Depression/Anxiety
advertisement

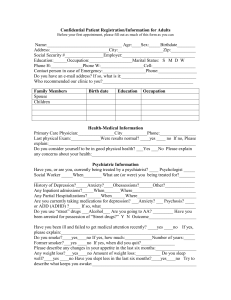
Depression and Anxiety Purpose: The purpose of this course is to provide an overview of two of the most common psychiatric disorders seen in primary care: depression and anxiety. The incidence, pathophysiology, signs and symptoms, diagnostic criteria, and treatment for each disorder will be discussed. Objectives: After completion of this course, the participant will be able to demonstrate familiarity with the pathophysiological changes in depression and anxiety identify the diagnostic criteria for depression and anxiety demonstrate familiarity with the SIG-E-CAPS pneumonic in the diagnosis of depression demonstrate familiarity with the treatment modalities for depression demonstrate familiarity with the treatment modalities for generalized anxiety disorder and other anxiety disorders demonstrate familiarity with the role of lifestyle in management of depression and anxiety Case A 32-year-old white female, who is the mother of three, presents to the primary care clinician with lack of energy, back pain, early morning wakening and irritability. She reports that she is so engrossed in her children’s lives that she has no time to do anything herself. On the rare evening that she has an evening free she chooses to go to sleep instead of going out. Her physical exam is unremarkable. Her past medical history is unremarkable except for three healthy vaginal births. She is on no medications and has no allergies to medications. Introduction Depression is one of the most common disorders encountered by the primary care clinician. Unfortunately, it remains under diagnosed and under treated. While depression has obvious implications on quality of life it can also affect quantity of life. Those who suffer from depression are more likely to commit suicide, have medical illness poorly controlled, abuse substances, lose work time and have problems in their personal lives. Anxiety is also a common medical diagnosis. Many different types of anxiety exist from generalized anxiety disorder to obsessive compulsive disorder. Death rates are higher among anxious individuals as anxiety negatively affects the endocrine and immune system. Those with anxiety also have a higher rate of suicide1. Both conditions have a negative social stigma, which partly explains why these conditions are under diagnosed. Patients and physicians are often reluctant to bring up the topic of depression or anxiety. Many times depression and anxiety co-exist. Depression affects 20 percent of women and 12 percent of men across a lifespan. Anxiety incidence is variable depending on the type of anxiety 1. Generalized anxiety disorder (GAD) 4.1-6.6% Social phobia 2.6 – 13.3% Panic disorder 2.3-2.7% Obsessive compulsive disease 2.3-2.6 Post traumatic stress disorder – 1-9.3% The prevalence of anxiety is high, one estimate proposes that 18% of primary care patients are afflicted with an anxiety disorder and around 7% are generalized2. Only 60% of those diagnosed with generalized anxiety disorder were treated in 20023. GAD disrupts the lives of about 10 million Americans4 and is often a predecessor to major depression. GAD is also associated with other mood disorders, functional impairment and alcohol and other substance dependence disorders4. The white population is more commonly affected with depression than the black population9. Panic disorder has equal incidence in the white, black and Hispanic population1. Females are more commonly diagnosed with both depression and anxiety than males. Depression rates peak between the ages of 25 and 449. Generalized anxiety disorder has its onset in the 20’s or early 30’s, but as children they are often characterized by being nervous about grades and social events. Panic disorder is most common in the late teens and early 20’s and than again the late 40’s and early 50’s. OCD is typically diagnosed in the mid 20’s to early 30’s1. Many disease states increase the risk of mental health disease. Chronic disease is associated with increased rates of depression and anxiety. Some diseases are more prone to mental health conditions than others. Chronic obstructive pulmonary disease (COPD) patients are at much higher risk for developing depression than the general population5. A recent study suggested that the risk of depression in COPD is higher than those with diabetes5. Heart disease is also linked to depression. Recent guidelines recommend that patients who have had a recent heart attack should be screened for depression regularly6. Individuals afflicted with metabolic syndrome are more likely afflicted with depression than those without the condition7. This is important to recognize as patients with metabolic syndrome need to make lifestyle changes to prevent complications of the disease and depressed patients are less likely to make these changes. Individuals with metabolic syndrome are at risk for diabetes, heart disease and stroke. Infertile couples are also noted to be at higher risk of depression and other mental health conditions. Women were noted to have more binge-eating than fertile women. Men were noted to have increased rates of social phobia and obsessive-compulsive disorder, but both conditions were noted to be subclinical8. A more lasting, but milder form of depression is called dysthymia. It can last for years before it is treated or recognized. It is diagnosed when a patient has a depressed mood on most days for most of the day for at least two years. These patients are withdrawn, pessimistic, irritable and are unable to find joy in life. Many people – including the patient themselves - mistakenly think these individuals are just this way by nature. Pathophysiology The exact pathophysiological mechanism responsible for both anxiety and depression are not known. The role of neurotransmitters is strongly implicated in the pathogenesis of both conditions. Serotonin, norepinephrine and dopamine are three neurotransmitters that have been looked at. Many factors contribute to psychiatric illness beyond the absolute level of neurotransmitters. The receptor regulation and sensitivity are also linked to mental disease. Likely there needs to be neuronal receptor regulation over time to affect mood9. The role of pathophysiology is important in the pharmacologic treatment of depression. Signs and Symptoms For the diagnosis of major depression the patient must demonstrate at least one of the following: depressed mood and/or reduction of interest or pleasure in activities. In addition, they must exhibit at least four physical symptoms such as weight/appetite changes, decrease in energy, fatigue, concentration difficulties, and sleep disturbance for a minimum of two weeks. Bereavement, general medical conditions, medications, drug or alcohol abuse cannot account for these symptoms. Bereavement is normal after certain events (e.g. death of a loved one), but symptoms should not persist beyond two months. The symptoms must result in significant impairment of social, occupational or school functioning10. A well known pneumonic is often used for the clinician to diagnose depression: SIG-E-CAPS (table 1). Table 1: SIG-E-CAPS pneumonic S Sleep disturbance – either insomnia or hypersomnia. Sleep disturbance is most commonly early morning wakening, known as terminal insomnia. Passive suicidal ideation is common with depression, which is not thoughts of suicide, but a preference to not be alive. Risk factors for suicide include: the existence of a mental health disorder (the presence of anxiety and depression increases the risk), lack of social support, substance abuse and availability of a weapon. Health care providers need to evaluate for a plan and a method to carry that plan out. Mania is important to rule out. This would indicate bipolar disease or manicdepression. To assess for this ask the patient if he/she ever feels the opposite of depressed. Do they ever feel really charged up and do not sleep or spend a lot of money? Mania is a feeling of elation that lasts greater than 3 weeks and is associated with pressured speech, decreased need for sleep, feelings of grandiosity, impaired functioning, increased activity, flight of ideas, easy distractibility