The impacted mandibular third molar is a frequently
advertisement

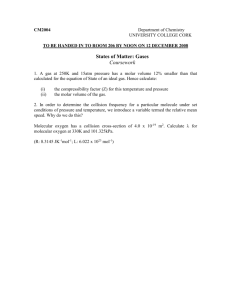
The impacted mandibular third molar is a frequently encountered • surgical problem in general dental practice. The removal of • impacted mandibular third molar is one of the most important and • most commonly performed oral surgical procedures. The general • practitioner who in most instances happens to see these patients • first is required to make two important decisions , firstly • whether the impacted third molar is to be removed or not and • secondly to determine whether he ought to remove it himself or • refer to a practising oral surgeon. Needless to say that these • important decisions will be based in the practioner's • understanding of the various aspects of the problem. In frequency • of occurance mandibular third molar is followed by maxillary • third molar,canine and mandibular canine. ETIOLOGY : The exact cause of impacted teeth is still unclear. It is • unlikely that there is one single factor responsible and with the • present understanding of the problem it appears to be • multifactorial in nature. The following are the various theories • or concepts put forth to explain the occurance of impacted teeth. 1. Phylogenic Theory: The present soft and refined diet does not • require a decided masticatory effort to chew the food • ,consequently it does not provide sufficient stimulus necessary • for jaw growth resulting in evolutionary reduction in size of • the human mandible and maxilla unable to accomodate the full • complement of teeth. 2. MENDELIAN THEORY : Impacted teeth could be the result of • inheretance of small jaw from one parent and a complement of • large teeth from the other parent. 3. ENDOCRINE DISORDERS : Several endocrinal disturbances can • result in dental anomalies and impacted teeth. e.g. • Hypothyroidism, rickets. 4. SKELETAL GROWTH DISTURBANCES : The skull and alveolar growth • influence the position and eruption of teeth. Any disturbance • affecting this at that particular age can result in impacted • teeth. e.g. 5. SYSTEMIC CONDITIONS : A number of systemic conditions which • interfere with normal growth and development of the face and jaws • may result in impacted teeth. e.g. Cleidocranial imperfecta,oxycephaly. dysostosis, osteogenesis • 6. LOCAL FACTORS : In addition to various systemic reasons • mentioned above, even local facts like trauma and infections may • play a role in the etiology of impacted teeth. ð 7 •3 ŠINDICATIONS FOR REMOVAL OF IMPACTED LOWER THIRD MOLAR. The impacted mandibular third molar may lead to several • complications if left untreated. The following are the common • reasons for which an impacted lower third molar is removed. 1. Repeated attacks of pericoronitis 2. Dental Caries 3. Periodontal disease 4. Resorption of second molar 5. Prior to orthodontic treatment 6. Presence in edentulous jaw 7. Involved in cyst formation 8. Obscure facial pain 9. In line of fracture mandible 10.Injury to soft tissues. CLASSIFICATIONS : I GEORGE WINTER'S CLASSIFICATION : George Winter in 1926 offered for the first time a scientific • and practical classification of the impacted mandibular third • molar which is still widely used. Winter based his classification on the relationship of long axis of the impacted third molar with that of the adjacent second • molar or in its absence the next adjoining teeth. The following positions are described. a. Vertical b. Mesioangular c. Horizontal d. Distoangular e. Buccoangular f. Linguoangular g. Unusual positions. • PELL & GREGORY'S CLASSIFICATIONS : Pell and Gregory in 1942 proposed a more detailed classification • taking into consideration three aspects of impacted mandibular • third molar A. Position and angulation : Winter's Classification is • incorporated for this. B. Relationship of impacted third molar to the ramus and second molar in terms of space available. • C. Related to the depth in the bone. Postion & Angulation : Based on the relationship of the long axis of the impacted third • molar with that of adjacent second molar ( Winter's • Classification ) ð 7 •3 ŠVerical Mesioangular Horizontal Distoangular Buccoangular Linguoangular Unusual positions Relation of the tooth to the ramus of the mandible and the • second molar Class I : There is sufficient amount of space between the ramus and the distal of the second molar to accomodate the third molar. Class II : The space between the ramus and the distal of the • second molar is less than the mesiodistal diameters of third • molar and a portion of third molar is present in the ramus . Class III : All or most of the third molar is present in the • ramus itself. Relative depth of the third molar in the bone : Position A: The highest portion