Immunopathology I
advertisement

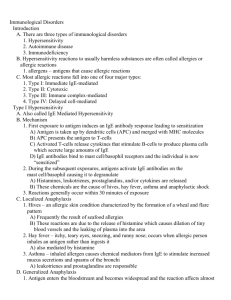
CLASS: 11:00 – 12:00 DATE: November 18, 2010 PROFESSOR: Bucy I. II. III. IV. V. VI. IMMUNOPATHOLOGY I Scribe: Adam Baird Proof: Page 1 of 7 IMMUNOPATHOLOGY I [S1] a. Immunopathology encompasses the mechanisms by which an immune response causes tissue injury and how that tissue injury can then lead to disease. There are many different pathways by which this can occur. b. Terminology and definitions: 1. “Immuno” refers to the adaptive immune system (T-cells, B-cells, etc.). 2. “Inflammation” refers to a non-antigen specific (innate) inflammatory mechanism. c. There are three classifications that the different adaptive immune response mechanisms are categorized into. We will discuss these groups in more detail later. NO TITLE [S2] a. Prime test questions: 1. Matching up these features (namely the name of the process, how fast the response occurs, what the immune mechanism is, disease that result from these mechanisms). You need to know how everything fits together. This may show up on the test in the form of a matching question or a multiple-choice question. TYPE I HYPERSENSITIVITY [S3] a. The first category is called Type I, also known as the “anaphylactic type” or “immediate hypersensitivity”. It is immediate because a skin test response (a way to distinguish between these processes) is accomplished by putting an antigen into the skin, usually as in intradermal injection. In Type I hypersensitivity, this occurs in approximately 10 minutes. It’s considered immediate. b. Type I hypersensitivity is understood to be synonymous with the activity of the special class of immunoglobulin, IgE (which behaves differently than the other classes of immunoglobulin). c. IgE is cross-linked (bound) to special cell-surface receptors, called the FCε receptor, which is primarily on mast cells that surround small blood vessels. d. The normal role of IgE is thought to be the immune defense against large parasites (like worms, for example). Many of these parasites are water-borne. The US doesn’t have many of these (because of our clean water supply), but other countries do. The normal function of IgE is not very relevant in modern medicine in the US, but it can be a nuisance. e. The best therapy for Type I hypersensitivity is to get rid of the antigen. Symptoms can be treated, but that only have marginal effects. The antigen itself is what is causing the problem. IMMEDIATE HYPERSENSITIVITY (TYPE I) [S4] a. When the IgE-specific antigen binds to the mast cells, it cross-links at 2 or more molecules of the IgE, which therefore drag the FCε receptors closer together on the cell surface. This interaction, then, initiates a signal cascade resulting in degranulation of the contents of the mast cells. The degranulation, in turn, results in a number of different pharmacologic activities. Very little IgE is present in the plasma or blood circulation though; all of the IgE is bound to tissue cells. b. Like other types of immunoglobulin, IgE comes from B-cells that are induced with specific antigens and CD4 T-Cell help. IL4, in particular, is critical in this process. For example: As mice that are knocked out will have a genetically-induced mutation of IL4 genes, meaning that they can not produce any other IL4 genes, nor can they produce any more IgE. c. The reason why certain antigens cause IgE formation (whereas other antigens don’t) is still unknown. It may have to do with the fact that some mast cells can actually produce Aisle 4, therefore driving an inflammatory response that initiates a positive feedback loop. NO TITLE [S5] a. The interaction between the IgE and mast cells primarily releases vasoactive amines (amines that affect the diameter of blood vessels, and thus blood pressure). This interaction also releases histamine as the chief pharmacological mediator in the granules of mast cells. There are many different granule contents though (like proteases, chemotactic factors, and arachidonic acids, which then give rise to leukotrienes and prostaglandins). b. Non-steroidal anti-inflammatory agents tend to block this process. Antihistamines (like Benadryl, for example) block the action of histamine, not at the degranulation of a mast cell, but at the level that histamine interacts with its target cells. c. Antihistamines are “less useful” though, because they also affect the CNS (causing drowsiness, for example). It cannot, therefore, be used a sufficient dose to completely overcome potentially serious Type I hypersensitivity. NO TITLE [S6] a. If the antigen is injected into the skin (via intradermal injection), an immediate response occurs, which involves degranulation of mast cells. This, in turn, causes vascular congestion via chemoattraction of CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 18, 2010 Proof: PROFESSOR: Bucy IMMUNOPATHOLOGY I Page 2 of 7 eosinophils and fluid leakage into the interstitial space (because the endothelial cells of small blood vessels open up and mucous production is stimulated). b. This is why, if a patient has Hay Fever (which is an example of Type I hypersensitivity), their nose will clog up, they will have stimulated mucus production, and their sinuses will be swollen. VII. NO TITLE [S7] a. This is a dust mite. b. The feces of the dust mite have a protein that is particularly antigenic and stimulates IgE responses. c. Many people are “allergic to dust”, so they say, but they are actually allergic to the dust mite. It’s difficult to get rid of dust though, because dust is everywhere (carpets, pets, furniture, etc.). Ragweed antigen can set off IgE production too. d. Antigens can be injected into the skin to observe what the patient might be sensitive to, all in hopes to inhibit the IgE response. VIII. TYPE II HYPERSENSITIVITY [S8] a. Type II hypersensitivity is also called the “antibody mediated cytotoxic type”. It involves two distinct mechanisms (and a third mechanism that is sometimes included in this group). 1. Ab coating of cells: a. The antibody coats macrophages, granulocytes, and other kinds of inflammatory cells via specific FC receptors (similar to how mast cells bind to IgE). The antibody mediates phagocytosis of bacteria. So if the antibody covers the bacteria, for example, then the inflammatory cells can engulf the bacteria and digest it much more avidly than they can normally. b. ADCC is when a coated macrophage kills a target cell based on the presence of the antibody. The antibody delivers the specificity component of the killing, but the cell mediates the actual lysis by secreting granules that destroy the target cell. 2. Ab plus complement: a. This results in the direct lysis of cells. It is thought to occur with RBC and other similar targets. 3. Ab interaction with cell surface receptor: a. This results in the stimulation or inhibition of the bioactivity mediated by the cell’s surface receptor. b. It is an antibody-mediated mechanism (not of the IgE class and not of the immune complexes though) that can cause disease or other abnormalities. IX. NO TITLE [S9] a. The previous mechanisms are illustrated in this figure. 1. Opsonization and engulfment of a target cell based on the presence of antibody complement mediated lysis. Which involves a series of proteins that results in the lysis of the target cell as well as the activation of neutrophils and the release of their mediators. 2. Antibody-mediated cellular dysfunction is observed in two contexts: a. Thyroid: TSH receptors b. Grave’s Disease: Antibodies to the acetylcholine receptors (which mediates a disease called myasthenia gravis). X. EXAMPLES OF ANTIBODY-MEDIATED DISEASES (TYPE II HYPERSENSITIVITY) [S10] a. We won’t talk about everything on this chart, but it’s an important chart to review. XI. TYPE III HYPERSENSITIVITY [S11] a. Type III hypersensitivity, also known as the “immune complex type”. b. The main idea here: antibodies interact with an antigen that is soluble. 1. The antibody-antigen complexes form and obtain a particular size and overall charge (usually multiple molecules of the antibody + multiple molecules of the antigen). The availability of the antigen and antibody determines the size of the complex. If there are more antibodies than antigens, the particles get coated with one antibody molecule per target and a complex isn’t formed (a complex wouldn’t be formed if there was more antigens than antibodies either). It’s dependent upon the correctly balanced physical ratio of the antigen and antibody. If the antibodies stick very tightly, there will likely be large complexes. If the antibodies are loose, however, the complex will likely fall apart. The disease course and characteristics, then, depends on the physical chemistry of the aggregates. Sometimes, the antibodies deposit in a particular anatomical site and the antibodies deposit in that site, causing immune complex disease (not because there are immune complexes in the blood stream or plasma, but are strictly localized in the tissue). 