and poor decision making such as excessive spending or sexual indiscretion. It is important to assess for psychosis as this may indicate depression with psychotic features or schizo-affective disorder. Ask the patient if delusions/hallucinations are present? Do they have special powers? It is also important to ask about homicidal thoughts. Depressed patients are at risk to physically or verbally attack other people. Anyone with homicidal thoughts should be hospitalized. Generalized anxiety disorder (GAD) is characterized by excessive anxiety or worry without proof or out of proportion to the given situation. The patient is in a continual state of tension and anxiety. The symptoms persist beyond six months and the anxiety is in response to various stressors. The DSM IV lists the criteria for GAD as three or more of the following symptoms - which impair normal functioning, cause distress and are not due to another medical or psychological problem - needing to be present most days for the past 6 months10. These symptoms include: irritability, sleep disturbance, fatigue, feeling restless, on edge or keyed up, lacking concentration and muscle tension. GAD affects quality of life as it impairs functioning. Patients often procrastinate, practice avoidance, have poor problem solving skills, miss work and do not maintain daily responsibilities. The physical symptoms of anxiety include: elevated blood pressure, increased respiratory and heart rate, muscle tension, and reduced blood flow to the intestines resulting in nausea or diarrhea. Tremor, shaking, furrowed brow, dilated pupils, cold clammy hands and diaphoresis may also be present. Physical findings often do not point to the diagnosis of anxiety. Needle track marks, ascites and hepatomegaly suggest substance abuse When evaluating a patient with non-specific or vague complaints, anxiety or depression must be considered in the differential. Common complaints of patients with GAD include: fatigue, sweating, dry mouth, flushing, nausea, diarrhea, urinary frequency, insomnia, weakness, irritability, restlessness and muscle tension and chills. Other conditions need to be evaluated for when anxiety is considering such as substance abuse, withdrawal, reactions to medications. Many medications may lead to signs and symptoms of anxiety. This includes prescription as well as non-prescription or illegal drugs. Common prescription drugs that may lead to signs and symptoms suggestive of anxiety include: thyroxin, theophylline, digoxin, steroids and narcotics. Amphetamines, marijuana, cocaine and withdrawal from alcohol, nicotine or sedative-hypnotics may also cause anxiety. Social conditions that may be found on history include major life events such as a death, marriage or divorce. A family history may be positive for mental illness. Medical conditions can mimic anxiety. Medical conditions to consider when anxiety is present include: chronic obstructive pulmonary disease, angina, myocardial infarction, arrhythmias, valvular disease, anemia, asthma, and hypoglycemia. Psychological testing such as the Beck Anxiety Inventory, the Hamilton Anxiety Rating Scale and the Anxiety Disorders Interview Schedule can be used in the diagnosis of this condition. When the diagnosis of anxiety is made it is important to keep other diagnoses as a consideration especially when treatments are not effective. Other clues that anxiety is not causing the issue include: symptoms starting after age 35, anxiety symptoms not related to life stressors, no avoidance behaviors and a lack of childhood history of significant forms of anxiety are clues to the need for further evaluation11. GAD should be a diagnosis of exclusion after other diseases have been ruled out. Panic disorder is associated with recurrent episodes or panic attacks. Panic attacks are short-periods of intense fear that come on very quickly. At least four symptoms must be present to diagnose panic attack including: shortness of breath, chest pain, palpitations, increased heart rate, sweating, trembling, dizziness, fainting, nausea, abdominal distress, numbness, chills or hot flashes, sensation of choking, depersonalization or fear of dying. Obsessive compulsive disorder (OCD) is a disorder characterized by obsessions and compulsions that cause distress for the person suffering from them. Obsessions are recurrent and persistent thoughts, images or impulses that cause stress and anxiety. Compulsions are repetitive behaviors carried out by the individual to reduce anxiety caused by the obsession. Phobia is a fear of something. Everyone is afflicted with specific fears, but when does a phobia become a disease. Agoraphobia is a fear of a specific item. Those with agoraphobia often fear being embarrassed by a public onset of a panic attack and often become socially isolated. Social phobias, also known as social anxiety disorder (SAD), are persistent fears in social situations that impair the ability to function socially. These situations cause the person to feel anxiety which is excessive. Post-traumatic stress disorder (PTSD) happens after a trauma that included a real or threatened death or injury. PTSD is characterized by at least one of the following: re-experienced the event; recurrent dreams; flashbacks; intense psychological distress from the previous trauma; or physiological changes when exposed to trauma cues. Diagnostic work up Ruling out other medical conditions is a critical part of the work-up of depression and anxiety disorder. Laboratory evaluation should include: Complete blood count Basic metabolic panel Thyroid function test Drug screen and urinalysis Other tests to consider based on the initial presentation may include: Liver function tests Vitamin B-12 levels Erythrocyte sedimentation rate Antinuclear antibody Rapid plasma reagin Human immunodeficiency virus testing Arterial blood gas Dexamethasone suppression test (Cushing disease) Cosyntropin stimulation test (Addison’s Disease) Electroencephalogram Lumbar puncture CAT scan of the brain Cardiovascular work up Treatment Many different treatments are available for depression and anxiety. Ideally a collaborative method is recommended for best depression treatment as this maximizes adherence, quality of life and treatment outcome12. Management should include adequate follow up with monitoring of effectiveness of treatment. The Institute of Clinical System Improvement12 recommends a team approach to depression management with the involvement the primary care physician, psychiatrist, and care manager. The primary goal of treatment is for the patient to have minimal symptoms and achieve complete remission. Additional goals include: restoration of functionality, prevention of further episodes, and prevention of a neurodegenerative process. Patients need to be active members in the treatment of their depression. Patients and families need to be educated about their disease and this is the responsibility of not only the patient, but the treating clinicians as well as the depression case manager. Ideally the involvement of a case manger would improve education and adherence to treatment. Most depressed patients are not assigned a care manager and the role of teaching, motivating the patient and assuring follow up are the role of the treating clinician. The depressed patient is a clinical challenge with treatment as the disease is often characterized by decreased energy and motivation, pessimism, and social isolation. Patients who do not understand the disease are likely to have reduced rates of treatment compliance. Patients need to understand the basics of the disease including its cause, symptoms and the natural course of the disease12. Understanding how treatment affects the disease is another critical aspect to the management of the disease. Patients need to understand that medications work over a period of weeks to months. Patients who assume that they will feel better after taking one to two doses of medication are much less likely to adhere to treatment. Understanding side effects of treatments is another critical aspect of treatment. Many side effects of medications used to treat depression are temporary and will improve as the body adapts to the medications. Knowing