PAF article (2)
advertisement

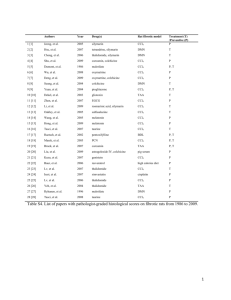
Effect of Selected Natural Products, Thioproline and Pegasys® on Hepatic Platelet Activating Factor (PAF) in CCl4-induced Hepatic Fibrosis In Rats Farid A. Badria1 and Hala A. Attia2* 1 Department of Pharmacognosy, 2Department of Biochemistry, Faculty of Pharmacy, Mansoura University 35516, Mansoura, Egypt. * To whom correspondence should be addressed. Abstract This study aimed to estimate hepatic levels of platelet activating factor (PAF) in liver fibrosis induced by CCl4 in rats. A group of selected natural products; boswellic acids, curcumin and glycyrrhizin (preparation named OMNI ® ; a drug under clinical trials for treatment of hepatitis C virus), Mirazid ® (a commercially available schistomicidal drug), Thioproline (a commercially available hepatoprotective agent) and Pegasys® (peg interferon alpha-2a; a commercially available therapy for treatment of hepatitis C virus) were examined for their effect on hepatic PAF after CCl4 intoxication. For this purpose, 54 rats were used in the study. Rats were divided into 6 groups each comprised 9 rats. Group 1 was treated only with CCl4, groups 2 to 5 were treated with OMNI®, Mirazid®, Thioproline and Pegasys®, respectively, whereas the sixth group was the normal control group (with no treatment, except an injection of the vehicle). Liver damage was induced in all groups except normal control group (groups 1 to 5) by i.p. injection of 40% CCl4 in corn oil (0.375 ml/kg) 3 times a week for 3 weeks. One week after CCl4 intoxication, all tested drugs were injected i.p. daily for 3 weeks. Hepatic PAF concentration was estimated by HPTLC (high performance thin layer chromatography), while, levels of serum transaminases (ALT, AST), hepatic hydroxyproline (as markers of liver fibrosis), serum malondialdehyde and catalase (as markers of oxidative stress) were estimated spectrophotometrically. The hepatic PAF levels were significantly higher in CCl 4 group (24.24±2.01 pmol equiv./mg) as compared to normal control (8.81±1.09 pmol ® ® equiv./mg) (p<0.001). Treatment with OMNI , Mirazid , Thioproline and Pegasys® reduced hepatic PAF significantly to be 11.84±0.22, 14.5±1.00, 13.17±0.54 and 14.26±1.09 pmol equiv./mg, respectively. This study may add further rational to the anti-fibrotic activity of the tested drugs via reduction of hepatic PAF. Key words: platelet activating factor (PAF), OMNI®, Mirazid®, Thioproline, Pegasys® and liver fibrosis. -1- Introduction Platelet activating factor (PAF:1-0-alkyl-2-acetyl-sn-glycero-3phosphocholine) is a potent pro-inflammatory phospholipid which exerts diverse biological activities including platelet secretion and aggregation, hypotension, bronchoconstriction, increased vascular permeability and stimulated synthesis of mediators such as eicosanoids (1-6). PAF acts as a mediator of inflammation, allergic reactions and shock and as a specific membrane bound adhesion molecule (6-8). The PAF content of the intact liver is elevated by various types of injury including ischemia reperfusion (9), endotoxin exposure in vivo (10) and obstructive jaundice (11). Plasma and liver tissue PAF levels are increased in experimental obstructive jaundice and activation of this mediator contributes to the ongoing liver injury (12). PAF has been suspected to play an important role in liver pathophysiology. The cultured Kupffer and endothelial cells produce and release PAF in order to facilitate communication between hepatic sinusoidal and parenchymal cells (12). Moreover, PAF is an important mediator of hepatic injury. Inappropriate production of PAF leads to pathologic inflammation, and PAF is clearly involved in liver damage as PAF receptor blockers reduce hepatic damage after ischemia reperfusion. (13). Villamediana et al. (14) found that, in the cirrhotic rats, PAF levels were elevated in systemic blood but made no measurements of the hepatic PAF system or altered hepatic responses to PAF. Marathe et al. (15) reported increased hepatic PAF two hours after CCl4 administration but did not determine if the PAF content of liver was elevated during chronic injury. Therefore, a thorough study was needed to estimate the level of hepatic PAF after intoxication for prolonged time. The present study aimed to estimate hepatic PAF levels 3 weeks after CCl4-induced liver damage in rats. Different agents with different postulated mechanisms of action on liver injury were selected; OMNI® (a drug under clinical trials for antiviral therapy), Mirazid® (Schistomicidal agent), Thioproline (a well known antioxidant