin (Ketek) is used for respiratory infections; Glycylcyclines—tigecycline (Tygacil) is used for drug-resistant abdominal infections and complicated skin infections. (See Table 34.9.) ANIMATIONS AND VIDEOS Mechanism in Action: Penicillin (Pentids) Mechanism in Action: Ciprofloxacin (Cipro) LEARNING OUTCOME 9 Explain how the pharmacotherapy of tuberculosis differs from that of other infections. Concepts 1. Tuberculosis is caused by Mycobacterium tuberculosis. Its cell wall is resistant to anti-infectives, so the body’s immune response attempts to isolate the pathogen by walling it off. Tuberculosis may remain dormant in walled-off areas called tubercles, but a decreased immune system can give tuberculosis the opportunity to become active. 2. Therapy is long term. Six to twelve months of drug therapy is needed to reach isolated pathogens in the tubercles, and the therapy must be continued for the full course even if there are no symptoms. Patients with multidrug-resistant infections require therapy for 24 months. Multidrug therapy consists of two to four antibiotics that are administered concurrently. Multiple-drug therapies are needed in the treatment of tuberculosis because the complex microbes are slow growing and commonly develop drug resistance. Therapy is initiated with first-choice drugs, and then when resistance develops, secondchoice drugs are used. The second-choice drugs are more toxic and less effective than first-choice drugs. 3. Chemoprophylaxis means that antituberculosis drugs are used prophylactically in high-risk populations. Close contacts and family members of recently infected tuberculosis patients begin therapy immediately after a patient has a positive tuberculin test. Patients with AIDS, those who are HIV-positive, or those who are receiving immunosuppressant drugs also receive therapy. LEARNING OUTCOME 10 Adams Ch 34-5 Use the nursing process to care for patients who are receiving drug therapy for bacterial infections. Concepts 1. Patients Receiving Antibacterial Therapy—Assessment: Obtain a complete health history including allergies, drug history, and possible drug interactions. Assess signs and symptoms of current infection noting location, characteristics, presence or absence of drainage and character of drainage, duration, presence or absence of fever or pain. Evaluate appropriate laboratory findings (e.g., CBC, culture and sensitivity, hepatic and renal function studies). Report immediately severe diarrhea, especially containing mucus, blood, or pus, yellowing of sclera or skin decreased urine output or darkened urine. Assess for possibility of pregnancy or breast -feeding in patients prescribed tetracycline antibiotics. 2. Patients Receiving Antibacterial Therapy—Nursing diagnoses: Infection; Pain, related to infection; Hyperthermia; Deficient Knowledge (drug therapy); Risk for Injury, related to adverse drug effects; Risk for Deficient Fluid Volume, related to fever, diarrhea caused by adverse drug effects; Risk for Noncompliance, related to adverse drug effects, deficient knowledge, or cost of medication. 3. Patients Receiving Antibacterial Therapy—Planning: The patient will report diminished signs and symptoms of infection, decreased fever; be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper selfadministration of the medication (e.g., dose, timing, when to notify provider). 4. Patients Receiving Antibacterial Therapy—Implementation: Monitor vital signs and symptoms of infection to determine antibacterial effectiveness. Monitor for hypersensitivity and allergic reaction. Monitor for severe diarrhea. Monitor periodic lab work: hepatic and renal function tests, CBC, urinalysis, culture and sensitivity, peak and trough drug levels. Administer drug around the clock. Monitor for superinfection. Monitor intake of OTC products such as antacids, calcium supplements, iron products, and laxatives containing magnesium. Monitor for photosensitivity. Monitor for hepatic, renal, and/or ototoxicity (e.g., jaundice, RUQ pain, darkened urine, diminished urine output, tinnitus, vertigo). Determine the interactions of the prescribed antibiotics with various foods and beverages. Monitor IV site for signs and symptoms of tissue irritation, severe pain, and extravasation. Monitor for side effects, renal function, symptoms of ototoxicity, and compliance with antibiotic therapy. Monitor for development of “Red Man” syndrome in patients receiving vancomycin. 5. Patients Receiving Antibacterial Therapy—Evaluation: Planning: The patient will report diminished signs and symptoms of infection, decreased fever; be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). 6. Patients Receiving Antituberculosis Agents—Assessment: Obtain a complete health history including allergies, drug history, and possible drug interactions. Assess signs and symptoms of current infection noting symptoms, duration, or any recent changes. Assess for concurrent infections, particularly HIV. Assess for presence or history of tuberculosis, immunosuppressant status, and kidney or liver disease. Assess cognitive ability to comply with long-term therapy. Evaluate appropriate laboratory findings (e.g., CBC, AFB culture and sensitivity, hepatic and renal function studies). 7. Patients Receiving Antituberculosis Agents—Nursing diagnoses: Infection; Fatigue; Imbalanced Nutrition, Less than Body Requirements, related to fatigue, adverse drug effects; Deficient Knowledge (drug therapy, infection control measures); Risk for Noncompliance, related to adverse drug effects, deficient knowledge, length of treatment required, or cost of medication; Risk for Social Isolation, related to disease, length of treatment. Ch 34-6 Adams 8. Patients Receiving Antituberculosis Agents—Planning: The patient will report diminished signs and symptoms of infection, decreased fever and fatigue, increased appetite). Be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). 9. Patients Receiving Antituberculosis Agents—Implementation: Monitor for hepatic side effects. Monitor for neurologic side effects. Collect sputum specimens. Monitor for dietary compliance when patient is taking isoniazid. Monitor for side effects specific to various antituberculosis drugs. Monitor for hepatic, renal, and/or ototoxicity (e.g., jaundice, RUQ pain, darkened urine, diminished urine output, tinnitus, vertigo). Establish infection-control measures. Establish therapeutic environment to ensure adequate rest, nutrition, hydration, and relaxation. Monitor patient’s ability and motivation to comply with therapeutic regimen. 10. Patients Receiving Antituberculosis Agents—Evaluation: The patient reports diminished signs and symptoms of infection, decreased fever and fatigue, increased appetite). Is free from or experiences minimal adverse effects. Verbalizes an understanding of the drug’s use, adverse effects, and required precautions. Demonstrates proper self-administration of the medication (e.g., dose, timing, when to notify provider). Adams Ch 34-7