here - Wound Infection Institute
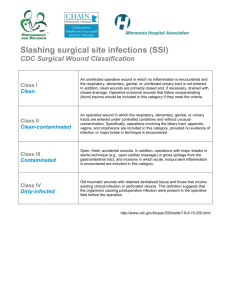
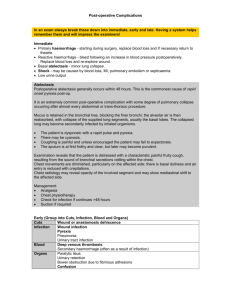
advertisement

Term Definition and comment Abscess A collection of pus ( containing live and dead neutrophils and macrophages, bacteria, fibrin and inflammatory mediators, opsonins and complement, and dead cells killed by the infective process) which has accumulated in a cavity formed by surrounding granulation tissue following an infection (usually caused by bacteria, particularly staphylococci or bacteroides, or parasites) or foreign materials (e.g. splinters, bullet wounds, or injecting needles). It is a defensive and localising reaction of the tissue to prevent the spread of infectious materials to other parts of the body. The organisms or foreign materials kill the local cells, resulting in the release of cytokines. The cytokines trigger an inflammatory response, which draws large numbers of white blood cells to the area and increases the regional blood flow. The tension within the abscess can be high and is the cause of associated pain which is relieved after drainage or spontaneous bursting The final structure of the abscess is an abscess wall of granulation tissue which is formed by the adjacent healthy cells to localise the pus and prevent infection of neighboring structures. However, such encapsulation tends to prevent immune cells or antibacterials from reaching bacteria in the pus. Abscesses tend to point to the surface and they should be drained surgically. Antimicrobials have a limited role unless there is associated spreading cellulitis or bacteraemia International Wound Infection Institute - Glossary of terms in wound infection – October 2009 Acknowledgements Antimicrobials Agents which can inhibit the growth of or kill microorganisms. These can be antibiotics (active against bacteria and given systemically), anti-fungal agents (active against fungi), antiviral agents (active against viruses) or anti-parasitic agents (active against parasites). There are also other broad spectrum antimicrobial agents such as antiseptics, disinfectants, preservatives and biocides (which are chemically derived but applied topically) Antiseptics Chemical, broad-spectrum, antimicrobial agents applied topically to skin or underlying tissues to prevent or control infection or increasing bacterial colonisation by killing or inhibiting pathogens Argyria A term that is often misused. This very rare condition produces blue-grey discolouration of the skin and is associated with long-term systemic exposure to silver salts. Argyria differs from the reversible local discolouration that may be associated with silver dressings; argyria is irreversible and can affect the skin of the entire body and the internal organs. The presence of viable bacteria in the blood. MRSA bacteramia is mandatorily reported in the UK WICP, page 10 Antimicrobial agents which destroy (kill) micro-organisms, such as antiseptics, antibiotics and disinfectants AWCN Bacteraemia Bactericidal International Wound Infection Institute - Glossary of terms in wound infection – October 2009 Bacteristatic Antimicrobial agents which inhibit the growth or multiplication of micro-organisms AWCN Bioburden The amount of contaminating micro-organisms present in tissues or on open ulcers/wounds prior to cleansing. Bioburden ranges from contamination (least) through to colonisation and infection (highest) AWCN Biofilms A layer of bacteria and/or other microorganisms on a solid or semi-solid surface, tissue or skin ulcer bound together in a bacterially-derived polysaccharide matrix (glycocalyx) shielded against the immune system and antimicrobial agents.. There appears to be a correlation between biofilms and non-healing in chronic wounds. Cellulitis A diffuse, spreading, acute infection of the skin and/or subcutaneous tissues characterized most commonly by local heat, redness and pain. There can be systemic signs of tachycardia, tachypnoea, pyrexia and raised white count and sepsis Mosby’s PDQ for Wound Care (2009). Mosby-Elsevier, St. Louis, MO. Colonisation Establishment of a community of microorganisms or ecosystem in a tissue or open ulcer healing by secondary intention, without necessarily resulting in tissue invasion or damage. WICP, page 1 Contamination The presence of microorganisms in a tissue or open wound healing by secondary intention, neither increasing WICP, page 1 International Wound Infection Institute - Glossary of terms in wound infection – October 2009 in number or causing clinical complications of infection. It is a sequel of colonisation and precedes infection in open wounds Crepitus A crackling feeling or sound detected on palpation of tissues that is due to gas within the tissues. It is not necessarily related to gas gangrene (Clostridium perfringens specific) as other infecting organisms can form gas in tissues Critical colonisation A point at which microorgansims are increasing in numbers in tissues or an open wound but not releasing virulence factors (or toxins) to cause infection. It may be related to delayed healing but is hard to define. Chemical agents whicjh are directly toxic to cells, preventing their reproduction or growth and causing cell death. This includes disinfectants which do kill bacteria but are also toxic to healthy tissues The removal of necrotic or foreign material from and around a wound to optimise wound healing. There are many different methods that can be used to