agent) and Pegasys® (long acting interferon). This study, in addition, aimed to test the influence of these drugs on hepatic PAF levels after CCl4 intoxication and subsequently the possible contribution of this effect to their known hepatoprotective action. OMNI®, a drug under clinical trials for treatment of hepatitis C virus (HCV), is composed of boswellic acids, curcumin and glycyrrhizin. Boswellic acids are the effective compounds isolated from the gum-resin of Boswellia serrata and Boswellia carterii that have been used for the treatment of rheumatoid arthritis and inflammatory bowel diseases (16) and may have cytostatic and apoptotic effects towards a variety of malignant cells (17). Curcumin is a natural compound -2- present in the rhizome of plant Curcuma longa Linn, it has anti-inflammatory, anti-carcinogenic, anti-thrombotic, antispasmodic and potent antioxidant effects (18). Glycyrrhizin, a major component of licorice root, is an anti-inflammatory and antioxidant compound isolated from Glycyrrhiza glabra (19). It has inhibitory effect on PAF production in human neutrophils in a dose dependent manner (20) and it was shown to significantly suppress the production of PAF from the rat peritoneal exudate cells (21). The anti-inflammatory and anti-allergic effects of glycyrrhizin were suggested to be due to the suppression of PAF production (21). Mirazid® is a commercially available drug used as a safe and effective natural product against Schistosoma mansoni infection (22). It is a special formulation of myrrh; the oleo-gum resin obtained from the stems of Commiphora molmol, and probably other species of Bursearacae (23). Myrrh is useful for treatment of sore throat, bleeding gums, chronic pharyngitis and amenorrhea (24) and is used widely in Somalia for treatment of diarrhea and stomach complains (25). Moreover, myrrh is approved by the Food and Drug Adminstation (FDA) for food use (21 CFR 172.510). Thioproline (thiazolidine-4-carboxylic acid, timonacic acid or Hepargen ) is a cyclic sulfur containing amino acid and is a condensation product of cysteine and formaldehyde (26). Animal studies confirmed the anti-toxic effects of Thioproline, particularly on the liver (27). Thioproline has been clinically used, mainly in the treatment of liver diseases and related gastrointestinal disturbances (27). Pegasys® (peg interferon alpha-2a) is a long acting interferon used in antiviral therapy in humans, mainly for viral hepatitis B and C. An anti-fibrotic effect of interferon has been postulated even in the absence of antiviral response, suggesting that, interferon directly inhibits fibrogenesis (28-30). Moreover, its effect on the reduction of fibrosis has been discovered in different experimental rat models of hepatic fibrosis (31-33). ® Materials and Methods A) Chemicals: ALT and AST kits were purchased from bioMerieux Co.; Thioproline powder, chloramine-T and perchloric acid were obtained from Aldrich Co.; pdimethylamino-benzaldehyde and authentic PAF (1-O-palmityl-2-acetyl-snglycero-3-phosphocholine) were purchased from Sigma Chemical Co. B) Animals: Fifty four Wistar rats, weighing 180-250 gm, were used in this study. They were fed with a standard laboratory diet and tap water ad libitum and housed in individual cages. Houses were kept at 255oC, 555% humidity, and a 12 h light/dark cycle. Rats were divided into 6 groups each comprised 9 rats. Based on the treatment protocol and dosage regimen described previously by the author (34), animals were treated as follow: Group 1 was treated only with 40% -3- CCl4 in corn oil ( 0.375 ml/kg), groups 2 to 5 were treated with OMNI®, Mirazid®, Thioproline and Pegasys®, respectively, one week after CCl4 intoxication, whereas the 6th group was the normal control group, which only received an injection of corn oil (0.375 ml/kg). Liver damage was induced in all groups except normal control group (groups 1 to 5) by i.p. injection of CCl4 3 times a week for 3 weeks. One week after CCl4 intoxication, drugs were injected i.p. daily for 3 weeks in the following doses; OMNI® (600 mg/kg), Mirazid® (500 mg/kg), Thioproline (100 mg/kg) and Pegasys® (0.5 μg/rat). C) Assessment of liver fibrosis: i- Estimation of liver enzymes (ALT and AST): At the and of the 3 weeks of study, blood was withdrawn from the eye ball under ether anesthesia. The blood was allowed to coagulate then centrifuged at 3000 rpm for 10 min. to separate the serum. Serum levels of ALT and AST were measured immediately according to the method of Reitman and Frankel (35). ii- Estimation of hepatic hydroxyproline: The