Medicalizing Sadness - Student Pugwash USA
advertisement

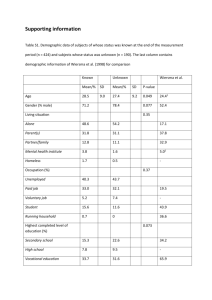
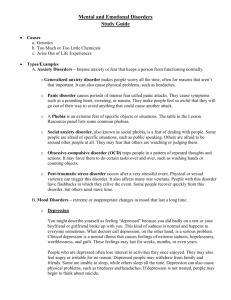
The Age of Depression: How Psychiatry Helped Create An Age of Depressive Disorder According to the New York Times, Sherri Souza is a typical wife of a National Guardsman posted in Iraq. Like most spouses in this situation, she misses her husband, worries about his safety, and is anxious for her family’s future should he be killed or injured. In the past she might have been “sad,” “lonely,” or simply missed her husband’s presence. Now, however, she characterizes herself as “depressed” and is taking medication for her condition. Although we are not given the details of Sherri’s condition, the characterization of her difficulties as “depression,” by which psychiatrists primarily mean major depressive disorder, is becoming more and more typical. Huge proportions of the population seemingly suffer from this disorder. Epidemiological studies indicate that depression afflicts about ten percent of adults in the United States each year and about a quarter of the population at some point in their lives. The number of depressed persons also seems to be steadily growing: For the past several decades, each successive generation reports more depressive disorders than the previous one. These enormous numbers have mobilized psychiatry, general medical practice, and the psychopharmacology industry to mount a coordinated (and profitable) offensive in response, in which better recognition of unreported, hidden, or “sub-clinical” depression plays an important role, thus pushing prevalence numbers ever higher. Not only the number of people labeled as suffering from depression but also the number of persons actually treated for depression has increased exponentially in recent 2 years. The percentage of the population in mental health treatment for depression each year nearly doubled from the early 1980s to the early 2000s. By 1997, fully 40% of all psychotherapy patients were diagnosed with some mood disorder, the category of psychiatric disorder that includes major depression and related conditions. As well, three times more people were treated for depression in primary medical care in 1997 than obtained treatment in these settings only ten years earlier. The consumption of antidepressant medications has also dramatically expanded. At present, 3 of the 7 largest selling prescription drugs (Prozac, Paxil, and Xoloft) of any sort are anti-depressants. Persons treated for depression were four and a half times more likely to have received a psychotropic medication in 1997 than in 1987. Auden’s “Age of Anxiety” appears to have been succeeded by our own “Age of Depressive Disorder.” No plausible theory of depressive disorder, whether genetic, psychological, or social, can explain why rates of depression have increased so much in such a short period of time. Instead, the explanation for the apparent magnitude of this problem appears to lie in vast changes that have occurred in the ways in which physicians, mental health professionals, and people themselves characterize and diagnose their mental states. There are and always have been true depressive disorders, but in the past such disorders in which the response to loss goes awry and takes on a debilitating life of its own were always distinguished from normal sadness that arises in response to life’s vicissitudes. That traditional, commonsense distinction has broken down in contemporary psychiatry, which conflates depressive disorders with normal sadness. The sources and social implications of this breakdown are as yet largely unappreciated. History of Depression 3 How did this transformation of sadness into depression occur? To appreciate what has transpired, the current approach to diagnosis of depression must be placed in the historical context of 2500 years of contrary medical and psychiatric practice. To follow this story to the present, one must also confront the esoterica of modern psychiatric classification as represented by successive editions of the American Psychiatric Association’s much-discussed Diagnostic and Statistical Manual of Mental Disorder (DSM-I through DSM-IV). Often called the “Bible of Psychiatry,” the DSM provides official diagnostic definitions for all mental disorders. As long as written records have been kept, Western cultures have recognized that depression can be a mental disorder. Hippocrates, writing in the 5th century B.C., provided the first known definition of melancholia as a distinct disease: “If fear or distress last for a long time it is melancholia.” While theories of depressive disorder have changed, the symptoms that indicate the disorder have not; for Hippocrates, its symptoms could include prolonged despondency, blue moods, detachment, nameless fears, irritability, restlessness, fear, sleeplessness, aversion to food, and suicidal impulses, much like today’s criteria. But Hippocrates’s