this may help get the patient through the initial weeks of therapy. Patients also need to understand about the discontinuation syndrome so they do not attempt to stop the medications abruptly without consulting their health care provider. Other points of education that are critical to convey to the patient include12: Signs and symptoms suggestive of relapse The amount of time treatment will take How to communicate with the health care provider Prognosis Patients should understand that depression is a very treatable medical disease and not a problem with their internal character. American society strongly stigmatizes against mental disease. Depressed patients should be treated. If active treatment is stopped, recurrence rates are high and patients should be educated about what to look out for that would indicate relapse. Lifestyle changes are primary interventions that should be encouraged in all patients. This includes activities such as exercise, nutrition, smoking cessation and alcohol restriction. Exercise is an effective strategy in the management of depression. Exercise in the depressed individual can be associated with other barriers due to the disease. These include: low energy level and feelings of guilt if exercise sessions are missed. Developing a plan that will maximize adherence is a critical aspect in the prescription of exercise. Discuss with the patient what type of exercise he/she enjoys (walking, swimming, group exercise). People comply with exercises that they enjoy much more readily. Provide information about aerobic exercise prescription guidelines so patients can derive benefits from exercise. Patients should be taught about the FITT principal. This is a pneumonic to help patients remember how to exercise aerobically. F stands for frequency, which should occur 3-7 times a week. Exercise ideally should occur most days of the week, but this is not the ideal strategy for someone who has low energy or deconditioned. Use clinically judgment to determine how often a depressed patient should exercise, encouraging them to gradually increase the number of days they exercise as conditioning and energy levels allow. I stands for intensity. The intensity is how hard one exercises during an exercise session. Multiple methods are available to gauge intensity. Patients should exercise hard enough to increase the breathing rate and heart rate, but not hard enough so they cannot carry on a conversation while exercising. More sophisticated methods to gauge intensity exist – such as monitoring the heart rate and exercising at 50-80% of the heart rate reserve (see table 2). Table 2: Determining the heart rate for exercise using the heart rate reserve method 220-age = maximal heart rate Maximal heart rate – resting heart rate = heart rate reserve (0.5-0.8 x heart rate reserve) + resting heart rate = Exercise heart rate training zone For example: A thirty year old male has a maximal heart rate of (220-30) or 190 beats/minute. His resting heart rate is at 70 beats per minutes. His heart rate reserve is therefore 190 – 70 or 120. To determine his heart rate training zone 120 is multiplied by 0.5 and 0.8 to yield: 60 and 96. To this the resting heart rate is added to yield the heart rate that the exerciser should be in during his aerobic training session. (60 + 70) to (96 + 70) or 130 to 166 beats per minute. T stands for time. Exercise should occur for at least 30 minutes during each exercise session. This may not be a realistic goal when initiating an exercise program, but should be a goal for all patients. Exercising up to 60 minutes a day is realistic in those who have the time, energy and conditioning to do so. The last T stands for type of exercise. Aerobic exercise should involve exercises that use large muscle groups such as the legs. Appropriate aerobic exercises include: walking, jogging, biking, swimming and group exercise classes. While lifestyle interventions should be recommended for all patients, the use of medications versus psychotherapy is a question of some debate. Determining the severity of the depression is a factor in determining which treatment option is recommended. For severe depression both psychotherapy and medications are recommended12. When depression is mild or moderate either option is appropriate12. Psychotherapy is effective. It often takes longer to see improvements in treatment with psychotherapy than medications. It is recommended to reconsider treatment options at 8-10 weeks before re-evaluation of the treatment. It is most effective in individuals with severe psychological or psychosocial issues. It is especially helpful in patients with chronic depression. It repairs psychosocial and occupational functioning, improves depression symptoms and prevents relapse12. One of the most popular methods of psychotherapy is cognitive-behavioral therapy (CBT). CBT is one of the more popular forms of talk therapy. This type of therapy often involves many tasks for the patient to involve themselves in, such as journaling and other home work assignments. This method has been made popular by David D. Burns in his book the Feeling Good Hand Book. Cognitive behavioral therapy looks to modify negative thought processes and behavior patterns to help the patient have more joy and less depression and anxiety. Other types of therapy include interpersonal therapy, problem-solving treatment, and short-term psychodynamic psychotherapy. Talk-therapies are an effective management strategy in the treatment of depression. Part of their benefit is that they provide regular contact with the health care system and helps the patient develop some responsibility. Medications Medications are a mainstay for the treatment of depression. All antidepressant have equal effectivness9. More important than which medication is prescribed is how well the patients adheres to therapy. As discussed earlier, education is important in the treatment of depression, it is very important when prescribing medications to patients. The length of treatment is between 6-12 months after there is a remission. Side effects may initially be more severe. As time elapses side effects often lessen. Nausea, a common side effect with many medications, tends to abate after about a week. Teaching patients to hang in there with mild side effects until the body adapts to the medication is critical to enhancing adherence. Teach patients that they will not feel better for a number of weeks. Early follow up is necessary to monitor for response at which time a dosage adjustment is sometimes needed or a change in medication is needed. Follow up must also assess for risk of suicide. Research suggests that young adults, children and adolescents are at risk of suicide after treatment with antidepressants. This often occurs after a depressed patient gets some energy back and now has the energy to complete an act of suicide. Any increase in irritability, agitation or another unusually psychiatric symptom may herald the onset of a suicide attempt and must be evaluated. Multiple medications are available for the medical treatment of depression and determining which medication to use requires evaluation of multiple factors. Evaluation of any other medications tried in the past can be helpful. A positive or negative response could steer the clinician toward or away from a particular agent. An evaluation of co-morbid medical and psychiatric conditions should be done. The clinician should evaluate other medications the patient is on to evaluate for any medication interactions. Another consideration is the provider’s familiarity with the medication. Having a complete understanding in regard to its dosing, side effects, drug interactions and clinical effectiveness may only be possible with a few medications. First line treatment for depression is the serotonin reuptake inhibitors (SSRIs). These medications work by increasing the amount of the neurotransmitter available in the brain. These are now considered first line treatment mainly because of their safety profile. The tricyclic antidepressants (TCAs) were available before the SSRIs and while effective, there were real safety concerns with these medications. Foremost, they are unsafe in overdose. This is a