of the tooth is on a level with • or above the occlusal level. • Position B: The highest portion of the tooth is below the • occlusal plane but above the cervical line of the second molar. Position C: The highest portion of the impacted tooth is below • the cervical line of the second molar. KAY 'S CASSIFICATION : Kay in classified impacted mandibular third molar taking • three important aspects into consideration. a. Position & angulation ( Winter's Classification) b. State of eruption of the third molar c. Number and pattern of roots. PERICORONITIS : Pericoronitis is the infection of the soft tissues around and • above the crown of a partially erupted tooth. The condition is • seen only when there is communication between the third molar and • the oral cavity. Pericoronitis is encountered only during the • eruption of lower third molar seldom with any other tooth. • Malposition and unduely prolonged eruption may contribute to • this. When the third molar is in the process of eruption a small sinus • may communicate the oral cavity with the follicle or the space • which lies between the crown and the layer of condensed bone. Inflammation probably begins in the follicle later extending to • the overlying soft tissues producing the classical clinical • features. Virulence of the bacteria with the retromolar space ð 7 •3 •Šand the trauma to the operculum which is edematous from the cusps • of the opposing third molar can influence the course. Pericoronitis is a very common condition in the age group of 17 • to 25 years, affects both sexes equally with highest incidence • during spring and autumn. Peridisposing factors are lowering of tissue resistance due to • systenic factors, upper respiratory infections,emotional • stress,fatigue and pregnancy. CLASSIFICATION : Pericoronitis is classified on the basis of clinical findings • into acute,subacute and chronic categories. Acute pericoronitis : Acute pericoronitis which is more serious • and common is charaterized by both extra-oral and intra-oral • findings along with consitutional symptoms. Charaterized by sever throbbing pain which is intermittant, • radiates to adjacent and areas exacerbated by chewing and • interferes with sleep. There is extra-oral swelling and • limitation of mouth opening. The submandibular lymph-nodes on the • affected side are enlarged and tender. Constitutional symptoms include raise in temperature, pulse and • respiratory rates, patient looks ill, leukocytosis will be • present. Intra orally gum pad is swollen, tender,red in appearance , • gentle pressure may cause a discharge of pus from beneath the • flap. There is marked foetor oris and the operculum may show sloughing • or ulcerations and signs of indentation related to cusps of • upper third molar. If acute pericoronitis is not properly treated • several severe complications may result. Treatment : Once a definitive diagnosis is made proper treatment • should be instituted without any delay. Standard therapetic • mesaures include both general and local . General measures : 1. Bed rest is ideal 2. Soft and nourishing diet 3. Relief of pain by prescription of analgesics 4. Antibiotic therapy Local Measures: The local measures are very effective in many cases. 1. The impinging maxillary third molar should be extracted. If • it is to be retained proper cuspal grinding should br carried • out. ð 7 •3 Š2. If pus is present in the buccal sulcus, incision and drainage • should be carried out. 3. The use of caustic solutions e.g. trichlor acetic acid beneath • the flap is of great value in releving pains. 4. Frequent use of hot saline mouth washes is of great value in • combating pain and speeding resolution of pericoronitis. 5. Once the active infection has subsided the incriminated mandibular third molar is removed. Treatment of sub acute pericoronitis is essentially same as the • acute and chronic pericoronitis does not usually require any • treatment. DENTAL CARIES : The space between the erupting third molar and • second molar provides an ideal environment for the development of • dental caries not only in the third molar but also on the distal • aspect of second molar due to collection of food debris and • plaque formations which cannot be easily removed by either tooth • brush or action of tongue. Due to the technical difficulties of • conserving such a tooth removal is indicated unless retention of • the tooth is warranted. Periodontal Disease : Impacted third molars are often associated • with a high incidence of periodontal pocket formation distal to • the second molar. The removal of third molar is the only • effective way of eliminating the pocket formation in such cases. Resorption of the second molar : When there is a tooth • impaction of the third