definition indicates that not symptoms alone but only symptoms of unexpected duration indicate the presence of a disease condition. A century later, Aristotle elaborated the distinction between normal and pathological mood states. He separated melancholic states that arose from the conditions of everyday life from disorders that involved enduring “groundless” despondency and thus stemmed from internal factors: “We are often in the condition of feeling grief without being able to ascribe any cause to it; such feelings occur to a slight degree in 4 everyone, but those who are thoroughly possessed by them acquire them as a permanent part of their nature.” As in Aristotle’s passage, the key distinction in ancient definitions of melancholia was between states of sadness without cause and those that had similar symptoms arising from actual losses; only the former were mental disorders. “Without cause” does not mean uncaused, for throughout history depression has been attributed to postulated physical or psychological causes such as excessive black bile, disturbances in the circulation of blood, or depletion of energy. Rather, “without cause” means that the symptoms of depression were not associated with the sorts of environmental events that would appropriately lead to sadness such as bereavement, rejection in love, economic failure and the like. Conversely, ancient Greek and Roman physicians would not consider symptoms of depression that occur “with cause” as signs of a mental disorder. Such normal reactions express, in Aretaeus’s words, “mere anger and grief, and sad dejection of mind.” This classic distinction was based not on symptoms, which could be identical in the two states, but on the relation of the symptoms to the context in which they appeared. Symptoms that arose in contexts that could expectably produce them and that abated in a reasonable period of time after the triggering events ended indicated normal functioning. Comparable symptoms potentially indicated disorder if they arose without appropriate triggering events or had greater duration or intensity than was appropriate to the triggering events, and thus must be primarily explained by internal factors. The same distinction can be found in Robert Burton’s classic work, The Anatomy of Melancholy, published in 1621. Burton defined the disorder of melancholy as “a kind of dotage without a fever, having for his ordinary companions fear and sadness, without 5 any apparent occasion.” Burton considered such disordered melancholic states “without cause” to be “contrary to nature.” In contrast, he considered the propensity to selflimiting melancholic feelings in response to loss and disappointment to be a normal part of human nature. He describes that transitory melancholy which goes and comes upon every small occasion of sorrow, need, sickness, trouble, fear, grief, passion, or perturbation of the mind, any manner of care, discontent, or thought, which causeth anguish, dullness, heaviness, and vexation of spirit …And from these melancholy dispositions, no man living is free, no Stoic, none so wise, none so happy, none so patient, so generous, so godly, so divine, that can vindicate himself; so well composed, but more or less, some time or other, he feels the smart of it. Melancholy, in this sense is the character of mortality. During the 20th century, psychoanalytic discussions of depression echoed the traditional distinction between abnormal depressions “without cause” and normal depressions “with cause,” calling the former “melancholy” and the latter “mourning.” In Freud’s central article on depression, Mourning and Melancholia, he took for granted that symptoms associated with mourning, although intense, were a normal and self-healing aspect of the human condition that did not require medical treatment, explaining that: … although grief involves grave departures from the normal attitude to life, it never occurs to us to regard it as a morbid condition and hand the mourner over to 6 medical treatment. We rest assured that after a lapse of time it will be overcome, and we look upon any interference with it as inadvisable or even harmful. Freud added an epicycle to the tradition. He observed that, although the symptoms of mourning and melancholia similarly include profound dejection, loss of interest in the outside world, an inability to feel pleasure, and an inhibition of activity, melancholia also frequently includes an extreme and inexplicable (“without cause”) decline in self-esteem beyond the normal self-recriminations after a loss. American psychiatry developed successive versions of its own classification system starting early in the 20th century. Until quite recently, psychiatric definitions of depressive disorder continued to reflect the historical distinction between depression “with” and “without” cause. The first standardized classification system in the United States, the 1918 Statistical Manual for the Use of Hospitals