critical point in the depressed patient who may be at risk for suicide. Taking a handful of TCAs is likely to be fatal, while a handful of SSRIs, while not recommended, is much less likely to be fatal. TCAs, while as effective as first line agents, are not used as often due to side effect profiles. They are associated with urinary retention, blurred vision, dry mouth and constipation. They can also lead to orthostatic hypotension or cardiac arrhythmia. TCAs are broken down into secondary (nortriptyline and desipramine) and tertiary amines. Tertiary amines (amitriptyline, doxepine, and imipramine) are linked to more sedation, cognitive changes and cardiac problems such as orthostatic hypotension. TCAs are particularly effective in older patients in the treatment of depression, but there is concern over side effects. Nortriptyline is considered the best first line medication for the older adult in the treatment of depression and it should be started at a low dose, titrated slowly and monitored closely for side effects. Tertiary amines TCA should be avoided in older individuals. Fluoxetine (Prozac) was the first SSRI made available. This medication has a long half-life (5 days). This makes the medication less likely to have the discontinuation syndrome. The body naturally tapers the medication. It is dosed 20 mg once a day to start, with a maximum dose of 80 mg once a day. The doses can be split into an AM dose and a noon dose. Fluoxetine also comes in a weekly formulation as Prozac weekly, which is dosed once a week. It may potentiate warfarin, digoxin, carbamazepine and phenytoin. Fluoxetine is indicated for depression, bulimia nervosa, panic disorder and obsessivecompulsive disorder. Fluoxetine is approved for depression in children (over the age of 8) and adolescents, but it carries a black box warning (like all other SSRIs). There is an increased risk of suicide noted when SSRIs are used in depressed adolescents. Since the introduction of this warning there has been fewer cases of depression diagnosed and decreased use of the medication in adolescents. Any adolescent treated needs to be monitored closely – office visits every week for 4 weeks and than every 2 weeks for one month and than every month for the next three months. Any patient who the clinician is concerned about suicide should be referred. Sertraline (Zoloft) has more of a sedating effect than fluoxetine and may be useful in the management of an anxious depression. It is started at 25-50 mg orally every day and than the dose can be increased gradually to 200 mg per day. It may interact with cimetidine, warfarin, digoxin, and diazepam. It is indicated for depression, premenstrual dysphoric disorder, panic disorder, PTSD, OCD and social anxiety disorder. Paroxetine (Paxil) is most likely to cause discontinuation syndrome because of its short half-life. It is comes in the standard form and an extended release form the standard form is dosed 10 mg per day to start to a maximum of 50 mg orally per day while the extended release form (Paxil CR) is dosed at 12.5 mg once a day to a maximum of 62.5 mg orally every day. Paroxetine may interact with cimetidine, fosamprenavir, ritonavir, warfarin and non-steroidal anti-inflammatory medications. It is indicated for depression, premenstrual dysphoric disorder, panic disorder and social anxiety disorder. Fluvoxamine (Luvox) is indicated for obsessive-compulsive disorders but is often used off label in the treatment of depression and anxiety. The starting dose for adults is usually 50 mg once a day and 25 mg per day for children and adolescents. This medication has multiple drug interactions and notably interacts with many benzodiazepines. Citalopram (Celexa) is indicated for depression and is dosed at 20 mg once a day and the dose can be increased to 40 mg once a day after one week. The maximum dose is 60 mg once a day. The medication may be potentiated by cimetidine, azole antifungal, macrolides or omeprazole. It is antagonized by carbamazepine Escitalopram (Lexapro) is dosed 10 mg orally every day to start and it may be increased to 20 mg everyday. It is indicated for depression and generalized anxiety disorder. It interacts with carbamazepine, lithium, anticoagulants and metoprolol (increases level). Side effects of SSRIs can vary between medications, but many side effects have a class effect. Anorexia is common. Tremor and sweating also occur. Headache and nausea can occur, but both will dissipate after the body gets used to the medication. Sexual dysfunction can occur. Delay in orgasm is very common – it can be used as a potential treatment for premature ejaculation. Increased risk of suicide is the most serious side effect. There is now a black box warning for children and adolescents for this mediation. This works typically by improving mood and energy to a point where the patient has the energy to act on a suicidal plan. This is one of the major reasons that follow up is so important. Serotonin syndrome is a condition characterized by an excess of serotonin in the body. It is typically caused by an interaction of the SSRI with another medication such as cocaine, amphetamines, Monoamine oxidase inhibitor (MAOI) (the most common clinical interaction) or St John’s Wort. It is characterized by a rapid onset of cognitive changes, elevated heart rate, sweating, nausea, vomiting, hyperthermia, hyperreflexia, tremor, cognitive changes. Treatment involves stopping the medication causing the syndrome and supportive care including control of elevated body temperature, elevated blood pressure, control of agitation; control of autonomic instability and in some cases the administration of serotonin antagonists. The serotonin-norepinephrine reuptake inhibitors (SNRIs) are a newer class of medication and have three medications in this class venlafaxine (Effexor), duloxetine (Cymbalta) and desvenlafaxine (Pristiq). They effect both serotonin and norepinephrine neurotransmitters. Venlafaxine – which is indicated for depression, GAD, panic disorder and social anxiety disorder - is started at a dose of 37.5-75 mg orally once a day and than titrated up by 75 mg no more than every four days. Generally pushing the dose beyond 225 mg is not recommended in the outpatients setting. Possible drug interaction can occur with venlafaxine and alcohol, non-steroidal antiinflammatory medications, cimetidine, diazepam, haloperidol, lithium, ketaconazole, risperdal, imipramine and metoprolol. Common side effects include nausea, constipation, sweating, dizziness, somnolence, dry mouth, nervousness and sexual dysfunction including abnormal ejaculation. One notable side effect is hypertension which is not common, but can be significant in a patient with pre-existing cardiovascular disease or hypertension. Hypertension is more common with higher doses. Duloxetine is indicated for depression, generalized anxiety disorder, diabetic nerve pain and fibromyalgia. It is started at a dose of 20 mg twice a day for depression and 60 mg once a day of GAD. It may be started at a lower dose of 30 mg once a day for GAD for the body to adapt to the medication. The dose can be pushed to 30 mg twice a day for depression. It may interact with other SSRIs, cimetidine, some fluoroquinolone antibiotics and tricyclic antidepressants. Desvenlafaxine (Pristiq) is the newest SNRI medication approved for treat major depressive, generalized anxiety, social anxiety and panic disorders. The recommended dose for Pristiq is 50 mg once a day. The most common side effects are: nausea, constipation, dizziness, somnolence, anorexia, male sexual dysfunction and anxiety. Other agents used to treat depression include: bupropion (Wellbutrin), mirtazapine (Remeron) and nefazodone (Serzone). Bupropion is indicated for depression and seasonal affective disorder. It should not be used in those with a seizure disorder, bulimia or anorexia nervosa. Side effects include CNS stimulation with tremor, dizziness, difficulty sleeping, and agitation, mania, dry mouth, nausea, palpitations, sweating, hypertension. Because the side effects are very common symptoms of anxiety, those with comorbid anxiety disorder would not do as well on this medication. Mirtazapine is dosed at 15 mg per