debride a wound. They can be broadly classified as surgical/sharp, mechanical, biological, enzymatic and autolytic. Cytotoxic Debridement Sharp debridement is the removal of dead or necrotic tissue or foreign material from and around a wound to expose healthy tissue using a sterile scalpel, scissors or both. Mechanical debridement involves methods such as wetto-dry dressings, wound irrigation, and similar techniques International Wound Infection Institute - Glossary of terms in wound infection – October 2009 WICP, page 10 AWCN David Leaper, World Wide Wounds 2002, plus Schultz, Sibbald, Falanga et al, WRR 2003;11:128 that physically remove debris from a wound. Biological debridement broadly describes the application of sterile larvae to the wound area. Enzymatic debridement involves the topical application of endogenous enzymes. Autolytic debridement is a process that spontaneously separates necrotic tissue and eschar from healthy tissue; it occurs to some extent in all wounds. Dehiscence Delayed healing Evidence supporting one method over another is lacking. The separation of a surgical incision or sutured wound exposing underlying tissues but not necessarily exposing deep contents of a body cavity. Used in the past to describe burst abdomen or chest where all layers of a surgical wound separate with exposure of viscera It is a surgical complication that results from poor wound healing. Risk factors include infection, age, diabetes, underlying disease such as cancer, obesity, immunosuppression, poor suture or surgical technique. Healing progresses at a slower rate than expected. As a guide: ■ in open surgical wounds healing mainly by epithelialisation, the epithelial margin advances at about 5mm per week ■ clean pressure ulcers with adequate blood supply and International Wound Infection Institute - Glossary of terms in wound infection – October 2009 IWII committee WICP, page 10 innervation should show signs of healing within two to four weeks ■ a reduction in venous leg ulcer surface area of >30% during the first two weeks of treatment is predictive of healing A chronic wound might be defined as a failure to heal after 6 weeks despite optimal conditions (such as adequate debridement and dressings, pressure relief, diabetic control, adequate arterial inflow or compression in pressure, diabetic, arterial or venous ulcers) Erythema Redness or inflammation of the skin or mucous membranes that is the result of dilation and congestion of superficial capillaries. It can be caused by invasive bacteria such as -haemolytic streptococci Endotoxin A toxin that forms an integral part of the cell wall of certain bacteria (Gram negative rods in particular) and is only released upon destruction of the bacterial cell. Endotoxins are less potent and less specific than most bacterial toxins but can cause pyrexia and sepsis. Exotoxin A toxin that is released from an actively growing cell, is heat labile and often proteinaceous in nature. It has a specific target and can be used to form toxoids which are used in vaccines. Many are important virulence factors in pathogenic bacteria e.g. Panton Valentine Leukocidin (PVL) of Staphylococcus aureus which can cause a International Wound Infection Institute - Glossary of terms in wound infection – October 2009 Mosby’s PDQ for Wound Care (2009). Mosby-Elsevier, St. Louis, MO. necrotising cellulitis and pneumonia Foreign body Every foreign body has the potential to act as a nidus for infection and to impair wound healing. The majority of wound debris may be removed through meticulous, copious irrigation. However, direct visualization and removal with instruments may be required. Objects can either be inert (nonreactive) or organic (reactive). Examples of inert objects include bullets, needles, and metal objects. While these may cause chronic pain, they may not provoke an inflammatory response. Organic materials—such as wood, bone, stone, rubber, and soil— may cause infection and must be completely removed. Their presence in tissues can logarithmically reduce the numbers of organisms needed to cause an infection Genotype The genetic constitution (the genome) of a cell, an individual or an organism. The genotype is distinct from its expressed features, or phenotype. The genotype of a person is her or his genetic makeup. It can pertain to all genes or to a specific gene. Gram stain A method of differentiating bacterial species into two groups, Gram- and Gram+, based on the chemical and physical properties of their cell walls. Staphylococci and streptococci are Gram positive cocci; E.coli and pseudomonas are Gram negative rods International Wound Infection Institute - Glossary of terms in wound infection – October 2009 Atlas of Emergency Medicine Hypertrophic scar An abnormal scar in which there is excess scar tissue formed, especially across a joint surface. The reddened scar tissue does not exceed the original size the wound. Hypertrophic scars tend to regress spontaneously Induration Hardening and swelling of the skin and subcutaneous tissues around a wound due to inflammation, which may be secondary to infection. The oedema and “tumor” of inflammation Infection Multiplication and invasion of an infectious agent within the body tissues causing signs and symptoms of disease. In wound care the most common are Gram positive cocci, such as staphylococci; and Gram negative rods, such as pseudomonas Redness, warmth, swelling and pain (the Celsian