for Mental Diseases, defines “reactive depression” as follows: Here are to be classified those cases which show depression in reaction to obvious external causes which might naturally produce sadness, such as bereavement, sickness and financial and other worries. The reaction, of a more marked degree and of longer duration than normal sadness, may be looked upon as pathological. This definition, not so different in intention from Hippocrates’s, recognizes that sadness that arises naturally and proportionally from external circumstances is normal, whereas disproportionate reactions that are of “more marked degree and of longer duration than 7 normal sadness” suggest disorder. A broad range of negative circumstances are considered to trigger normal sadness, including “bereavement, sickness and financial and other worries.” We shall shortly see that more recent definitions abandon this bit of common sense. The DSM-I (1952) and DSM-II (1968) that succeeded the Statistical Manual emphasized psychoanalytic concepts. The DSM-II defined “depressive neurosis” as follows: “This disorder is manifested by an excessive reaction of depression due to an internal conflict or to an identifiable event such as the loss of a love object or cherished possession.” In insisting that neurotic depressive disorders included only “excessive” reactions, the DSM-II implicitly recognized that disordered reactions are disproportionate to loss. Such reactions were “without cause” either in having only internal causes (assumed to consist of internal conflict) or in being “excessive,” thus unexplainable by external events. Again, normal triggers beyond loss of a loved one were recognized, such as loss of a cherished possession. In sum, 2500 years of psychiatry has held with common sense that human nature includes a normal propensity to potentially intense sadness after certain kinds of losses. Disorder can be judged to exist, it has been widely agreed, only when explanations in terms of triggering events fail to establish a normal cause for the intensity or duration of symptoms. DSM-III and the Revolution in Psychiatric Diagnosis The tradition of systematically distinguishing intense normal sadness from depressive disorder was largely abandoned in the DSM-III (1980). This neglect has 8 continued through various revisions to the current DSM-IV (1994). This shift occurred as part of a broader revolutionary transformation of psychiatric classification guided by Robert Spitzer, the DSM-III’s Editor-in-Chief and Head of the DSM-III Task Force. The great weakness of the DSM-I and II was that their vague, brief, and very general definitions for each of the mental disorders were not capable of generating standardized and reliable methods of classifying and studying mental disorders. In addition, the psychoanalytic dominance of psychiatry was waning, and there was a sharp reaction against the psychoanalytic assumptions of the DSM-II. Psychiatric practice and research had split into rival theoretical fiefdoms ranging from behavioral and cognitive theories to the increasingly influential biological approach, each of which had its own idiosyncratic theory-based definitions of mental disorders. This made communication among practitioners difficult. It meant that research within different paradigms was based on incommensurable definitions, was not cumulative, and could not be usefully compared. It also put many mental health practitioners and researchers in the uncomfortable position of being unable to accept psychiatry’s standard definitions of disorders because of the theoretical assumptions built into them. On top of all of this, psychiatric diagnosis was under attack from a variety of sources. Behaviorists claimed that all behavior was the result of normal learning processes and thus that no mental disorders in the medical sense really existed. The “antipsychiatry” movement, inspired by writers such as psychiatrist Thomas Szasz and sociologist Thomas Scheff, portrayed psychiatric diagnosis as a matter of labeling socially undesirable behavior with medical terminology as an excuse to bring psychiatric interventive power to bear on behavior that was not truly medically disordered. 9 At the crux of many of these objections was the fact that psychiatric diagnosis itself was notoriously unreliable. DSM-II’s vague definitions forced psychiatrists to use considerable clinical judgment in fitting a patient to a diagnosis. This led to unreliability in the application of diagnostic labels: given the same information about the same patient, different mental health professionals were likely to arrive at different diagnoses. Between its theoretical fragmentation and its diagnostic unreliability, psychiatry’s claim to scientific status and even its legitimacy as a medical field seemed in jeopardy. The DSM-III inaugurated basic changes in psychiatric diagnosis to address these challenges. Explicit diagnostic criteria based on lists of observable