content of hepatic hydroxyproline was measured to estimate the anti-fibrotic property of the injected drugs by using the modified method of Woessner (36). Briefly, at room temperature, liver tissues of the right lobe were dehydrated by 95% alcohol for 5-6 hrs, and defatted by acetone for two days. The obtained defatted tissues were dried at 110oC and ground into powder. Forty mg of liver tissue powder were hydrolysed in 3 ml of 6 M HCl at 110o for 6 hrs. The hydrolysates were filtered and diluted to 50 ml with distilled water, and the solution was neutralized to pH 6 by 6 M NaOH. Two ml of the solution and 1 ml of 0.05 M chloramine-T were placed in a glass tube, shaken vigorously and left at room temperature for 20 min., followed by addition of 1 ml 3.15 M perchloric acid and 1 ml of 10% p-dimethylamino-benzaldehyde and incubated at 60oC for 20 min. Finally, the reaction mixture was cooled in an ice bath for 5 min. and the obtained color was measured spectrophotometrically at 550 nm against reagent blank. Standard hydroxyproline solutions of concentrations 5, 10, 15, 20, 25 and 30 g/ml, were used for construction of the standard curve. D) Assessment of oxidative stress: Lipid peroxidation, a major indicator of oxidative stress, was assayed by measuring malondialdehyde (MDA) in serum (37). Serum level of catalase was determined according to the method of Goth (38). E) Determination of PAF in liver tissues: PAF was extracted and purified form liver as described previously (39, 40). PAF was determined using high performance thin layer chromatography (HPTLC) (41) as described below. For lipid extraction, 100 mg of liver were homogenized in 9.5 ml of methanol-chloroform-water mixture (2:1:0.8 v/v). The homogenates were kept at -4- room temperature for one hour, mixed with 5 ml chloroform-water (1:1 v/v), and after one hour the mixture was centrifuged (3000 rpm for 15 min). The lower chloroformic layer containing hepatic lipids, including PAF, was aspirated into glass tubes and stored at -20oC. For purification, the chloroformic layer was dried under nitrogen and the obtained residue was dissolved in 200 l of chloroform and finally purified by Sep-Pak columns (Strata, phenomenex, USA) using 3 ml of acetone-chloroform (2:3 v/v). The eluate was dried under reduced pressure at room temperature and then quantitatively transferred with chloroform into a small vial and evaporated until dryness under nitrogen. For PAF determination, the residue was redissolved in 100 l chloroform and spotted on precoated HPTLC (Merck, Germany) using chloroform-methanol-water (65:53:6 v/v/v) as the developing solvent (41). Spots on a HPTLC were quantitized spectroscopically by transmission at 254 nm. The layer was passed through a beam of light, and the transmitted energy was measured by densitometer (Wilmington, FNC, USA). Authentic PAF (C16); 1-Opalmityl-2-acetyl-sn-glycero-3- phosphocholine (Sigma, GmbH, Germany) was dissolved in chloroform to produce a concentration range of 2.5 to 50 fmoles and assayed by the same method. PAF concentrations on HPTLC fractions of unknown samples were calculated directly from PAF C16 standard curve and expressed pmole equivalent of PAF C16/ mg liver tissue. Total PAF for a given sample represented the sum of PAF activity detected in all HPTLC fractions for that sample. Statistical analysis: Data were expressed as mean standard error of mean (SEM). Statistical analysis was performed using Instat-3 computer program (Graph pad software Inc, San Diego, CA, USA). The groups were compared using one way analysis of variance (ANOVA) followed by Tukey-Kramer multiple comparison test. Results Values of the analyzed parameters and the statistical differences in the groups are shown in Table (1) and Figure (1). During the experiment, one rat died from each of the following groups; CCl4, Mirazid® and Pegasys®, while three rats died from Thioproline group. a) Liver fibrosis markers: Three weeks after CCl4 administration; levels of serum transaminases (ALT, AST) and hepatic hydroxyproline were significantly higher (p<0.001) in group 1 (rats received CCl4 only) than those of control. Groups 2 to 5 (OMNI®, Mirazid®, Thioproline and Pegasys®) showed significant reductions (p<0.001) in serum ALT and hepatic hydroxyproline levels in comparison with CCl 4 group and insignificant differences were observed as compared to control group. On the other hand, serum AST decreased significantly (p<0.01) only in OMNI®-treated -5- group as compared to CCl4 group, whereas, Mirazid®, Thioproline and Pegasys® did not significantly affect AST as compared