2. The immune complex deposition is in vessel walls and glomeruli (kidney). They can involve complement deposition and neutrophil activation. CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 18, 2010 Proof: PROFESSOR: Bucy IMMUNOPATHOLOGY I Page 3 of 7 3. A skin test of antigen peaks at about 10 hours. This particular skin test is called the Arthus reaction. XII. NO TITLE [S12] a. This is a picture showing the processes. b. The antibodies and antigens are in the circulation. An antigen that is typically invoked is Hepatitis B core antigen (a chronic viral infection of the liver that doesn’t totally destroy the liver, but produced chronic levels of antigen in the blood stream). The antibodies, then, cannot clear the antigens because the liver is producing the antibodies – so the correct ratio can be maintained over an extended period of time, resulting in the accumulation of an immune complex injury. c. The complexes will eventually precipitate into the blood vessel wall, activating complement and cells that have FC receptors. Granulocytes, then, are tricked: they think they are recognizing bacteria that are covered with antibody, but it is instead an immune complex that is deposited to another antigen. d. Some of the cleave complement components are chemotactic (meaning that they recruit other inflammatory cells to the local site). This process continues, and hopefully the antigen goes away. However, persistent antigen concentration can lead to significant vasculitis. XIII. IMMUNE COMPLEX DEPOSITION IN THE KIDNEY [S13] a. They also deposit in the kidney. b. Exactly what kind of glomerulonephritis (inflammation) is present depends on the size of the complexes. If the complexes are small, they deposit on the endothelial surface (notice the blood on the inside, urine on the outside), which will cause a specific kind of nephritis of the glomeruli (called membranous glomerulonephritis). c. They can also deposit inside the basement membrane or on the epithelial surface. d. Sometimes, diseases like systemic lupus (autoimmune disease where the regulation of antibody production is not functioning properly) result in antibodies multiply tissue antigens. This can lead to deposits in multiple places depending on the type of antibody involved. e. f. XIV. THE ARTHUS REACTION [S14] a. The Arthus reactions works by the artificial injection of an antigen. b. It takes a while for antibodies in the circulation to bind to the antigen. Once they are bound, though, it activates complement and polymorphonuclear cells, which releases chemoattractant molecules, potentially causing degranulation of mast cells and ensuing inflammatory response. XV. NO TITLE [S15] a. This is a picture of the Arthus reaction. b. The skin is red because blood flow has increased. c. There is a bump because fluid is leaking out of small vessels, leading to inflammation. d. The complement factors (that are released by inflammatory factors) stimulate nerve ending that cause pain. XVI. NO TITLE [S16] a. This is a histological picture of what the Arthus reaction looks like. b. Notice the granulocytes in the lesion (as opposed to lymphocytes and macrophages, which would be considered Type IV hypersensitivity). c. Notice cell wall of the blood vessels. Notice that it also is filled with granulocytes. d. Notice the muscle throughout. e. Notice that the inflammatory lesion goes through the dermis and into the muscle. XVII. EXAMPLES OF IMMUNE COMPLEX-MEDIATED DISEASES [S17] a. Theses are examples of diseases that are associated with particular antigens. XVIII. TYPE IV HYPERSENSITIVITY [S18] a. Type IV hypersensitivity, also known as the “cell-mediated type”, is classically involved in “delayed type hypersensitivity”, which got its name from a delayed skin test, usually peaking from 24-48 hours (as opposed to 10 hours with the Arthus reaction Type III hypersensitivity or opposed to 10 minutes with Type I hypersensitivity or opposed to Type II hypersensitivity, where there isn’t a skin test involved). This delayed type hypersensitivity is now known as a response driven by CD4 T-cells as they recognize the specific antigen releasing cytokines (particularly γ-interferon