symptoms were provided as definitions for each of the disorders, allowing improved reliability. Symptom lists provided criteria on which virtually all clinicians of opposed theoretical schools could agree. References to postulated psychodynamic causes of a disorder (e.g., internal conflict, defense against anxiety) were consequently purged. The DSM-III’s diagnostic criteria were theory neutral in the sense that they did not presuppose any particular theory, psychoanalytic or otherwise, of the cause of psychopathology; the criteria were descriptive rather than etiological. Competing theories could henceforth try to prove their claims without begging the question by defining disorders in their own terms, and research became cumulative and comparable across theories. The psychoanalytic dominance of psychiatric diagnosis, unwarranted by the state of the evidence, was effectively ended, and rival approaches were allowed to compete on a flat conceptual playing field. However, a major negative side effect of symptom-based criteria was that they eliminated the consideration of the context in which symptoms arose. One reason for the 10 abandonment of context was the quest for reliability. Studies had shown that most depressions occur after some triggering event. Thus, requiring that reactions be disproportionate to context would mean that clinicians would be frequently making judgments of proportionality, substantially reducing reliability. The problem that increased reliability is of no value if it comes at the cost of validity was ignored. A second reason for leaving out context is that the DSM-III was supposed to be theory neutral, which was interpreted to mean that it had to be neutral as to how the disorder was caused. Moreover, there was an impression that psychotropic medication for depression worked on all people reacting to losses, so that the “with versus without cause” distinction was considered irrelevant to treatment decisions. The problem here is that the normality-versus-disorder distinction has prognostic implications and can be an important consideration in treatment decisions. Finally, there was a fear of misdiagnosing the truly disordered as normal, given that depressed patients are subject to suicide risk. Granting some validity to these reasons, there does not seem to have been an organized attempt to balance potential harms from underdiagnosis and overdiagnosis, as is done with many medical tests. The problem remained that, as the previous 2500 years of psychiatric diagnostic practice had attested, without an exploration of context and meaning, one simply cannot tell whether someone is likely suffering from intense normal sadness or a depressive disorder. From Sadness to Depression: The DSM’s Definition of Depressive Disorder This brings us to how, in the case of depression, the DSM-III criteria went conceptually awry. (For brevity, we focus on Major Depressive Disorder and ignore 11 related diagnoses.) The DSM-III replaced DSM-II’s vague criteria with specific symptomatic criteria. These criteria have remained more or less the same through to the current DSM-IV (1994). Nearly all current studies of depressive disorder are based on the DSM-IV’s definition. Different audiences use this definition for different purposes: clinicians for diagnosing persons who have sought their help; epidemiologists for determining the number of people in the general population who are depressed; researchers for finding the causes of why people are depressed and for evaluating the effectiveness of treatments; economists for estimating the costs associated with depression; pharmaceutical companies for marketing their products; reimbursers for establishing medical necessity and determining quality-of-care standards; and mental health advocates for claiming how widespread this condition is. The DSM definition is used not only in the United States but also has come to be the standard definition used worldwide. The logic of the DSM’s definition of depressive disorder is key to understanding depression as a social fact. The definition requires that five symptoms out of the following nine (the five must include either depressed mood or loss of interest/pleasure) must be present during a two-week period: (1) depressed mood; (2) diminished interest or pleasure in activities; (3) weight gain or loss or change in appetite; (4) insomnia or hypersomnia (excessive sleep); (5) psychomotor agitation or retardation (slowing down); (6) fatigue or loss of energy; (7) feelings of worthlessness or excessive or inappropriate guilt; (8) diminished ability to think or concentrate or indecisiveness; (9) recurrent thoughts of death or suicidal ideation or suicide attempt. In addition, to eliminate rare cases where symptoms are so mild as to 12 be insignificant, symptoms must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. Anyone satisfying these criteria is considered to have a depressive disorder, with three