to CCl4 group. No significant differences were found among drug-treated groups in ALT and hydroxyproline levels. b) Oxidative stress markers: Serum MDA levels were significantly higher (p<0.001) in CCl4 group than in control. OMNI®, Mirazid®, Thioproline and Pegasys® significantly reduced (p<0.001) serum MDA levels as compared to CCl4 with no significant differences in comparison with control. On the other hand, serum catalase levels decreased significantly (p<0.05) in CCl4 group as compared to control. All tested drugs significantly increased catalase levels as compared to CCl4 group (p<0.01). No significant differences were observed in levels of MDA and catalase among tested drug groups. C) Hepatic PAF levels: A highly significant increase in hepatic PAF levels was observed in CCl4 group as compared to control (24.242.01 Vs 8.811.09 pmol equiv./mg, p<0.001). A highly significant reductions (11.84±0.22, 14.5±1.00, 13.17±0.54 and 14.26±1.09 pmol equiv./mg, p<0.001) were detected by OMNI®, Mirazid®, Thioproline and Pegasys®, respectively, as compared to CCl4 group. OMNI® and Thioproline groups showed no significant differences in hepatic PAF as compared to control, while PAF levels in Mirazid® and Pegasys® groups were still significantly higher (p<0.01) than those of control. No significant differences were shown among tested drug groups. As shown in Table (2), positive correlation was found between levels of PAF and MDA in CCl4 and tested drug groups. The correlation was significant in CCl4, OMNI® and Thioproline groups, while insignificant correlation was seen in Mirazid® and Pegasys® groups. On the other hand, negative correlation was observed between levels of PAF and catalase, significantly in CCl4 and OMNI® groups and insignificantly in Mirazid®, Thioproline and Pegasys® groups. Discussion Metabolism of CCl4 by hepatocytes and/or endogenous macrophage like Kupffer cells (42), resulted in severe hepatic necrosis and fibrosis as indicated by elevated liver enzymes (ALT and AST) and hepatic concentration of hydroxyproline. In this established model, liver injury is derived from a mixture of free radicals and reactive oxygen species (43, 44), lipid peroxidation (45, 46) and activated Kupffer cells (47), each of which has an underlying role in resulting liver damage. The administration of OMNI®, Mirazid®, Thioproline and Pegasys® to CCl4-intoxicated rats for 3 weeks limited the metabolism of CCl4 and improved the biochemical parameters. These results were obvious from their effect on lowering -6- liver enzyme (ALT), hepatic hydroxyproline and serum MDA in addition to increasing serum catalase (Table 1). The antioxidant activity of OMNI® is derived mainly from curcumin which is a very potent antioxidant (18, 48-50) and glycyrrhizin which antioxidant activity (51-53) and its role in reducing liver fibrosis (54) has been established. Thioproline (thiazolidine-4-carboxylic acid) is a well known intracellular sulfhydryl antioxidant and free radical scavenger (27, 55). Diet supplementation with this antioxidant slowed the aging process, prolonged life span and stimulated the immune system in old mice (55) and reversed age-related behavioral dysfunction in prematurely-aging mice (56). Many studies suggest an antioxidant and anti-fibrotic activity of interferon alpha (IFN-) (29,32,57-59). Lu et al.(58) suggested that, IFN- may enhance biological defense activities against oxidative stress and function as a potent fibro-suppressant by protecting hepatocytes and hepatic stellate cells from lipid peroxidation. In the study of Serejo et al. (29), IFN- promoted a long term inhibition of oxidative stress with concomitant improvement of activity of fibrosis. Madro et al. (32) found positive effects of high doses of IFN- in improving liver function and reducing liver fibrosis induced by CCl4 in rats. Platelet activating factor (PAF) is a potent pro-inflammatory and hypotensive phospholipid (1-6). Inappropriate or excessive PAF has the potential to modify liver function, and PAF is an established hepatotoxic agent (9, 11). Our study aimed to estimate hepatic levels of PAF in CCl4-induced liver fibrosis in rats. In addition, the effect of different hepatoprotective drugs (OMNI®, Mirazid®, Thioproline and Pegasys®) on these levels was also studied. The results showed a highly significant increase in hepatic PAF levels in CCl4 group as compared to control (Fig. 1). This is in agreement with the results obtained by Yang et al. (60). It has been found that, Kupffer cells isolated from cirrhotic rats release significantly more PAF than