molar, the second molar roots can undergo • considerable resorption resulting even in the exposure of pulp • leading to peroiapical infection of second molar. The third molar • should be extracted in all those cases where the crown of the • third molar is in close contact with that of second molar roots • before the damage is done. ORTHODONTIC REASONS : A controversy still exists on prophylatic removal of third • molars prior to orthodontic treatment, similarly whether crowding • of lower anterior teeth could be produced by the forces exerted • during eruption of third molar. Many orthodontists prefer removal • of third molars before starting the orthodontic management. Presence of third molars in edentulous mandible. As resorption of the mandible progress rapidly under a denture • the retained third molar may become more superficial and may • either interfere with the retention of the lower denture or cause • pain & ulcerations. The impacted third molar should be removed in • such conditions. ð 7 •3 ŠCyst Formation : The follicle of the impacted third molar may • undergo pathological changes leading to the formation of a • dentigerous cyst, ameloblastoma or even carchonoma in the • lining .Any such changes suspected the impacted third molar • should be removed and the soft tissue lining examinated • histologically. OBSCURE FACIAL PAIN : Impacted lower third molar is often implicated as a cause of • untractable facial pain due to its close relationship with the • inferior dental neurovascular bundle. Removal of the impacted • tooth may relieve symptoms in few cases. In line of mandibular fracture: A third molar is line of mandibular fracture is often removed • to enhance healing unless its retension is warranted to prevent • displacement of fragments until some callus formation has taken • place. Injury to soft tissues : Malposed partly erupted third molar causing irritation to • buccal mucosa,tongue should be extracted to prevent chronic • irritation and discomfort. Prophylactic Reasons: Prophylatic removal of the impacted third molars is occassionally undertakers to avoid problems in future when conditions may not • be suitable for surgery. Assesment of impacted lower third molar: A thorough assesment of impacted lower third molar is absolutely • necessary to predict the possible difficulties and complications • which might arise during the surgical procedures and to take • possible measures to prevent them. Assesment also helps the practitioner to decide whether he ought • to remove the tooth himself or refer to a practising oral surgeon • after taking into consideration the surgical skill required and • the facilities available. Factors to be considered in assesment are general and local General factors : Age of the patient is an important general factor which has a • bearing on the method to be employed for bone removal. Two other • important general factors are medical condition of the patient • and the temperament which will influence the choice of • anaesthesia. ð 7 •3 ŠLocal Factors : Local factors which should be taken into • consideration are size of the mouth,mandibular retrusion and the • relationship of the external oblique ridge to the impacted third • molar. The access will be better if the mouth opening is normal • Mandible in either normal or prognathic and the external oblique • ridge is situated behind the third molar. Radiological assesment : Radiographs required for proper assesment are 1. Periapical film which will provide most information and often • is the only radiograph required. 2. Lateral oblique view is indicated when the third molar is • deeply placed to assess the amount of bone present below the • impacted tooth to prevent possible fracture during surgical • procedure. Also indicated in cases of extreme trismus and the • patient unable to retain the I.O film due to retching. 3. Lower occlusal film in invaluable in deciding whether the • impacted tooth is placed bucccally or lingually. 4. Orthopantograms has the advantage if there is any pathology • associated with the impacted third molar or to study all the four • impacted third molars. Points to be noted in the periapical radiograph. 1. Position and angulation of the third molar based on Winter's • classification. 2. Amount of space available between diatal aspects of second • molar and ramus of the mandible for the third molar. 