and TNFα). b. These cytokines activate endothelial cells to make them more leaky and to increase expression of adhesion molecules, so that other leukoctyes stick to the spot in the endothelium and migrate out into the tissue. c. These cytokines also activate macrophages that come into that location. These macrophages release more cytokines and chemokines that auto-propel that lesion. d. A pathologically distinct form of Type IV hypersensitivity is called granulomatous inflammation, in which the antigen doesn’t go away. Typically, delayed hypersensitivity goes away after 24 hours, for example, and last maybe 72 hours. The hypersensitivity stops once the antigen that has been injected gets cleared (once the CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 18, 2010 Proof: PROFESSOR: Bucy IMMUNOPATHOLOGY I Page 4 of 7 macrophages digest it and make it into amino acids that are no longer stimulatory for the T-cell, then the whole response comes down). If the antigen is hard for the macrophages to digest (like fungal cell walls, for example), then the macrophages can’t completely clear the material, the T-cells continue to get stimulated though, and the process develops a particular type of morphology of a granuloma formation (which is basically an organized collection of macrophages) e. Cytotoxic T-lymphocytes (CTL) delivers a distinct type of cell-mediated immunity, which is typically of the CD8 cell class (as opposed to CD4 cell class that is primarily responsible for DTH). The CTLs directly kill target cells that involve the T-cell antigen receptor mediated lysis at the final stage of delivering the “lethal hit”. f. Examples: skin lesions of contact sensitivity, where T-cells mediate the lysis of individual epithelia cells that have an antigen on them. g. NK cells activity is usually included in cell-mediated immunity. NK cells do not have a T-cell receptor or B-cell receptor immunoglobulin, but are driven by IL2 production (which is usually at a low supply in vivo. In certain types of viral responses though, NK cells may dominate in the response. h. It is very technical and difficult to demonstrate T-cell reactivity, whereas it is relatively straight forward to measure antibody activity (because that simply involves two simple things binding together, which is easily detected). T-cells have to be alive. The antigen has to be at an appropriate level. The antigen-presenting cell has to be alive. The entire thing has to occur in a hospital environment. It takes 24-48 hours for it to even occur. XIX. NO TITLE [S19] a. This diagram (and the diagram on the next slide too) illustrate the responses of CD4 T-cells: 1. How it recognizes an antigen 2. How the CD8 T-cells can recognize these antigens and often kill normal cells off the epithelia 3. How the cytokines (produce by either of these previous cells) can activate granulocytes, macrophages, endothelial cells, etc., which together, can combine to damage tissue. 4. How the CTLs can directly kill the target cells without the mediation of macrophages and cytokines XX. NO TITLE [S20] a. The entire sequence involves a “round about” process. The antigen-presenting cell and T-cells often interact initially in the lymph nodes. Then cells enter the circulation, find cells in the periphery and then initiate the inflammatory response (which involves cytokine production by the CD4 T-cell in the tissue) that mediates chemotaxis and ultimately, tissue destruction and injury. XXI. NO TITLE [S21] a. Positive TB skin test, also called purified protein derivative (PPD) from Dr. Bucy (after doing an autopsy on a patient who unknowingly had TB). b. The PPD takes an extract of the mycobateria organism and injects in into the skin, resulting in a classic DTH response. This is the test to see if someone has TB. c. TB is a disease that can cause harm even with a very low organism load; therefore, the mycobacteria can’t always be detected in the beginning form of the infection. XXII. NO TITLE [S22] a. Notice the squamous epithelium on both sides. Notice the “foamy” stuff down the middle (cartilage). b. This is the ear pinna of a mouse. c. An experimental way to measure DHT: inject antigen into one ear and saline into the other ear, and then measure the thickness of the ear pinna 24 hours later, for example. A strong response would have redness and inflammation. d. Notice where the antigen was injected. Notice