those obtained from control rats (61). Hepatic endothelial cells and systemic macrophage recruited to injured liver may also contribute to elevated hepatic PAF levels. Marathe et al. (15) found that, the livers of rats metabolizing CCl4 contain inflammatory phospholipids, mainly PAF. They also found that, oxidants, which stimulate cellular PAF generation in vitro, such as H2O2, (62) lead to the accumulation of significant amounts of hepatic PAF. In addition, CCl4 metabolism by cytochrome P-450 generates the reactive trichloromethyl (CCl3) radical and this event generates superoxide and H2O2 (45). H2O2 stimulates the synthesis of PAF (62,63) and PAF is synthesized by stimulated macrophages and Kupffer cells (61). All these findings coincide with our results in CCl4 group that revealed a strong positive correlation between PAF and MDA as well as a significant negative correlation between PAF and catalase (Table 2). It is also postulated that, the elevated hepatic PAF in this model is related to reduced PAF metabolism by the liver due to low secretion of PAF- -7- actylhydrolase, an enzyme predominantly responsible for hydrolysis of PAF to lysoPAF (64). All tested drugs (OMNI®, Mirazid®, Thioproline and Pegasys®) exerted a significant reduction of hepatic PAF after 3 weeks of treatment (Fig. 1). These results may add further explanation to the anti-fibrotic activity of these drugs. However, the levels of hepatic PAF were still higher than those of control (significantly in Mirazid® and Pegasys® groups and insignificantly in OMNI® and Thioproline groups). This may suggest the need for either higher doses or prolonged time of treatment. The effect of the tested drugs on hepatic PAF could be attributed to their inhibitory effect on PAF production, through their antioxidant activity revealed by lowering MDA levels and increasing catalase (Table 1). This explanation could be confirmed by the positive correlation observed in the tested drug groups between levels of PAF and MDA as well as the negative correlation found between PAF and catalase (Table 2). Higher catalase levels achieved by these drugs leads to H2O2 scavenging limiting its role in PAF production (62,63). Most likely, the drugs in this study may affect the activity of cholinephosphotransferase (CPT) or PAF-acetylhydrolase; the enzymes which are responsible for synthesis and degradation of PAF, respectively. It has been found that, CPT was reduced significantly in renal cell carcinoma patients who had received IFN- compared with those who had not (65). These findings suggest that IFN- may modulate the production of PAF. Further studies are recommended to study the modulatory effect of these drugs on the enzymes that regulate PAF levels. Conclusion Hepatic PAF level showed an increase in CCl4-induced liver fibrosis in rats. The treatment of intoxicated rats with OMNI®, Mirazid®, Thioproline and Pegasys® daily for 3 weeks modulated the toxic effect of CCl4 via either antioxidant activity and/or lowering PAF contents of liver tissues. This study may add further explanation to the anti-fibrotic activity of the tested compounds via reducing hepatic PAF levels. Acknowledgment We thank Mr. Ahmad Abbas; the technician of Pharmacognosy Department, Faculty of Pharmacy, Mansoura University for technical assistance, care of animal house and his effort throughout the whole work. -8- References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Snyder F. Platelet-activating factor and related acetylated lipids as potent biologically active cellular mediators. Am J Physiol 1990; 259:C697–708. Chao W and Olson MS. Platelet-activating factor: receptors and signal transduction. Biochem J 1993; 292:617–629. Snyder F. Platelet-activating factor and its analogs: metabolic pathways and related intracellular processes. Biochem Biophys Acta 1995; 1254:231–249. Prescott SM, Zimmerman GA, Stafforini DM and McIntyre TM. Plateletactivating factor and related lipid mediators. Annu Rev Biochem 2000; 69:419–445. Montrucchio G, Alloatti G and Camussi G. Role of platelet-activating factor in cardiovascular pathophysiology. Physiol Rev 2000; 80:1669– 1699. Zimmerman GA, Prescott SM and McIntyre TM. Endothelial cell interactions with granulocytes: tethering and signaling molecules. Immunol Today 1992; 13:93–100. Braquet P, Paubert-Braquet M, Bourgain RH, Bussolino F and Hosford D. PAF/cytokine autogenerated feedback networks in microvascular immune injury: consequences in shock, ischemia and graft rejection (published erratum appears in J Lipid Mediat 1989; 1:361). J Lipid Mediat 1989; 1:75–112. Lorant