3. Depth of the third molar and state of eruption 4. Size and shape of the crown of third molar 5. Number and pattern of roots of third molar 6. Crown and roots of second molar 8. Density of bone 9. Relationship with mandibular canal 10. Relationship with external oblique ridge to asses the access. Third molar relationship with mandibular canal. In most of the cases the mandibular canal passes below the roots • of the impacted third molar and is clearly distinguished as a • radiolucent band bound by radioopaque lines. It is also often seen to be crossing the roots of the third molar • due to radiographic superimposition when it is actually either on • the lingual or buccal aspects. But occassionally the contents of • the mandibular canal may cause either grooving,deep grooving or • complete perforation of the roots of the third molar with • distinct radiographic appearances. ð 7 •3 Š1. Groove is seen as a band of decreased radioopacity crossing • the roots and coinciding with the mandibular canal. 2. Deep groove is seen as a band of increased radiolucency with interruption of radioopaque outline crossing the root • coinciding with the outline of mandibular canal. 3. Perforation is characterized by narrowing of the radiolucent • band with loss of the white lines. WINTER'S IMAGINARY LINES : • George Winter described three imaginary lines which could be • drawn on a standard periapical film to determine the position and • depth of the impacted third molar within the mandible. WHITE LINE : The white line is drawn along with occlusal surfaces of the • erupted mandibular molars and extended posteriorly over the third • molar regions. The axial inclination of the impacted molar is • determined with this. AMBERLINE : Drawn from the surface of the bone lying distally • to the third molar to the crest of the inderdental sept between • the first and second molars. Amber line indicates the margin of • the alvelor bone. REDLINE : It is a perpendicular dropped from the amber line to • an imaginary point of application for an elevator which is • usually the cementoenamel junctions on the mesial side except in • case of distoangular where it is on distal aspect of third molar. • Red line indicates the depth of which the impacted tooth lies in • the mandible. REMOVAL OF IMPACTED LOWER THIRD MOLAR : Before the surgical procedure is planned selection of a standard • set of instrumants and choice of anesthesia must be considered. INSTRUMENT'S CHOICE : The following is a list of standard instruments required in the • removal of impacted molar. -MOUTH MIRROR -DENTAL PROBE -TWEEZERS -B.P. HANDLE WITH NO 15,12 BLABES -HOWARTH PERIOSTEAL ELEVATOR -STRAIGHT HAND PIECE, BURS ROUND,FISSURE -SALINE IRRIGATION SYRINGE COUPLAND,WARWICK JAMES ELEVATORS MOLAR FORCEPS ROUNGER'S FORCEPS, BONE FILE ð 7 •3 Š ARTERY FORCEPS CURVED CURRETTE NEEDLE HOLDER TISSUE HOLDING FORCEPS B.B.S. SUTURE WITH NEEDLE SCISSORS. Choice of Anaesthesia: The impacted third molar may be removed under either local • anesthesia. I.V Sedation with local anaesthesia General anaesthesia. Techincally most of the third molars can be removed under local • anaesthesia . However in apprenhesive patients I.V. Diazepam • could be used for better patient co-operation. General anaesthesia is used for technically difficult cases, • surgery time more than an hour and when it is patient's choice. STANDARD OPERATIVE PLAN : The following are the steps in operative plan :I Incision & reflection of mucoperiosteal flap II Removal of Bone III Removal of the tooth IV Toilet of the wound V Closure of the wound VI Post operative care. INCISION & REFLECTION OF MUCOPERIOSTEAL FLAP While making an incision to expose the impacted third molar the • three important requirements of adequate access,proper blood • supply to the flap and uneventfull healing should be ensured. The • standard and commonly used incision starts half an inch in the • mucobuccal fold at the junction of the anterior two thirds and • posterior one third of the second molar,carried to the distal • aspect where the incision is carried backwards and outwards along • with the line of the external oblique ridge. With the help of a periosteal elevator the mucoperiosteal flap is raised exposing • the bone. Removal of Bone : Bone can be removed either by chisel or bur. Bone removal by using bur in the method of choice when working • under local anaesthesia. Number 8 round and fissue burs are used • in a straight hand piece. Bone is guttered on the buccal aspect • and also particular attention should be paid to clear the bone at • distobuccal angle. Care should be taken not to cause heat • necrosis of the bone by continous saline irrigation through out • the procedure. Atleast the full crown and cervical one third of • the roots should be cleare from bone before elevation of the • tooth is attempted. ð 7 •3 ŠRemoval of the tooth : A Warwick James or Cryers elevator is used to luxate the • third molar from its socket using gentle pressure with the buccal • plate on mesial aspect of the third molar for leverage. In case • of tooth impaction where the crown of third molar is locked with • second