day to start and may be increased to 45 mg. It is typically dosed at bedtime because it is sedating. It may also lead to weight gain as it increases appetite. Other side effects include: dizziness, nausea, dry mouth and constipation. This drug is commonly used in nursing home residents who are depressed and are losing weight as it may encourage weight gain. Tricyclic antidepressants such as imipramine (Tofranil), amitriptyline (Elavil), and nortriptyline (Pamelor) are effective older drugs used to treat depression but are not used as frequently today because of the improved safety and side effect profiles of the newer medications. Monoamine oxidase inhibitors (MAOI) are effective but rarely used today because of the strict dietary restrictions, possible risk for hypertensive crisis and multiple drug interactions. As a result, MAOI are rarely used for patients with major depression and if they are used are used under the care of psychiatrist. Patients who are most effectively treated are those with depression with atypical features12. Early discontinuation is not recommended as it can be associated with multiple negative effects. Early discontinuation is associated with relapse or recurrence of symptoms. Early discontinuation is often self-prescribed and therefore not done properly. Discontinuation often needs to happen gradually to avoid a discontinuation syndrome. If the medication is going to be discontinued it should be tapered over 2-3 months. Discontinuation syndrome presents with flu-like symptoms, dizziness, imbalance, insomnia, nausea and hyper arousal. With abrupt discontinuation of medications the symptoms may last 1-2 weeks and sometimes longer. Cutting the dose by 25% per week is a reasonable tapering schedule, but the patient should be watched closely for any indication of discontinuation syndrome. Certain medications are more prone to discontinuation syndrome including agents with shorter half-lives, such as paroxetine, than in those with longer halflives, such as fluoxetine. Moreover, data is lacking regarding the optimal duration of treatment of depression. A conservative estimate would be 6 to 12 months of antidepressant therapy if the patient was experiencing their first episode of major depression9 13. Accordingly, any patient male or female, who is severely depressed, is having suicidal ideation or has not responded to an adequate antidepressant trial, should be referred to a psychiatrist for further evaluation and treatment. Symptoms of psychosis are an indication for an emergency psychiatric evaluation and/or hospitalization. Depression in pregnancy is a common problem. Depression can lead to risk for both the mother and the fetus and needs to be evaluated for during pregnancy. Untreated depression increases the risk of preterm labor, preeclampsia and spontaneous abortion12. Treatment of depression in pregnancy is often done with behavioral adjustment such as psychotherapy. Antidepressant therapy has not been rigorously studied in pregnancy, but is considered relatively safe. Paroxetine is the only medication that has shown some possible increase in risk12. The remaining antidepressants have shown no increase in the risk of fetal malformations, pregnancy complications, intrauterine death or behavioral toxicity12. Paroxetine is associated with a slight increased risk of cardiovascular malformations when compared to other antidepressants. This was only noticed in patients who were on paroxetine in doses greater than 25 mg in the first trimester. Another risk of depression in mothers is the risk of depression or another mental illness in their child. Mothers with untreated depression have children that have an 8% increased risk of having a psychiatric diagnosis. Children whose mothers have treated depression have a11% reduced risk of psychiatric diagnosis14. Caution should be used when prescribing antidepressants in breastfeeding mothers. Small amounts of the medication will show up in the breast milk. It is theoretically problematic when small amounts of medications show up in the neonate’s blood as their immature clearance systems may lead to higher levels in the blood. It is currently unknown if there will be any negative long-term effects on the developing central nervous system. Therefore, it is generally not recommended that breastfeeding mothers take antidepressants. Herbal treatment Herbal treatments are often tried in the management of depression. Multiple agents are available for the management of depression, but none have been rigorously studied and therefore should be used with extreme caution. Hypericum perforatum (St. John’s wort) is one of the most popular medications. Data on the use of St. John’s Wort is variable. It has not been proven to be overwhelmingly effective in the management of major depression12. Some research shows that it is as good as traditional antidepressants while some data shows that it is only minimally effective15. It is also associated with multiple drug-herb interactions. It interferes with beta-blockers, digoxin, cyclosporine, oral contraceptives, simvastatin, warfarin, fexofenadine and benzodiazepines. Side effects are not common and include allergic reactions, nausea, insomnia, restlessness, irritability, dizziness, vivid dreams, anxiety and dry mouth. It is linked to the serotonin syndrome and should not be taken when the patient is also taking a prescription antidepressant. Dosing is inconvenient with 300 mg taken three times a day. It takes about one month until effects are noticed SAM-e (S-adenosyl methionine ) is another alternative treatment used in the management of disease. SAM-e is similar in efficacy to TCAs in the treatment of major depression12. Side effects include: anorexia, nausea, constipation, dry mouth, insomnia, dizziness, nervousness and sweating. It can be given intramuscularly or orally. It is dosed between 400-1600 mg per day. Follow up Follow up should initially occur on a weekly basis. The follow up can be via phone or in person. When the patient stabilizes the follow up can be extended to every 2-4 weeks. The goal during follow up is to help the patient reach remission and at follow up appointments the medications or doses may need to be adjusted. Response to treatment can be measured on formal scales such as the HAMD or the PHG-9. A full response is a greater than 50% reduction is symptoms while a partial response is a 25-50% reduction in symptoms12. Once the patient has stabilized on the medication the patient should remain on treatment for at least 6-12 months. Some patients are candidates for continued pharmacotherapy or psychotherapy. Between 50-85% of people with an episode of major depression have a repeat episode within 2-3 years12. Some patients do not respond to the initial treatment even when the dose is pushed to the maximal dose. When there is not adequate response, other conditions must be considered such as substance abuse, bipolar disease and personality disorders. If other issues are present they must be addressed to achieve control of symptoms. Evaluation of treatment compliance is another issue that should be addressed. Clinicians often make the mistake of not pushing the dose to the tolerable upper limit. If major depression remains the diagnosis another treatment approach should be considered. Switching to different antidepressant medications may be warranted. Recent trails showed some success when therapy was switched to another medication in the same class or a different class of antidepressant medications14. Adding psychotherapy is another option to achieve a remission. Augmentation of therapy should also be considered in the management of resistant depression (discussed below). Maintenance therapy is recommended for certain groups of depressed patients to prevent another episode of major depression. Individuals who have had two previous episodes of major depression, severe depression, a family history of depression or old age at onset of depression (greater than 60) are candidates for maintenance therapy. Those with a co-morbid anxiety disorder or substance abuse disorder should also be considered for maintenance therapy. Other factors that increase the risk of reoccurrence include: unable