exceptions to be considered shortly. Yet, symptoms such as depressed mood, loss of interest in usual activities, insomnia, lessened appetite, inability to concentrate (because one is grappling with a loss), and so on might naturally occur for two weeks if a major loss, humiliation, or threat to one’s meaning system is experienced, such as being left by a spouse or romantic partner, diagnosis of a serious illness in oneself or a loved one, losing one’s job or pension, failing a major test that has serious implications for one’s career, and so on. Such reactions, even when quite intense due to the severity of the loss, are surely part of normal human nature. Two exceptions to the DSM depression criteria simply shift the diagnosis to other categories of mood disorder - bipolar (manic-depressive) illness or depression caused by a medication or a general medical condition. The third exception is the only acknowledgment of the existence of normal sadness. It exempts from diagnosis cases of normal bereavement after the death of a loved one: “The symptoms are not better accounted for by Bereavement, i.e., after the loss of a loved one, the symptoms persist for longer than 2 months or are characterized by marked functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychotic symptoms, or psychomotor retardation.” The bereavement exclusion thus allows that intense grief reactions are not truly depressive disorders, unless the reaction lasts more than 2 months or it includes one out of a list of five especially serious symptoms. 13 There are two notable aspects of the bereavement exclusion. The first is its limited range of normal grief reactions. For example, an intense grief reaction lasting more than 2 months need not be a disorder. And, the five specified symptoms might indicate disorder, but not necessarily: a normally bereaved individual may experience "marked functional impairment" (e.g., does not feel up to usual work or social activities); may feel that the lost person was his or her "better half" and that he or she is worthless or hopelessly inadequate to life's tasks without the lost partner; may entertain the notion that he or she might be better off "joining" the deceased partner; and so on, without necessarily indicating disorder. But by far the most important thing about the bereavement exclusion is that it offers exclusions only for reactions to the death of a loved one. Yet, such normal sadness reactions that are symptomatically similar to depressive disorders are not limited to bereavement. They encompass reactions to a wide range of severe losses and other negative events such as unwanted marital dissolutions, betrayals by romantic partners, losses of valued jobs, failures to achieve long-anticipated goals, or discoveries of life threatening illnesses in oneself or a loved one. Of course, to be normal responses that satisfy DSM criteria, these conditions must involve a serious loss, and coping mechanisms must allow the individual to adapt to the new circumstances and get over the symptoms within a reasonable time after the stressor ends. If such a trajectory of adaptation to the circumstances does not occur, then one might infer that the original reaction had somehow caused a psychological problem that is now maintained by some internal dysfunction and is no longer a normal reaction. But there are many reactions to loss that, just like normal bereavement responses, might satisfy DSM symptom criteria 14 but are not disorders. The basic flaw, then, is that the DSM fails to exclude from the disorder category sadness reactions to any stressors other than death of a loved one that are intense enough to meet the DSM’s criteria but are still normal reactions. The Age of Depression in which we find ourselves is partly an artifact of a logical error. Creating Major Depression in the Community A vast extension of the application of the symptom-based concept of mental disorder occurred when DSM criteria became the basis for large epidemiological studies attempting to measure the extent of mental disorder among people in the community who are not in mental health treatment. Because DSM diagnoses were based entirely upon symptoms, epidemiologists could easily construct lists of questions about symptoms that could be used to determine whether a respondent met DSM criteria for disorder, including depressive disorders. Lay interviewers could administer such questionnaires, allowing researchers to obtain psychiatric diagnoses comparable to those a psychiatric would obtain without the prohibitive expense of psychiatric interviewers. The results would presumably provide good estimates of how much untreated mental disorder existed. These estimates were intended to guide policy makers in allocating resources in light of how much unmet need existed for psychiatric services. The decision to use objective measures of symptoms in community studies largely stems from considerations of practicality and cost and an uncritical acceptance of the DSM’s symptom-based criteria, not from independent tests showing these methods are accurate in identifying disorder in the community. 