molar, sectioning of tooth is indicated. Toilet of the wound : A careful wound toilet must be carried out • before closure of the wound. All the overhanging sharp bony • margins should be smoothened, detached bone pieces either buccal • lingual plates or interadicular septums likely to be devitalized • should be removed. If there is any granulation tissue proper • curettage is advised and traumatized flaps properly trimmed. • Thorough irrigation is carried out finally to remove all the bone • powder. Proper haemostasis should be obtained prior to closure of • the wound to prevent haematoma formations. Closure of the wound: The wound is closed with two or three • interrupted sutures using black braided silk. One suture is • placed just distal to second molar taking a large bite on the • buccal flap to the lingual flap. Second suture is placed • distally. The vertical incision in the mucobuccal fold is not • required to be sutured. Post operative care : Proper postoperative care and instructions • should be given to the patient to avoid discomfort and help • prevent complications. 1. Ice application in the immediate post operative period to prevent ocedema formation. 2. Analgesics to relieve pain • 3. Prophylactic antibiotic treatment 4. Warm saline gargles after 24 hours 5. Sutures to be removed on 6th post operative day. Complications in the removal of third molar The complications that might arise during the removal of • impacted third molar may be considered as those occuring during • the surgical procedure and those resulting in the postoperative • period. I Complications during surgical procedures A. During incision and raising mucoperiosteal flap Damage to lingual nerve if the incision is carried lingually. Haemorrhage due to damage to nutrient vessel in the retromolar • triangle rare complication of damage to facial vessels if knife • slips into the cheek causing massive heamorrhage. ð 7 •3 ŠB. During removal of bone : Necrosis of bone due to heat if saline irrigation is not done • properly Damage to second molar Damage to inferior dental neurovascular bundle if bur goes deep. Splitting of bone when chisel is used with out proper stop cuts. C. Removal of tooth Fracture of the roots Accidental luxation of second molar if elevator is not used properly • Damage to inferior dental canal contents. Fracture of the mandible if excessiveforce is used to elevate the • tooth .Toilet of the Wound : During curettage of the socket • exposure of the mandibular canal when it lies close to the root • apices. Closure of the wound : Neuropraxia of the lingual nerve if it is • caught in the suture when a large bite of lingual flap is taken. Post operative complications : 1. Pain: Removal of third molar is associated with pain and can • be relieved by analgesics. 2. Swelling : Oedema following third molar removal is inevitable • and resolves in a few days time & does not require any special • treatment other than warm saline gargles. 3. Trismus : Trismus is a protective phenomena which sets in to • prevent aggravation of pain during jaw movements. 4. Haematoma formation : This results if proper haemostosis is • not achieved before closing the wound and could be differentiated • from edema by discolouration of the soft tissues, firm • consistency and severe pain and tenderness. Treatment includes removal of sutures evacuation of the collected • blood and antibiotic course. 5. Infection: Incidence of dry socket is more in third molar • extractions compared to other teeth. It can be easily diagnosed • by history and treated by irrigation placing a sitable sedative • pack and a cause of an antibiotics Impacted Maxillary Canine: Among the impacted teeth the third molars are followed by • maxillary canine in frequency. Impaction of maxillary canine is • more common than mandibular canine and it can be one canine or • both. Possible reasons for unerupted canine: 1. Upper canine has the largest distance to travel before ð 7 •3 •Šreaching occlusion. 2. If it is on the palatal aspect the thick mucoperiosteum and • palatal bone resist eruption 3. Scar tissue in the path of eruption 4. Space between the first premolar and lateral incisor less than • mesodistal diameter of canine due to early loss of decidous • canine. 