to achieve remission, recurrence of symptoms when dose was decreased or lowered, and preexisting dysthymic. For individuals with two episodes of depression, medication should be continued for 3 years. Expert consultation Primary care providers can manage depression just as well as specialty care14. There are times that specialty care can be helpful. Patients who are candidates for psychotherapy should be referred to a psychologist or a psychiatrist with special training in talk therapy. Individuals with co-morbid psychiatric conditions such as mania, personality disorder or substance abuse should be considered for referral. Those at high risk for suicide are candidates for expert care. Resistant depression may be better managed by a mental health expert. Augmentation therapy Those who fail to achieve remission on one medication could have there therapy augmented by the addition of another medication. When augmentation is considered a referral to an expert is recommended. Augmentation often involves the use of medications that work through different mechanisms. Adding bupropion or mirtazapine to a SSRI is one strategy. Adding thyroid hormone in the form of T3 between 25-50 mcg/day may be helpful. The addition of stimulant medications may be helpful in the augmentation of someone with a low energy depression. The use of methylphenidate has been used with SSRIs, but this should not be used in those with cardiac problems or on other stimulant medications. The combination of TCA-SSRI has been used. Caution must be used as the TCA level can be elevated with this combination resulting in cardiac problems. Citalopram and sertraline result in the most modest effects12. Lithium is another agent that is used with antidepressants. Caution must be exercised as serotonin syndrome may occur with SSRIs and lithium. Recent trails suggest that lithium is not as effective as thyroid hormone14. Atypical antipsychotic medications with antidepressants are used in the management of resistant depression. Aripiprazole is approved by the FDA as an agent to augment depression. Concerns about side effects of these agents need to be considered included weight gain, glucose intolerance, akathisia and tardive dyskinesia. Other therapies Other therapies are available in the management of depression including: light therapy and Electroconvulsive treatment (ECT) therapy. Light therapy is an effective treatment for seasonal affective disorder, but it may work for other types of depression. Some evidence suggests that it may enhance the effectiveness of antidepressant medications. ECT involves shocks to the brain under anesthesia. It is one of the most effective treatments for major depression. Some patients are more suited for therapy with ECT than others, including: geriatric, co-morbid Parkinson’s disease, the patient with catatonia or psychotic features, unsuccessfully treated with other antidepressants, past history of positive response to ECT, medication compliance is questionable or in those who medications are risky. Vagus nerve stimulation uses an implantable device that stimulates the left vagus nerve intermittently. It is indicated for resistant depression. Other therapies are available but due to non-approval status and lack of evidence based many are not used. These methods include: transcranial magnetic stimulation, magnetic seizure therapy, deep brain stimulation and acupuncture. Hospitalization may occur in those who are severely depressed or those at risk to harm someone else or themselves. It may also occur when the doctor wants to closely monitor therapy, augment therapy or monitor drug levels. Treatment of Anxiety Treatment of anxiety bears resemblance to the treatment of depression. Lifestyle interventions for the management of anxiety is critical. Exercise as outlined in the depression section should be encouraged. Proper diet is helpful in the management of anxiety as it can help make the body resilient to stressful situations. Stress and anxiety increase the risk of over or under eating and the abuse of alcohol. Sleep is an important aspect to assure that the body is in balance. Many lifestyle changes should be encouraged to enhance quality sleep. Regular exercise, not eating heavy meals before bed, avoiding caffeine or alcohol before bed will assist in improved sleep patterns. Relaxing activities before bed such as listening to pleasant music, light reading, watching a light television program may help aide in sleep. Changing the way of thinking can help reduce anxiety. This often requires the help of a trained therapist, but encouraging patients to change negative thought and behavior patterns can help reduce anxiety. Patients should be encouraged to make a conscious choice to avoid anger over trivial matters and attempt to adopt a humorous outlook on life. Relapse is common upon the discontinuation of treatment for anxiety16. In order to minimize the risk of relapse, treatment should be continued for at least 12 months. When treatment is discontinued, monitoring for early warning signs of relapse is critical. A common early warning signs of relapse is functional impairment. Non-pharmacological treatments of anxiety disorders include: cognitivebehavioral therapy, interpersonal therapy, stress management, and biofeedback therapies. Psychotherapy is an effective therapy for anxiety disorders. CBT is a common and effective treatment of generalized anxiety disorder. It involves changing maladaptive thinking as well as changing behaviors. It entails the patient objectively recognizing the thoughts that fabricate and maintain anxiety and change these thoughts using techniques that change behavioral response and eradicate the anxiety reaction. The treatment can last between 3 and 5 months. Other techniques are available in the management of anxiety disorders including panic disorders such as: systematic desensitization, exposure and response treatment, modeling treatment and relaxation. Overall, relapse rates after psychological treatment are about 60 to 80 % after one year17. Medications Multiple agents are available in the treatment of GAD including benzodiazepines; buspirone; TCAs; and selective serotonin-reuptake inhibitors. Benzodiazepines - alprazolam (Xanax) and clonazepam (Klonopin), diazepam (Valium), lorazepam (Ativan), and chlordiazepoxide (Librium) - provide short-term immediate relief of anxiety. SSRIs are first line treatment options for anxiety disorders and are approved in GAD, SAD, PTSD and phobia. Difficulties with the SSRIs include a delay prior to effectiveness, usually two to four weeks, and the potential for temporary anxiety to occur initially. A combination of a benzodiazepine and an antidepressant has been used to avoid initial anxiety symptoms and hasten relief from anxiety. A selective serotonin reuptake inhibitor (SSRI) may be initiated at low doses and titrated upward for full therapeutic response in the treatment of generalized anxiety disorder. SSRIs used for the treatment of GAD include fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), and fluvoxamine (Luvox). SSRIs have similar effectiveness in the management of anxiety. Paroxetine and sertraline are equally effective for the treatment of GAD and SAD, but paroxetine may be more likely to cause weight gain16 18 19. Similarly paroxetine and escitalopram were studied with one study showing paroxetine more efficacious and the other showing sertraline more efficacious for SAD. The two drugs were found to be equally effective for GAD16 20 21. SSRIs are likely effective agents in the management of anxiety across the lifespan. Older adults with GAD respond favorably to escitalopram. In a recent study, 177 adults over the age of sixty were studied with 69% of those taking escitalopram showing reduced anxiety levels compared with 51% of placebo patients. In addition, individuals on escitalopram showed more improvement in functioning, social function and activity level. One interesting aspect of the study suggested that those treated with medication had a significant decrease in blood pressure22. Likewise children showed an improvement in anxiety symptoms when treated with SSRIs. The SSRI, sertraline, was given to children ages 7 to 17 and 