the collection of lymphocytes and macrophages with vascular activation. The edema, with the cellular infiltrate, is what is measured as the thickness. XXIII. GRANULOMATOUS INFLAMMATION [S23] a. Granuloma inflammation involves aggregation of macrophages with fibrosis. Notice the globs of tissue that organize together. Sometimes they have an active state for so long that they fuse together, leading to epithelia giant cells (which have several nuclei in one cell). Sometimes these giant cells can be found in granulomatous lesions; other times though, they’re not seen. XXIV. EXAMPLES OF T-CELL-MEDIATED (TYPE IV) HYPERSENSITIVITY [S24] a. We’ll talk about these tomorrow. XXV. RELATIONSHIP OF ANITBODY VS. CELL MEDIATED HYPERSENSITIVITY [S25] a. There is a radical difference in the assay’s detection methodology for antibodies versus cell-mediate hypersensitivity. In a strong response, both are present. Therefore, the presence of antibodies basically act as markers for specific T-cell mediated activation. b. What is the primary way to prove what is responsible for a particular lesion? Passive transfer; if a purified antibody is injected into a test organism, and the symptoms of the disease are reproduced, then it’s evident that the disease is antibody-mediated. On the other hand, in experimental situations, there are cases where CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 18, 2010 Proof: PROFESSOR: Bucy IMMUNOPATHOLOGY I Page 5 of 7 the disease can be transferred by activated T-cells (free of any antibody). Infusion of those cells into the test organism can cause the same kind of symptoms. c. Note: Experiments where T-cells are transferred from one individual to another is not done on humans (because there are many problems and issues that may arise). In animals models though, there may be a hint that T-cells are involved, but it can’t truly be equally confirmed for humans. XXVI. CLASSIFICATION SCHEME (MECHANISM VS. ANTIGEN) [S26] a. One way to classify immune responses is by focusing on the mechanism. The problem with that, though, is that not all of the mechanisms are known. Historically, lymphocytes were not separated into any subclass (Tcells and B-cells were just considered lymphocytes). Everything that was not antibody-mediated was clumped into the cell-mediated group (Type IV). b. In actual diseases, there is an overlap between formation of antibodies, immune complexes, T-cell activities, etc. Although one disease may be associated with one mechanism, but oftentimes, there may be other diseases or mechanisms involved. Remember: the classification scheme is man-made, so it has some imperfections. c. An alternative way to consider these immune responses is to consider the antigen that is driving the reaction. The idea is that the kinetic course of antigen is a key regulator of how that immune response works. One of the problems, though, is that we don’t know the specific antigens. XXVII. LEPROSY [S27] a. We’ll now talk about a few immune responses. The first type we will discuss is infection. A good example of this is leprosy (because there are two diseases, but only one infectious organism, microbacterium leprae). b. Tuberculoid leprosy is an intense immune response with low organism load. c. Lepromatous leprosy is a suppressed immune response with high organism load. This may sometimes lead to disfigurement. d. These two forms result from the response to the infection itself, not the nature of infection. Lepromatous leprosy, for example, may affect different people in different ways. This illustrates the importance of the pathway of a host interaction with the organism. XXVIII. NO TITLE [S28] a. This is a picture of tuberculoid leprosy. b. Notice the lymphocytes. c. Notice the nerve ending. The organisms like to grow in peripheral nerve ending. The immune response to the organism damages the nerves, resulting in symptoms relating to end-organ destruction. XXIX. NO TITLE [S29] a. This is a picture of lepromatous leprosy. b. Notice the lymphocytes. c. Notice the big, foamy macrophages, which are filled with the mycobacterial organism. XXX. NO TITLE [S30] a. Notice that this is an acid-fast stain. Each red rod is an infectious agent (with symptoms occurring on the face, skin, etc.). It is infectious because of the high organism load. XXXI. CONTACT DERMATITIS [S31] a. Contact dermatitis is an environmentally induced