DE, Patel KD, McIntyre TM, McEver RP, Prescott SM and Zimmerman GA. Coexpression of GMP-140 and PAF by endothelium stimulated by histamine or thrombin: a juxtacrine system for adhesion and activation of neutrophils. J Cell Biol 1991; 115:223–234. Zhou W, McCollum MO, Levine BA and Olson MS. Inflammation and platelet activating factor production during hepatic ischemia/reperfusion. Hepatol 1992; 16: 1236-1240. Olson MS, Kitten AM, Eakes AT, Howard KM, Miller JE and Mustafa SB. The role of lipid and peptide mediators in hepatic cell communication. In: Shimazu T, ed. Liver Innervation London: John Libbey& Co. Ltd 1996, pp. 75–85. Zhou W, Chao W, Levine BA and Olson MS. Role of platelet activating factor in hepatic responses after bile duct ligation in rats. Am J Physiol 1992; 263:G587–G592. Coker A, Coker I, Huseyinov A, Sokmen S and Karademir, S. Is mannitol effective against platelet activating factor (PAF)-induced liver damage in obstructive jaundice? Hepatogastroenterology 2001; 48(40): 1134-1137. Yamakawa Y, Takano M, Patel M, Tien N, Takada T and Bulkley GB. Interaction of platelet activating factor, reactive oxygen species generated by xanthine oxidase and leukocytes in the generation of hepatic injury after shock/resuscitation. Ann Surg 2000; 231:387-398. Villamediana LM, Sanz E, Fernandez-Gallardo S, Caramelo C, Sanchez Crespo M, Braquet P and Lopez-Novoa JM. Effects of the platelet -9- 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. activating factor antagonist BN 52021 on the hemodynamics of rats with experimental cirrhosis of the liver. Life Sci 1986; 39:201–205. Marathe GK, Harrison KA, Roberts LJ, Morrow JD, Murphy RC, Tjoelker LW, Prescott SM, Zimmerman GA and McIntyre TM. Identification of platelet activating factor as the inflammatory lipid mediator in CCl4-metabolizing rat liver. J Lipid Res 2001; 42:587–596. Syrovets T, Buchele B, Krauss C, Laumonnier Y and Simmet T. Acetylboswellic acids inhibit lipopolysaccharide-mediated TNF-alpha induction in monocytes by direct interaction with I kappa B kinases. J Immunol 2005; 174(1): 498-506. Hostanska K, Daum G and Saller R. Cytostatic and apoptosis-inducing activity of boswellic acids toward malignant cell lines in vitro. Anticancer Res 2002; 22(5): 2853-2862. Kohli K, Ali J, Ansari MJ and Raheman Z. Curcumin: A natural antiinflammatory agent. Indian J Pharmacol 2005; 37: 141-147. Francischetti IM, Monteiro RQ, Guimaraes JA. Francischetti IM, Monteiro RQ and Guimaraes JA. Identification of glycyrrhizin as a thrombin inhibitor. Biochem Biophys Res Commun 1997; 235(1): 259-263. Nakamura T, Kuriyama M, Kosuge E, Ishihara K and Ito K. Effects of saiboku-to (TJ-96) on the production of platelet-activating factor in human neutrophils. Ann N Y Acad Sci 1993; 685:572-579. Ichikawa Y, Mizoguchi Y, Kioka K, Kobayashi K, Tomekawa K, Morosawa S and Yamamoto S. Effect of glycyrrhizin on the production of platelet-activating factor from rat peritoneal exudate cells. Arerugi 1989; 38(4): 365-369. Badria FA, Abou-Mohamed G, El-Mowafy AM, Masoud A and Salama O. Mirazid: A new Schistosomicidal drug. Pharmaceutical Biology 2001; 39(2): 127-131 Greene DA. Gold, frankincense, myrrh and medicine. North Carolina Med J 1993; 54: 620-622. Claeson P, Andersson R and Samuelsson G. T-cadinol: A pharmacologically active constituent of scented myrrh: introductory pharmacological characterization and high field H- and C- NMR data. Planta Med 1991; 57: 352-356. Michie CA and Cooper E. Frankincense and myrrh as remedies in children. J R Soc Med 1991; 84: 602-605. Ratner S and Clarke HT. The action of formaldehyde upon cysteine. J Am Chem Soc 1937; 59:200-206. Weber HU, Fleming JF and Miquel J. Thiazolidine-4-carboxylic acid, a physiologic sulfhydryl antioxidant with potential value in geriatric medicine. Arch Gerontol Geriat 1982; 1 (4): 299-310. Shiratori Y, Imazzeki F, Moriyama M, Yano M, Arakawa Y, Yokosuka O, Kuroki T, Nishiquchi S, Sata M, Yamada G, Fujiyama S, Toshida H and Omata M. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Int Med 2000; 132: 517-524. Serejo F, Emerit I, Filipe PM, Fernandes AC, Costa MA, Freitas JP and de Moura MC. Oxidative stress in chronic hepatitis C: the effect of - 10 - 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. interferon therapy and correlation with pathological features. Cand J Gastroenterol 2003; 17(11):644-655. Guerret S, Desmouliere A, Chossegros P, Costa AM, Badid C, Trepo C, Grimaud JA and Chevallier M. Long term administration of interferon- α in non-responder patients with chronic hepatitis C: follow up of liver fibrosis over 5 years. J Viral Hepatol 1999; 6: 125-133. Souza MM, Parana R, Trepo C, Barbosa AA, Oliveira I and Andrade ZA. Effect of interferon- α on experimental septal fibrosis of the liver-study with a new model. Mem Inst Oswaldo Cruz 2001; 96(3): 343-348. Madro A, Somka M, Celiski K, Chibowski D, Czechowska G, Kleinrok Z and Karpiska A. The influence of interferon alpha on the rat liver injured by chronic administration of carbon tetrachloride. Ann Univ Mariae Curie Sklodowska 2002; 57(1): 55-60. Chang M-C, Chang Y and Jia A. Effects of interferon-alpha on expression of hepatic stellate cell and transforming growth factor-β1 and α-smooth muscle actin in rats with hepatic fibrosis. World J Gastroenterol 2005; 11(17): 2634-2636. Badria FA, Houssen WA, El-Nashar EM and Said SA. Biochemical and histopathological evaluation of glycyrrhizin and Boswellia carterii extract on rat liver injury. Biosci Biotech Res Asia 2003; 1 (2): 93-96. Reitman S and Frankel S. Determination of serum GOT and GPT by a colorimetric method. Am J Clin Path 1957; 28: 56. Woessner, JF. The determination of hydroxyproline in tissue and protein samples containing small proportion of this amino acid. Arch Biochem Biophys 1961; 93: 440-447. Draper, H and Hadley, M. Malondialdehyde determination an index of lipid peroxidation. Methods Enzymol 1990; 186:421-431. Goth, L. A simple method for determination of serum catalase and revision of reference range. Clin Chem Acta 1991; 196:143-152. Bligh EG and Dyer WJ. A rapid method of total lipid extraction and purification. Can J Biochem Physiol 1959; 37: 911-917. Shinozaki K, Kawasaki T, Kambayashi J, Sakon M, Shiba E, Uemura Y, Ou M, Twamoto N and Mori T. A new method of purification and sensitive bioassay of platelet activating factor (PAF) in human whole blood. Life Sci 1994; 54 : 429-437. Wang R, Zhang XJ, Hu XL and Zhao XH. High performance thin layer chromatographic (HPTLC) determination of PAF in cerebrospinal fluid of patients with subarachnoid hemorrhage (SAH). Se Pu 1999; 17(6): 590592. Badger DA, Sauer JM, Hoglen NC, Jolley CS and Sipes IG. The role of inflammatory cells and cytochrome P450 in the potentiation of CCl4induced liver injury by a single dose of retinol. Toxicol Appl Pharmacol 1996; 141: 507-519. el Sisi AE, Earnest DL and Sipes IG. Vitamin A potentiation of carbon tetrachloride hepatotoxicity: role of liver macrophages and active oxygen species. Toxicol Appl Pharmacol 1993; 119: 295-301. - 11 - 44. Sipes IG, el Sisi AE, Sim WW, Mobley SA and Earnest DL. Reactive oxygen species in the progression of CCl4- induced liver injury. Adv Exp Med Biol 1991; 283: 489-497. 45. Terao J, Asano I and Matsushita S. High-performance liquid chromatographic determination of phospholipid peroxidation products of rat liver after carbon tetrachloride administration. Arch Biochem Biophys 1984; 235: 326-333. 46. el Sisi AE, Earnest DL and Sipes IG. Vitamin A potentiation of carbon tetrachloride hepatotoxicity: enhanced lipid peroxidation without enhanced biotransformation. Toxicol Appl Pharmacol 1993; 119: 289-294. 47. Edwards MJ, Keller BJ, Kauffman, FC and Thurman RG. The involvement of Kupffer cells in carbon tetrachloride toxicity. Toxicol Appl Pharmacol 1993; 119: 275-279. 48. Sharma OP. Antioxidant activity of curcumin and related compounds. Biochem Pharmacol 1976; 25: 1811-1815. 49. Osawa T, Sugiyama Y, Inayoshi M and Kawakishi S. Antioxidant activity of tetrahydrocurcuminoids. Biosci Biotechnol Biochem 1995; 59: 16091612. 50. Iqbal M, Sharma SD, Okazaki Y, Fujisawa M and Okada S. Dietary supplementation of curcumin enhances antioxidant and phase II metabolizing enzymes in ddy male mice: Possible role in protection against chemical carcinogenesis and toxicity. Pharmacol Toxicol 2003; 92: 33-38. 51. Hu CC, Chen WK, Liao PH, Yu WC and Lee YJ. Synergistic effect of cadmium chloride and acetaldehyde on cytotoxicity and its prevention by quercetin and glycyrrhizin. Mutat Res 2001; 496(1-2): 117-127. 52. Melhem A, Stern M, Shibolet O, Ackerman Z, Pappo O, Hemed N, Rowe M, Ohano H, Zebrecky G, Cohen R and Ilan Y. Treatment of chronic hepatitis C virus infection via antioxidants: results of a phase I clinical trial. J Clin Gastroenterol 2005; 39 (8): 737-742. 53. Rahman S and Sultana S. Chemopreventive activity of glycyrrhizin on lead acetate mediated hepatic oxidative stress and its hyperproliferative activity in Wistar rats. Chem Biol Interact 2006; 160 (1): 61-69. 54. Ono M, Miyamura M, Kyotani S, Saibara T, Ohnishi S and Nishioka Y. Effects of Sho-saiko-to extract on liver fibrosis in relation to the changes in hydroxyproline and retinoid levels of the liver in rats. J Pharm Pharmacol 1999; 51 (9): 1079-1084. 