55% of patients improved. This was over double the number (24%) of patients on placebo in this study who improved23. This study also looked at the effect of cognitive behavioral therapy on anxiety. It showed that 60% of patients who had cognitive behavioral therapy as a treatment for anxiety had an improvement. The most striking part of the study suggested that the combination of medication and cognitive behavioral therapy was most effective for the management of anxiety in children. Eighty-one percent of those who got this combination showed improvement23. Multiple issues – mainly dependency, abuse and side effects – limit the use of benzodiazepines in the treatment of anxiety. Side effects include daytime drowsiness, psychomotor impairment and weight gain. Patients should be cautioned not to combine alcohol and benzodiazepines. Experts differ on limiting benzodiazepines to short term use or recommending relatively long-term use in individuals with no history of substance abuse who can be closely monitored. Some authorities do not recommend benzodiazepines as monotherapy or as first-line treatments for generalized anxiety disorder4. A common problem with benzodiazepines is the loss of effectiveness over time with continued use at the same dosage. Tolerance may develop to the anxiolytic effects of benzodiazepines. Dependence can occur as early as three months. Discontinuing benzodiazepines after long periods of use may result in rebound symptoms such as sleep disturbances and anxiety, withdrawal symptoms, including stomach distress, sweating and insomnia. Venlafaxine and duloxetine are indicated for the treatment of GAD and are often chosen as first line agents in its management. Other medications used to treat anxiety include: nefazodone (Serzone), which is indicated for depression and panic disorder and mirtazapine (Remeron), a unique antidepressant known as a 5-HT2 blocker, which may be effective for generalized anxiety disorder, but is not indicated for GAD1. Azaspirones are a class of drugs proving useful in the treatment of generalized anxiety disorder. Buspirone (BuSpar) is an azaspirone that has been effective even with long-term use. It is not addictive and appears to have less pronounced side effects and no withdrawal effects. It causes fewer CNS effects such as sedation and psychomotor impairment than benzodiazepines and may be better for those patients whose work requires mental acuity. It usually takes 2 to 4 weeks to be effective9. Due to its low potential for abuse, buspirone is useful in persons with anxiety and alcoholism. Common side effects include dizziness, drowsiness, and nausea. Patients who have been taking benzodiazepines may respond less well to buspirone. Other drugs used as alternatives to the benzodiazepines and SSRIs for the treatment of anxiety disorders include the tricyclic antidepressants. Many prefer them to benzodiazepines for the treatment of generalized anxiety disorders; and they are better suited for medium or long-term therapy or when depression is also present. For people with co-morbid conditions of generalized anxiety disorder and depression, doxepin (Sinequan) has been beneficial. Imipramine and doxepin are tricyclic antidepressants with the unlabeled use for treatment of anxiety. Side effects often limit the use of tricyclic antidepressants and include sleep disturbance, orthostatic hypotension, weight gain, sexual dysfunction, and mental disturbance. Pregabalin (Lyrica) is used in the treatment of anxiety and effectively treats symptoms of GAD. It is not indicated for these uses, but is sometimes used by clinicians. It is associated with an onset of action in about one week. Interestingly it may also improve co-morbid depression. Unlike SSRIs and SNRIs it is associated with few withdrawal symptoms24. SAD is treated with medication and psychotherapy. SSRIs are first-line medications in its management. Venlafaxine is another option in the management of SAD. No agent is approved for individuals less than 18 years old, but many medications are likely effective in the under 18 year old population. Benzodiazepines, buspirone are also useful in the management of SAD. Although infrequently used, MAOIs may be used as well. The beta-blocker, propranolol, can mitigate the autonomic response in social phobia and reduce heart rate and tremor. Levetiracetam and topiramate have been studied in the treatment of SAD. They are well tolerated, although not approved for use, but are often effectively used in the management of treatment resistant SAD16. Psychotherapy, CBT, is also used in the management of SAD. Gradual desensitization, insight therapies are major parts of therapy in the management of SAD. The treatment of OCD includes medications, behavior therapy, education and family interventions. Surgery can be performed in rare cases of OCD. SSRIs, clomipramine (Anafranil) and venlafaxine are commonly used to treat the disorder. Many medications commonly used for OCD do not have an indication for OCD. Higher doses (than for depression) and up to 10 weeks is needed until effect is noticed. Most patients do not obtain a full remission, but only a reduction in symptoms with medications. The addition of CBT, with a trained psychotherapist, is helpful. An important part of therapy is the exposure and response (or ritual) prevention (ERP). Threatening situations are ranked and the person is gradually exposed to these situations with the goal of decreasing the compulsive behavior to this response. This process can be difficult and take a long time to succeed. Another important aspect of CBT is recognizing and challenging the cognitive distortions of OCD symptoms. For those individuals who do not respond to treatment should be referred for expert care by a psychiatrist for advanced medication management. . PTSD is best treated if it can be done soon after the traumatic event. Like other anxiety disorders it responds most favorable to a combination of medications and therapy (group, individual, family etc). Children and teenagers respond better to psychological therapy. Panic attacks are treated with SSRI as primary agents along with CBT. Benzodiazepines can be used for quick relief and are often used while the SSRIs take effect. They are used in some for long-term management but should only be used in cases that do not respond to SSRIs or TCAs. Clonazepam is a preferred agent as it has a longer half-life and should have fewer withdrawal effects and less dependency issues than the more commonly used alprazolam. CBT should be used with medications and may be used alone. Therapy looks at the patients distorted beliefs and looks to desensitize the patient to anxiety provoking situations. Conclusion Depression and anxiety are conditions that have significant impact on the quantity and quality of life. Identification of the disease is not complex, but both diagnoses are often missed. Regularly evaluating patients for depression and anxiety will improve identification and consequently improve outcomes. Treatments for each disease are similar and include lifestyle modifications, psychotherapy and medications. Case Study Revisited The patients was given a quick screening in the office using the SIG-E-CAPS criteria. While she denied depression she did test positive for Sleep disturbance, loss of Interest (key criteria), lack of Energy, poor Concentration, excessive Appetite and Psychomotor agitation. Based on these findings she was treated with citalopram 20 mg everyday with a follow up in 10 days. At the ten day follow up appointment she reported that she had some initial nausea, but did notice that her sleep had improved. The nurse practitioner increased her dose to 40 mg and had a follow up in one month. At the one month appointment she reported that she felt much better. She reported that her husband has made several comments on her reduced irritability. She has recently became more active in her church group. 1 Yates WR. Anxiety. 2008. (cited 2008 December 15). Available from: URL: http://emedicine.medscape.com/article/286227-print 2 Seitz DP. Screening mnemonic for generalized anxiety disorder. Canadian Family Physician 2005; 51(10): 1340-1342. 