antigen exposure. b. In this case, it is exposure to the skin to agents that tend to from covalent bonds with the skin cells, immunizing T-cells. The second exposure is known as eczematous eruption or rash (due to the immune response to the skin tissue). c. The resulting lesion is a mononuclear infiltrate, epidermal spongiosis (intracellular edema), and vesicle formation (bullae). d. Exposure to poison ivy is a common example of this process. e. Another example of this process is benzoin (found in disinfectant betadine, which some people may be allergic to). This is why it is important to get medical history of patients (especially of their allergies). XXXII. NO TITLE [S32] a. This patient got a benzoin rash (on her finger and her mouth, but nowhere else). She only got a rash where the benzoin touched. XXXIII. NO TITLE [S33] a. This is a histological picture showing the T-cell inflintrates in the dermis and epidermis. b. Notice the small blisters (bullet formation). c. Notice the intracellular edema in the epithelial level, which is why the skin weeps fluid; it is very wet and crusty because the skin is being disrupted and no longer provides the barrier to fluid for escaping. XXXIV. NO TITLE [S34] a. This is picture of poison ivy. b. This is an immune response to a toxin. CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 18, 2010 Proof: PROFESSOR: Bucy IMMUNOPATHOLOGY I Page 6 of 7 c. Patients don’t get a reaction to poison ivy the first time they are in contact with it, but the second time (because the immune response then acts accordingly). XXXV. PENICILLIN ALLERY [S35] a. Penicillin is a typical allergy that causes an immune response to an epitope associated with the drug. b. There can be different types of allergies (based on the dosage, for example). c. It can lead to conjugation of RBCs, resulting in hemolytic anemia (because the clearing of the immune response clears the cells that have been conjugated to the drug. d. Penicillin is common allergan because it is an active molecule with proteins (which is part of its antibiotic activity, because it is that bacterial protein that inhibits bacteria. Antibiotics that mediate that type of activity can induce an allergic response (like in this example with penicillin). XXXVI. TUMOR ANTIGENS FOR CD8+ T-CELLS [S36] a. A certain type of antigen that the immune response will attack is a tumor antigen, which may involve response to normal self-proteins (which, in this case, T-cells are tolerant to). In most cases, the proteins (antigens) in a normal cell will not have an immune response. If the cell becomes a tumor, another protein may be formed, which may cause an immune response. That new protein, though, is usually in low concentration. The activation to these tumor antigens occurs, but is not the dominant pathway (althougth this is still being heavily researched). b. When a virus is directly oncogenic to cells (like HPV, for example, which infects the cervical epithelial cells and gives rise to squamous cell carcinoma of the cervix. Most cervical cancers are caused by this mechanism. So if people are immunized to the virus in a regular immunization, so that they don’t get affected, then that can prevent the oncogenic transformation of the cells later on. The vaccine (like Gardisil, for example) is produced by Merck and is recommended for girls before they have ever been exposed to HPV, so that the immunity can block the initial exposure. It takes 20 – 40 years for the virus to result in a cancer. XXXVII. ORGAN/TISSUE TRANSPLANTS [S37] a. A tissue transplant is another situation where an immune response can cause damage to foreign antigens (but not to the normal tissues) because the antigens from someone else are not the same antigens that another person has (so there is a lack of tolerance). b. The target of tissue transplant control much about the immune response’s activation. c. The cornea, for example, which has a weak and low level of immune response and topical steroids usually are sufficient to block transplant rejection. d. The liver and smaller bowel, on the other hand, are quite immunogenic and it is difficult to control transplant rejection because there is so much lymphoid tissue that is involved, which in turn causes inflammation responses. e. The heart, as well, has some interesting transplant characteristics. If the transplanted heart is rejected, the patient