15 Findings from two major national studies, the Epidemiological Catchment Area Study (ECA) and the National Co-Morbidity Study (NCS) are the basis for the estimates regarding the prevalence of mental disorder that are now widely cited in the scientific, policy, and popular literatures. The NCS estimates that about 5 % of subjects had a current (30-day) episode of major depression, about 10 % had this diagnosis in the past year, about 17% had an episode over their lifetime, and about 24% reported enough symptoms for a lifetime diagnosis of either major depression or a related disorder, dysthymia. Are the many cases of putative Major Depression uncovered in community studies equivalent to treated clinical cases? The odds are against it. These studies follow the DSM in ignoring the context of symptoms. It seems obvious that when all symptoms are counted as potentially disordered, ordinary sadness is hopelessly confounded with genuine disorder. For example, in the ECA study the most common symptoms among those reporting symptoms are “trouble falling asleep, staying asleep, or waking up early” (33.7%), being “tired out all the time” (22.8%), and “thought a lot about death” (22.6%). College students during exam periods (particularly those studying existential philosophy), people who must work overtime, or those worrying about an important upcoming event could all naturally experience these symptoms. Symptoms that neither respondents nor clinicians would consider reasons for entering treatment can indicate disorder in community surveys. Moreover, the duration criteria only require that the symptom last for a two-week period, insuring that many transient and self-correcting symptoms are counted as disordered. 16 The sorts of experiences that produce normal sadness responses – breakups of romantic relationships and marriages, job losses, disappointed career goals and the like – are common in community populations. A survey respondent might recall symptoms such as depressed mood, insomnia, loss of appetite, or diminished pleasure in usual activities that lasted for longer than two weeks after such events. Some of these normal experiences lead to symptoms severe enough to qualify for a diagnosis of major depressive disorder and thus contribute to the seemingly high rate of depression in community populations. Although these symptoms might have dissipated as soon as a new relationship developed, another job was found, or the goal was finally achieved, this individual would join the 20 million people who are claimed to suffer from the presumed disorder of depression each year. Community studies did not so much uncover high rates of depressive disorders as they demonstrated that the natural results of stressful social experiences could meet DSM’s symptom criteria for depression. Promoting estimates of presumed vast numbers of people who suffer from untreated depression and who therefore have an unmet need for mental health treatment might have the opposite effect from what its advocates intend. The medicalizing of sadness can seem to provide a mandate to deal medically with all human misery. A problem of such magnitude would require enormous resources to resolve and can undermine arguments for the parity of treatment for mental and physical health conditions. Ironically, these overwhelmingly high rates have backfired by encouraging skepticism and dismissal by policy makers. 17 The Constituencies for Depression Many factors, some legitimate and some less defensible, drove psychiatry and epidemiology to use symptom-based, context-free criteria for disorder. In the case of depression, in which the symptoms of normal emotional reactions can closely resemble the symptoms of disorder and can best be distinguished by reference to context, this approach is disastrous for achieving the basic psychiatric goal of validly distinguishing disorder from non-disorder. Once this conceptually flawed diagnostic system was securely in place, various constituencies began to take advantage of it as they found that served their respective agendas. The medicalization of sadness thus had a social impact far beyond the narrow domain of psychiatric diagnosis. The National Institute of Mental Health (NIMH) is the major sponsor of research about mental illness. Conflating mental disorders and ordinary sadness and calling both mental illnesses allowed the NIMH to expand its mandate, make claims that mental illness is rampant in the population, and protect and expand its budget. The creation of ubiquitous depressive disease states also depoliticized the NIMH’s previous concern with the problematic psychological consequences of social problems such as poverty, racism, and discrimination. Political support is far more likely to accrue to an agency that is devoted to preventing and curing a widespread disease than to one that confronts controversial social problems. The psychological consequences of chronic states of social deprivation and injustice as well as of stressful life situations are now viewed as diseases that fall within the mandate of mental health professionals when in fact they may be normal human reactions to problematic environments. 