55. de la Fuente M, Ferrandez D, Munoz F, de Juan E, Miquel J. Stimulation by the antioxidant thioproline of the lymphocyte functions of old mice. Mech Aging Dev 1993; 68 (1-3): 27-36. 56. Guayerbas N, Puerto M, Hernanz A, Miquel J and de la Fuente M. Thiolic antioxidant supplementation of the diet reverses age-related behavioral dysfunction in prematurely ageing mice. Pharmacol Biochem Behav 2005; 80 (1): 45-51. 57. Vendemiale G, Grattagliano I, Caruso ML, Serviddio G, Valentini AM, Pirrelli M and Altomare E. Increased oxidative stress in dimethylnitrosamine-induced liver fibrosis in the rat: effect of N- - 12 - 58. 59. 60. 61. 62. 63. 64. 65. acetylcysteine and interferon-alpha. Toxicol Appl Pharmacol 2001; 175 (2): 130-9. Lu G, Shimizu I, Cui X, Itonaga M, Tamaki K, Fukuno H, Inoue H, Honda H and Ito S. Interferon-alpha enhances biological defense activities against oxidative stress in cultured rat hepatocytes and hepatic stellate cells. J Med Invest 2002; 49(3-4): 172-81. Dikici I, Mehmetoglu I, Dikici N, Bitirgen M and Kurban S. Investigation of oxidative stress and some antioxidants in patients with acute and chronic viral hepatitis B and the effect of interferon-alpha treatment. Clin Biochem 2005; 38 (12): 1141-1144. Yang Y, Nemato EM, Harvey SAK, Subbotin VM and Gandhi CR. Increased hepatic platelet activating factor (PAF) and PAF receptors in carbon tetrachloride induced liver cirrhosis. Gut 2004; 35:877-883. Yang Y, Harvey SAK and Gandhi CR. Kupffer cells are a major source of increased platelet-activating factor in the CCl4-induced cirrhotic liver. J Hepatol 2003; 39: 200–207. Lewis MS, Whatley RE, Cain P, McIntyre TM, Prescott SM and Zimmerman GA. Hydrogen peroxide stimulates the synthesis of platelet activating factor by endothelium and induces endothelial cell-dependent neutrophil adhesion. J Clin Invest 1988; 82:2045-2055. Hughes H, Sands MA, McGuire GM and Taylor AA. PAF formation by H2O2-stimulated perfused canine carotid arteries. Prostaglandins Leukt Essent Fatty Acids 1994; 51:323-328. Blank ML, Hall MN, Cress EA and Snyder F. Inactivation of 1-alkyl-2acetyl-sn-glycero-3-phosphocholine by a plasma acetylhydrolase: higher activities in hypertensive rats. Biochem Biophys Res Commun 1983; 113: 666-671. Imagawa M, Mimata H, Takahashi S, Nakagawa M, Nomura Y and Ogata J. Modulation of platelet activating factor synthesis by recombinant interferon-alpha in human renal cell carcinoma. Urol Int 1996; 57(1): 1116. - 13 - Table (1): Group Marker CCl4 (n=8) OMNI®+CCl4 ALT AST H. proline MDA CAT (IU/ml) (IU/ml) (g/ml) (nmol/ml) (kU/L) a 151.214.3 a b 76.68.2 b b 70.04.2 a 219.69.9 a 22.051.07 a 17.70.84 164.69.6 b 12.90.42 b 205.810.6 b b 10.630.68 a 219 4.27 b 289.7 15.2 b 295.5 (n=9) Mirazid®+ 14.50.7 11.060.7 CCl4 (n=8) Thio+CCl4 11.7 b b (n=6) Pegasys®+CCl4 (n=9) 252.618 b 13.90.52 b 13.350.9 292.6.4 13.5 b b (n=8) Control 71.258.0 b 73.125.6 194.521.7 b 13.40.44 b 11.260.38 302.6 11.7 b b 58.574.7 b 159.36.4 b 12.50.73 b 10.70.26 291.5 10.95 n=number of rats a=significance versus control. b=significance versus CCl4 group. Thio=Thioproline, ALT=alanine aminotransferase, AST=aspartate aminotransferase, MDA=malondialdehyde, CAT= catalase, H. proline=hydroxyproline. - 14 - Table (2): Correlation between Correlation between PAF PAF and MDA and Catalase Significant, p<0.01 Significant, p<0.05 r =0.87 r = -0.81 Significant, p<0.05 Significant, p<0.01 r =0.79 r = -0.76 Not significant Not significant r =0.67 r = -0.50 Thioproline+CCl4 Significant, p<0.05 Not significant (n=6) r =0.82 r = -0.55 Not significant Not significant r =0.52 r = -0.57 CCl4 group (n=8) OMNI®+CCl4 (n=9) Mirazid®+CCl4 (n=8) ® Pegasys +CCl4 (n=8) - 15 - Table (1): Markers of liver fibrosis and oxidative stress in OMNI ®, Mirazid®, Thioproline and Pegasys® groups as compared to both control and CCl4 groups 3 weeks after treatment. Values were expressed as meanSEM. Table (2): Correlation between levels of PAF and levels of both MDA and catalase in CCl4, OMNI®, Mirazid®, Thioproline and Pegasys® groups. - 16 - Figure (1): 30 PAF (pmol equiv./mg) a 20 ab b ab b b 10 0 CCl4 OMNI® Mirazid® Thio Pegasys®Control + CCl4 + CCl4 + CCl4 + CCl4 - 17 - Legends to figures: Figure (1): Hepatic platelet activating factor (PAF) levels in OMNI ®, Mirazid®, Thioproline and Pegasys® groups as compared to both control and CCl4 groups 3 weeks after treatment. Values were expressed as meanSEM. a = Significance versus control group. b = Significance versus CCl4 group. - 18 -