dies. Whereas if the patient rejects the kidney, for example, the patient can survive off dialysis. Another interesting point: heart transplants typically have less inflammation than kidney transplants. f. There is a special kind of antigen presentation that is not typical of the normal pathway, commonly called indirect presentation. XXXVIII. ALLOANTIGEN RECOGNITION [S38] a. Potential test material: The definition of indirect recognition is that the donor contributes the peptide and the antigen-presenting cell is from the host. The T-cell receptors (grown in the thymus) with that particular MHC antigen and a peptide (that came from the donor tissue) stimulate that response. Direct recognition, however, the donor contributes the antigen-presenting cell. A lot of different peptides could fit in the altered MHC molecule (the normal MHC for the donor). In the recipient, that MHC molecule is not what the T-cell expects though, and therefore, there is a high frequency of T-cells that respond to this kind of donor antigen. This pathway exists between donors and recipients of the same species, but the more distantly related the species is, the less indirect response there will be (because the MHC molecules changes so much that the T-cells are not fooled). XXXIX. MECHANISMS OF TRANSPLANT REJECTION (CLASSICAL) [S39] a. There are a couple mechanisms of transplant rejection: 1. Antibodies that are preformed that can cause hyperacute rejction (anti-MHC or anit-endothelial antibodies) are made immediately. With correct cross matching, it rarely occurs today. 2. Acute vascular rejection is thought to be when antibodies attack the vessel, but because the levels are initially low, the transplant induces the formation of those antibodies (which takes about a week and a half). 3. Acute cellular rejection involves the DTH process where CD4 cells release cytokines and CD8 cells kill target cells. 4. Chronic rejection is a compromise that occurs months or years after a transplant. The specific mechanism, though, is still unknown. CLASS: 11:00 – 12:00 Scribe: Adam Baird DATE: November 18, 2010 Proof: PROFESSOR: Bucy IMMUNOPATHOLOGY I Page 7 of 7 XL. MECHANISMS OF TRANSPLANT REJECTION (MODERN) [S40] 1. Cytotoxic damage endothelial cells with coagulation are the mechanism of the hyperacute rejection. 2. DTH and CTL are acute cytorejection. 3. Antibody-mediated injury to endothelia can be associated with acute vascular rejection. b. All of these, in a low state cause chronic rejection. XLI. NO TITLE [S41] a. This is a diagram showing glomerulopathy, which is thought to be mediated by antibodies to glomerulial capillaries and can result in decreased creatinine from the transplanted kidney. b. This is acute rejection. Notice the individual lymphocytes (that go through the basement membrane and are killing the epithelial cells of the tubules). This is a process of acute vascular rejection of many cells in the vascular endothelium. c. Chronic rejection, on the other hand, is caused by damage to the endothelium, leading to scar formation in the lumen of the vessel. Notice how small the lumen of the vessel is now. Most of the cells, then, die due to ischemia. XLII. CLINICAL MONITORING OF ALLOGRAFT REJECTION [S42] a. The immune response is not measure to determine the rejection (because it doesn’t help here). Instead, the target damage is used to measure the rejection. 1. Kidney and Liver – There are substances in the blood. For example, creatinine (which measures renal function), or bilirubin and transaminases (which indicate hepatic function, meaning that when those levels increase in the blood, there is active damage to the organ). Blood tests are sufficient to monitor this. 2. Heart – Heart transplants don’t have a serial marker like kidney and liver. If you wait for the BP to fall, the damage is too far along and the rejection has begun. Blind biopsies help identify if any rejection is occurring, because sometimes it can go unnoticed without the signs of symptoms. 3. Lunge – Pulmonary function tests help monitor rejection, as do biopsies. 4. Pancreas – There really isn’t a good method to monitor how well the transplant it. However, the pancreas and the kidney are often transplanted together, so any rejection may be noted by observing the other organ. XLIII. NO TITLE [S43] a. Know the four immune responses (mechanisms, antibodies, etc.) XLIV. [End 52:27 mins]