Coronary circulation
advertisement
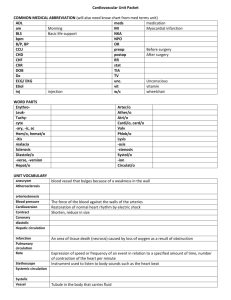
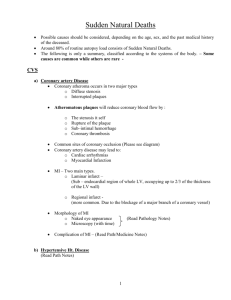
12- Circulation through special regions Coronary circulation Anatomical considerations : The two coronary arteries that supply the myocardium arise behind the aortic valve at the root of the aorta. Eddy currents keep the valves away from orifices of the coronary arteries. Venous blood returns to the heart through the coronary sinus and anterior cardiac veins which drain into the right atrium. Anastomoses between coronary arteries in humans are only less than 40 µm in diameter, but there is evidence that these channels enlarge and increase in number in patient with coronary artery disease. Regulation of coronary Blood flow: 1-Neural factor: Coronary arterioles contain α-adrenergic receptors which mediate vasoconstriction and β2-adrenergic receptors which mediate vasodilation. The predominant effect of sympathetic stimulation in coronary arteries is vasodilation. Parasympathetic stimulation also causes modest dilatation of normal coronary arteries. Healthy coronary endothelium release nitric oxide (NO) which promotes vasodilation, but if endothelium is damaged by atheroma, endothelium dependent vasodilation may be impaired. 2-Chemical factor: When metabolism of myocardium is increased, vasodilator substances increase which cause coronary vasodilation such as O2 lack, increase concentration of CO2, H+, K+, lactate, and adenosine. Adenosine is powerful vasodilator in coronary vessels. 3-Aortic pressure: When the systemic blood pressure fall, the noradrenergic discharge increases due to effect of the sympathetic reflex and coronary blood flow increases. At same time cutaneous, renal, splanchnic vessels are constricted. So the coronary circulation shows autoregulation. Coronary blood flow at rest in humans is about 250 ml / min. (5 % of cardiac output). The coronary vessels are severely compressed during systole. BF to left ventricle is during diastole only, while BF to right ventrile and atria are reduced during systole. So subendocardial portion of left ventricle is prone to ischemic damage which is most common site of myocardial infarction (MI). The narrowing coronary artery by atheromatous does not limit blood flow even during exercise until the cross-sectional area of vessel is reduced by at least 70%. Coronary artery diseases : 1- Stable angina. The most cause of angina is atherosclerosis. See figure 49. 2-Unstable angina. Coronary arteries can be constricted by vasospasm to produce anginal symptoms. 3-Myocardial infarction (MI). If myocardial ischemic is sever and prolonged, irreversible changes occur in the Myocardial muscle lead to MI. The cause of MI is atherosclerotic plaque or hemorrhage into it which triggers the formation of coronary clot at site of plaque. Figure (49): Atherosclerotic plaque. Coronary arteries bypass grafting (CABG): The internal mammary arteries, radial arteries or segment of patient's own saphenous vein can be used for bypass coronary artery stenosis. This usually involves major surgery under cardiopulmonary bypass. See figure50. Figure (50): Coronary arteries bypass grafting. Microcirculation The major mechanisms for exchange are diffusion and filtration. Substances pass through the junction between endothelial cells and through fenestrations, when they are present. Some also pass through the cells by vesicular transport or through the cytoplasm in the case of lipidsoluble substances. Diffusion is much more important in exchange of nutrients and waste materials between blood and tissue. O 2 and glucose are in higher concentration in bloodstream than in the interstitial fluid, so they diffuse to the interstitial fluid, whereas CO 2 diffuses in the opposite direction. The rate of filtration at any point depends upon a balance of Starling forces. Cerebral circulation Anatomic consideration of vessels: The principal arterial inflow to brain in humans is via four arteries. Two internal carotid and two vertebral arteries. The vertebral arteries unit to form the basilar artery. The basilar and the carotids artery form the circle of Willis below the hypothalamus. The circle of Willis is the origin of the six large vessels supplying the central cortex. Figure 51. Figure (51): Cerebral circulation. Venous drainage from the brain by deep veins and dural sinuses empties principally into the internal jugular veins in humans. The cerebral vessels have a number of anatomic features: 1- In choroid plexus there are gaps between the endothelial cells of capillary walls, but the choroid epithelial cells that separate them from CSF are connected to one another by tight junction. 2- Capillaries in the brain substance are non-fenestrated resemble capillaries of muscles, tight substance between endothelial cells. Substance transport through capillaries is by vesicular transport. 