rubor, calor, tumor and dolor) and decreased function (the mediaeval addition of function laesa) seen in injured, infected or irritated tissues. Inflammation is also the first mechanism used as a type of nonspecific immune response. In wound care it usually pertains to infection Inflammation Invasion The process whereby an infectious agent (in wound care usually bacteria) enters the host cells or tissues and spreads in the body (as cellulitis, lymphangitis and bacteraemia). International Wound Infection Institute - Glossary of terms in wound infection – October 2009 WICP, page 10 Keloid scar Keloids represent excess scar formation that grows beyond the borders of the original wound and does not tend to resolve spontaneously. Keloids tend to form in persons with darker skin pigmentation and can form as late as a year after injury. Lymphangitis Inflammation of lymph vessels, seen as red skin streaks running proximally from a site of infection. Most often seen with streptococcal and staphylococcal infections Micro-organism Organisms that are microscopic or invisible to the naked eye, including bacteria, fungi, viruses, and parasites Multi-organ dysfunction syndrome MODS is the presence of altered organ function in a patient who is acutely ill such that homeostasis cannot be maintained without intervention. Primary MODS is the direct result of a well-defined insult in which organ dysfunction occurs early and can be directly attributable to the insult itself. Secondary MODS develops as a consequence of a host response and is identified within the context of SIRS and sepsis. Patients with uncontrolled wound infection (e.g. in pressure sores) may develop sepsis, organ failure and death International Wound Infection Institute - Glossary of terms in wound infection – October 2009 WICP, page 10 Opportunistic Pathogen An infectious agent capable of causing disease when the hosts’ immune system is impaired Pathogen An infectious agent capable of causing an infectious disease. Phenotype The observable characteristics or traits of an organism such as morphology, development or behaviour Pathogenicity The ability of a microorganism to cause disease, also called virulence Planktonic bacteria Free floating bacteria that is not attached to a surface Prophylaxis An agent used to prevent the spread of disease or condition. Classically an antibiotic given once, IV, at induction of anaesthesia to prevent surgical site infection Purulent Containing or comprised of pus. Pus is a collection of infected material, usually living and dead leukocytes Quorum sensing A type of decision making process used by decentralized groups to co-ordinate behaviour. Many species of bacteria use quorum sensing to co-ordinate their gene expression according to the local density of their population Resistance The ability of a micro-organism to not be effected by antimicrobial agents by blocking their cellular action or by the production of an enzyme to inactivate the agent International Wound Infection Institute - Glossary of terms in wound infection – October 2009 Sepsis Defined as systemic inflammatory response syndrome (SIRS) in the presence of a known or suspected infection. The body may develop this excessive inflammatory response to microbes in the blood, urine, lungs, skin, or other tissues such as infected wounds or ulcers. An incorrect lay term for sepsis is blood poisoning, or septicaemia;both terms are now redundant American College of Chest Physicians/Society of Critical Care Medicine Consensus Panel Similar syndromes may follow burns or pancreatitis with the systemic response to endotoxins and expression of cytokines Multiple organ dysfunction syndrome (MODS) may result (eg, lactic acidosis, acute respiratory distress syndrome, oliguria, obtundation). Septic shock is refractory hypotension in addition, despite adequate fluid resuscitation Surgical site infection Definitions of surgical site infection include: Superficial incisional SSI: Infection involves only skin and subcutaneous tissue of incision. Deep incisional SSI: Infection involves deep tissues, such as fascial and muscle layers. Organ/space SSI: Infection involves any part of the anatomy in organs and spaces other than the incision, which was opened or manipulated during operation. International Wound Infection Institute - Glossary of terms in wound infection – October 2009 Centers for Disease Control (US) Systemic Inflammatory Response Syndrome Systemic inflammatory response syndrome (SIRS) may follow a variety of clinical insults, including infection, pancreatitis, ischemia, multiple trauma, tissue injury, hemorrhagic shock, or immune-mediated organ injury. It is defined as two of: Tachycardia >90 beats/min; Tachypnoea> 20 breaths/min WBC >12x 109/l or <4x109/l; temp >38oC or <36oC Tensile strength The tensile strength of a wound is a measurement of its load capacity per unit area. The bursting strength of a wound is the force required to break a wound regardless of its dimension. Bursting strength varies with skin thickness. Peak tensile strength of a wound occurs approximately 60 days after injury. A healed wound only reaches approximately 80% of the tensile strength of unwounded skin. Virulence Virulence is the quantitative or relative ability of the agent to cause disease WICP = Harding et al, Wound Infection in Clinical Practice, MEP 2008 International Wound Infection Institute - Glossary of terms in wound infection – October 2009