5. Presence of odontome or supernumerary tooth in the path of • eruption 6. Associated with syndromes Classification; Simple classification used for impacted canines Labial position Palatal position Intermediate position A great number of maxillary canines are impacted on the palatal • aspect and the reason attributed to this is the development of • permanent tooth germ on the palatal aspect of deciduos canines. Localization of unerupted canine: Clinical examination : Careful examination of the labial sulcus and palate may reveal exposure of the tip of the canine or a • smooth hard swelling corresponding to canine region. But on • several occasions the clinical findings will not contribute to • the location of the unerupted tooth. Radiographic examination: Proper radiographic assesment is • essential to determine whether the canine is in a latrial or • palatal position and also to study its relationship with other • adjoining teeth, in addition to knowing the size and shape of its • root. a. Periapical films: The condition of the adjacent teeth to the • unerupted canine together with the size , shape and root pattern • of canine are revealed in this radiograph. b. Parallax method of Clark: Also known as the tube shift method is invaluable in the • localization of the maxillary unerupted canine. This is a more • reliable method to know whether the canine is in a labial or • palatal positio . A periapical radiograph of the canine area is • taken and the x-ray tube is moved either in a mesial or distal • direction and a second periapical film is taken. ð 7 •3 ŠThe two radiographs taken are then studied and compared and if • the unerupted tooth is seen to move in the same direction as the • x-ray tube it is lying palatally, while if it moves in the • opposite directions it is lying on the labial side. c. Vertex occlusal view: Taken with the central ray passing along • the long axis of the central incisor. It is also used to • determine the true position of the impacted canine. Since it has to pass through the skull and facial bones the film • lacks the contrast and details, therefore longer exposure is • required and an intra-oral cassette containing an intensifying • screen is required. purpose,it can assist in determining the position of the • unerupted canine. If the tip of the canine is shown to be lying • in front of the apices of the incisors the tooth will be on • labial side and if the tip is behind it will be on palatal side. Management of impacted canine : There are several methods in which an unerupted maxillary canine • is managed. 1. Leaving it in place : If the erupted tooth is asymptomatic, elderly patient, not • causing damage to the adjoining teeth it can be left as it is and • kept under observation periodically for any possible pathological • changes. 2. Surgical exposure : This is the most commonly used mathod of • managing impacted canine. When the patient is young with the • canine having eruption potential the tooth should be surgically • exposed and allowed to erupt irrespective of its position and • brought into occlusion by orthodontic treatment. 3. Surgical removal and transplantation: The unerupted canine is removed carefully without damage and • transplanted into the socket occupied by the deciduos canine by • extracting it or if it is lost by creating a socket. 4. Surgical removal : The final method in managing impacted • canine after ruling out other options is surgical removal. This is usually considered when surgical exposure and • transplantation is ruled out due to the age of the patient or • abnormal root shape etc. The surgical approach copuld be either • labial or palatal depending on the position of the tooth • determined by Clark's parallax method. Basic principles of • mucoperiosteal flaps are followed and bur is used to remove the • bone. 1. Lateral approach 2. Palatal approach 3. Surgical exposure ð 7 •3 Š Impacted Maxillary third molar : Maxillary third molar may be partly erupted or completely • impacted on several occasions. Even if fully erupted may be • displaced bucally causing cheek bite. When impacted it may assume • either vertical mesioangular and more commonly distoangular • positions. Inspite of it being impacted very frequently the upper third • molar causes symptoms less frequently unlike its lower counter • part. Reasons for removal : . Caries 2. Cheek bite 3. Rarely pericoronitis Problems encountered are 1. Limited access both visual and mechanical Access can be improved if the mouth is opened partly 2. the root of the maxillary third molar are ususally fused and • curved but occasionaly could be divergent and hooked making • removal diffiult if fractured. 3. Fracture of the maxillary tuberosity 4. Creation of oroantra fistula 5. Displacement of the tooth into the maxillary antrum 6. If there is tearing of palatal mucosa during extraction • severe haemorrage is encountered 7. To improve access a wide flap can be designed at the surface • of the second molar passing around the gingival of the second • molar and from its distal surface midpoint extended to the • tuberosity region. 8. Bone removed can be done either using chisel,gouge or bur. 9. Wound is closed usually with a single suture. 10. Post extraction infection is very rare.