3- Brain capillaries are surrounded by end feet of astrocytes. These end feet are closely applied to the basal lamina of the capillaries but they do not cover the entire capillary wall and there are gaps about 20 nm between end feet. See figure 52. Figure (52): Transport across cerebral capillaries (Ganong's review of medical physiology 2010). Innervations: three systems of nerve innervate the cerebral blood vessels postganglionic sympathetic neurons, their ending contain norepinephrine many contain neuropeptide Y, they cause vasoconstriction. Cholinergic neurons also innervate the cerebral vessels and their ending contain acetylcholine many contain vasoactive intestinal peptide (VIP), they cause vasodilation. While sensory nerves are found on most distal arteries, their cell bodies in the trigeminal ganglia and contain P substance. Toughing or pulling cerebral vessel cause pain. Cerebral blood flow: There are many methods to measure cerebral blood flow as Kety method which depends on Fick principle by use inhaled nitric oxide (N2O) Blood flow in the cerebral cortex and cerebellar cortex is high, but the part of the brain with highest blood flow per gram is the inferior colliculus. The blood flow in gray matter is much greater than in white matter. The average cerebral blood flow in young adult is about 54 mi/ 100 g / min. If the weight of brain is 1400 gm, so the cerebral blood flow is 765 ml/min. Regulation of cerebral circulation: In site of marked local fluctuation in brain blood flow, the blood flow remains relatively constant. The factors that effect blood flow are: 1- Intracranial pressure: the cerebral vessels are compressed whenever the cranial pressure rises. 2- Mean venous pressure: any change in venous pressure causes a similar change in the intracranial pressure. 3- Concentration of vasodilator substances: There are marked local fluctuation in blood flow by vasodilator metabolites such as K ions, H ions and adenosine. The most important local vasodilator for the cerebral circulation is CO2 4-Viscosity of blood. 5- Mean arterial pressure at brain level. Neural sympathetic control help to maintain constant blood flow with elevated blood pressure, but it play a minor role. The autorgulation maintains a normal cerebral blood flow at arterial pressure of 65 – 140 mmHg. Brain is sensitive to hypoxia, and occlusion of its blood supply produces unconsciousness in short period as 10 second. Glucose enters the brain via glucose transporter, found in high concentration in cerebral capillaries. There is decrease glucose utilization during sleep. Glucose utilization at rest parallels to blood flow or oxygen consumption. Because of low stored glucose and glycogen, the brain can not stand when total blood occlusion for more than 2 minute (which is longer time than it can withstand hypoxia). The cortical regions are more sensitive to hypoglycemia than centers in the brain stem. Ammonia is very toxic to nerve cells and ammonia intoxication is major neuralgic symptoms in hepatic failure. Insulin is not required for most central cells to utilize glucose. Effect of gravity on the body The following changes occur when an individual move from a supine position to standing position: 1- A significant increase blood pools in the lower extremities. 2- Increase venous pressure in legs. 3- Decrease venous return, both stroke volume, COP decrease (FrankStarling relationship), and decrease in arterial pressure 4- If COP decrease cerebral blood pressure becomes low, fainting may occur. Compensatory mechanism: Vasomotor center then increases sympathetic outflow to the heart and blood vessels and decreases parasympathetic outflow to heart. As a result, heart rate and TPR increase and blood pressure increases toward normal Effect of altitude on the body: As we ascend to higher altitude in aviation, The following changes occur: 1-The oxygen partial pressure decreases, hypoxia beginning at altitude of about 12,000 feet ( drowsiness, lassitude, mental and muscle fatigue, sometime headache). 2-Hypoxia stimulates arterial chemoreceptors to increase ventilation to a maximum of about 1.65 times of normal. This is an immediate compensation with in seconds. 3-It increases red blood cell production, hematocrit from 40 – 45 to about 60. 4- Increase concentration of hemoglobin from 15 gm /dl to about 20 gm /dl. 5- It increases diffusing capacity for O2 through the pulmonary membrane 3 fold as much as during exercise. Normal capacity 21 ml / mmHg / minute. 6- Increase the cardiac output (COP) 30% immediately after a person ascends to high altitude but then decrease back toward normal as the blood hematocrit incre es. 7- Increase in number of systemic circulatory capillaries. 8- In animals native to altitude of 13,000 to 17,000 feet, cell mitochondria and cellular oxidative enzyme systems are slightly more plentiful.