3 Healthy People 2010. DATA 2010. (cited 2008 December 26). Available from: URL: http://wonder.cdc.gov/data2010/focus.htm Fredman S. & Korn M. Anxiety Disorders and Related Conditions. 2007. (cited 2008 November 27). Available from: URL: 4 http://www.medscape.com/viewarticle/436399 van den Bemt L, Schermer T, Bor H, et al. The risk for depression comorbidity in patients with COPD. Chest. 2009;135(1):108-114 6 Green LA, Dickinson WP, Nease DE Jr, et al. AAFP guideline for the detection and management of post-myocardial infarction depression. Annals of Family Medicine 2009; 7(1): 71-9 7 Dunbar JA, Reddy P, Davis-Lameloise, N et al. Depression: an important co morbidity with metabolic syndrome in a general population. Diabetes Care. 2008; 31(12):2368-73. 8 Volgsten H, Skoog-Svanberg A, Ekselius L et al. Risk factors for psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Fertility and Sterility. 2008 Dec 30. [Epub ahead of print}. 9 Bhalla RN & Moraille-Bhalla P. Depression. 2008. (cited 2008 December 15). Available from: URL: http://emedicine.medscape.com/article/286759-print 10 American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C: American Psychiatric Association, 2000. 5 Korn M & Pollock R. Anxiety Disorders: Science and Clinical Understanding. (cited 2008 November 27). Available from: URL: 11 http://www.medscape.com/viewprogram/1974 Institute for Clinical Systems Improvement. Major Depression in Adults in Primary Care. Eleventh Edition, May 2008. Available from: URL: www.icsi.org 13 Pies R & Rodges D. The Recognition and Treatment of Depression: A Review for the Primary Care Clinician (cited 2008 November 8) Available from: URL: http://www.medscape.com/viewprogram/4572_pnt 12 Gaynes BN, Rush AJ, Trivedi MH et al. The STAR*D study: Treating depression in the real world. Cleveland Clinic Journal of Medicine 2008; 75(1): 57-66. 15 American Pharmacists Association. Popular Herbal and Dietary Supplements. 2007. (cited 2009 January 8). Available from: URL: 14 http://www.nphealthcarefoundation.org/ce/otc/ Starcevic V. Anxiety States: A Review of Conceptual and Treatment Issues. Current Opinion Psychiatry 2006; 19(1): 79-83. 16 Gliatto M. Generalized Anxiety Disorder. American Family Physician 2000; 62:1591-600,1602 18 Bandelow B, Behnke K, Lenoir S, et al. Sertraline versus paroxetine in the treatment of panic disorder: an acute, double-blinded non-inferiority comparison. Journal of Clinical Psychiatry 2004; 65: 405-413. 19 Ball SG, Kuhn A, Wall D et al. Selective serotonin reuptake inhibitor treatment for generalized anxiety disorder: a double,-blind, prospective comparison between paroxetine and sertraline. Journal of Clinical Psychiatry 2005; 66: 94-99. 20 Lader M, Stender K, Burger V et al. Efficacy and tolerability of escitalopram in 12 and 24 week treatment of social anxiety disorder: randomized, double-blind, placebo controlled, fixed-dose study. Depression and Anxiety. 2004; 19: 241-248. 17 Bielski RJ, Bose A & Chang CC. A double-blind comparison of escitalopram and paroxetine in the long-term treatment of generalized anxiety disorder. Annals of Clinical Psychiatry 2005; 17: 65-69. 22 Lenze EJ. SSRI and Generalized anxiety. Journal of the American Medical Association 2009; Jan 21. [Epub ahead of print}. 23 Walkup JT, Albano AM, Piacentini J et al. Cognitive-behavioral therapy, sertraline and their combination for children and adolescents with anxiety disorders: acute phase efficacy and safety. New England Journal of Medicine, 2008; 359(17): 2753-2766. 24 Pohl RB, Geltner DE, Fieve RR et al. Efficacy of pregabalin in the treatment of generalized anxiety disorder: double-blind, placebo-controlled comparison of BBID versus TID dosing. Journal of Clinical Psychopharmacology. 2005 ;25(2): 151-8. 21 Quiz 1) Major depression is. Self limiting *Likely to reoccur Is not associated with higher death rates Is part of a normal grief reaction 2) Which is a risk for major depression? African American *Having chronic obstructive pulmonary disease Being male Witnessing a traumatic event 3) For anxiety, benzodiazepines: Do not help with situational, short-term anxiety Are associated with alcohol abuse *Are quicker in onset of action than selective serotonin reuptake inhibitors (SSRIs) Are associated with reduced rates of depression 4) Which symptom is least suggestive of anxiety: Irritability Insomnia *Flat affect Reduced ability to concentrate 5) Dysthymia is a milder depression that tends to persist. *True False 6) Diagnostic testing for a patients with depression should include all of the following EXCEPT: Thyroid stimulating hormone levels Complete blood count *Lipid panel Basic metabolic panel 7) Which medication is the best first line option for major depression: *Citalopram (Celexa) Nortriptyline (Pamelor) Alprazolam (Xanax) Mirtazapine (Remeron) 8) When discontinuing SSRIs it important to taper them over a period of weeks. *True False 9) Tricylcic antidepressants are not used as first line medications in the management of depression because of all of the following reasons EXCEPT: Association with confusion in the elderly Risk of constipation *It is associated with increasing anxiety They are often fatal in overdose 10) Medication treatment of the first episode of major depression should last _______ after remission : *6-12 months For life Two years 3-6 months 11) SSRIs are contraindicated in patients with glaucoma. True *False 12) Which anti-depressant has the fewest sexual side effects: Venlafaxine Sertraline *Bupropion Paroxetine 13) Which anxiety is characterized by a baseless morbid fear of apparently harmless objects often leading to agoraphobia. Generalized anxiety disorder Obsessive compulsive disorder *Panic disorder Post-traumatic stress disorder 14) Depressed patients should be encouraged to: Initiate an exercise program 5-7 times a week Exercise for 10-15 minutes each session Perform weight training as a type of aerobic exercise *Encourage up to an hour of exercise a day in those whose conditioning and energy level allows 15) The A in the SIG-E-CAPS mnemonic stands for: Anxiety Agitation *Appetite changes Anhedonia 16) In teen-agers, which is the most effective treatment in the management of anxiety: Watch and wait therapy Selective serotonin treatment Cognitive-behavioral therapy *Combination therapy with cognitive-behavioral therapy and a selective serotonin therapy 17) Which SSRI is least likely associated with the discontinuation syndrome? *Fluoxetine Paroxetine Sertraline Citalopram 18) Which is linked to depression? Chronic obstructive pulmonary disease Metabolic syndrome Myocardial infarction *All of the above 19) Which medication is least likely to cause the serotonin syndrome when combined with the SSRI sertraline: *Buspirone St. John’s Wort Venlafaxine Paroxetine 20) The effects of buspirone may not be noticed for 2-4 weeks. *True False 21) Which medication is associated with the highest risk in pregnant women? Fluoxetine Sertraline *Paroxetine Citalopram 22) Mirtazapine is associated with sedation. *True False 23) Which medication is likely to interact with SSRIs? Warfarin Digoxin Cimetidine *All of the Above 24) Tapering of SSRIs should occur by _____% every week. 10 *25 50 75 25) Which of the following is NOT a symptom of abrupt withdrawal from paroxetine? *Sexual dysfunction Dizziness Nausea Hyper-arousal 26) Which medication is not recommended for the patient with anxiety? Paroxetine Sertraline Venlafaxine *Bupropion 27) Which benzodiazepine is recommended due to fewer dependency issues in the patient with panic attacks? Lorazepam Anafranil Alprazolam *Clonazepam 28) Benzodiazepines are the first-line long-term treatment in panic attacks. True *False 29) Which statement is true regarding anti-depressant medication therapy Nausea typically persists for the first 2-3 months of therapy *Improvement in symptoms may not be noticed for 4-8 weeks. Abrupt discontinuation of the medication will result in minimal side effects Monoamine oxidase inhibitors are the most effective medication used to treat depression 30) Which of the following statements about St. John’s Wort is FALSE? It is dosed three times a day *Its effects are noticed in 10 days It has multiple drug-herb interactions Should not be used with paroxetine