18 This transformation has some benefits. American society is sometimes more willing to be compassionate about disorder than about deprivation. Nor is it necessarily a bad thing when economically deprived people receive mental health treatment. In addition, NIMH personnel and the researchers they sponsor are not cynical manipulators of the public but truly believe that the conditions they study are mental disorders. However, changing public discourse to view sadness as depression has the costs of stigmatizing poor people as mentally ill, replacing social policies with the medical treatment of individuals, and creating a one dimensional public discourse that can undermine moral and political distinctions. Mental health researchers are another group that has much to lose if measures of depression should be changed. The DSM’s criteria are used in virtually all of the thousands of studies done in recent years on depression. Many researchers’ careers are built around the study of major depressive disorder. Any major change in diagnostic criteria would throw into doubt the value of past research based on current criteria. Moreover, reducing prevalence estimates by adequately distinguishing normal sadness from depressive disorder could possibly lessen opportunities for funding. No doubt, these practical considerations clash with other, higher values; the understanding of the etiology and best treatment of depressive disorder depends on their using a valid definition of disorder as the basis for sample selection. For mental health clinicians, symptom-based measures of depression not only expand markets but also help obtain reimbursement from third party insurers that will pay to treat diseases but not problems of living. What is now happening is a strange case of two “wrongs” seemingly making a “right.” The DSM provides flawed criteria that do not 19 adequately distinguish disorder from non-disorder. Individual clinicians are faced every day with patients who are suffering from conditions that appear to be intense normal sadness, but that satisfy the DSM’s criteria for disorder. Many sophisticated privatepractice clinicians will readily admit that a sizable proportion of their “depression” caseload consists of individuals who are psychiatrically normal but experiencing stressful life events. To obtain reimbursement for the treatment of such patients, the clinician must classify the individual within a DSM category of disorder, and depression is one of the more common and one of the easier ones to justify given the ubiquity of its symptoms. So, the DSM criteria are invalid, and the clinician goes along, perhaps knowingly, classifying a normal individual as disordered. But who is the clinician to question the fact that the diagnosis is officially sanctioned by the DSM? The patient—and, not incidentally, the clinician—financially benefits from the official diagnosis, and the patient may get useful treatment. This elaborate system of conceptually fraudulent reimbursement is of course easily dismissed as unethical and corrupt. However, it is an unethical act easily rationalized on overriding ethical grounds; the alternative seems inhumane control over treatment decisions by reimbursers on excessively narrow grounds, and refusing requested intervention for people who are suffering. In other areas of medicine, treatment of the normal is debated openly (e.g., should growth hormones be given to normal but short children? Should post-menopausal women be reimbursed for fertility treatment? When does the use of Viagra represent a medical necessity?). In psychiatry, faulty criteria help avoid the issue. 20 One cost of this avoidance is that some policy analysts effectively use the expansiveness of the DSM criteria to argue against reimbursement parity for mental health care. When the issue of parity arises, the first objection sure to be heard is that such parity would break the health-care bank because it would allow every instance of normal unhappiness to qualify for treatment. Such objections are buttressed by the ridicule frequently heaped on DSM criteria in the popular media. A more honest discussion of the normal versus abnormal and their appropriate rights to reimbursement might help to address some of these objections. Family advocacy organizations, which became an influential political movement during the 1980’s, are another group that promotes the idea that mental illnesses such as depression are widespread in the population. The notion that mental disorder is a biologically based medical disorder is essential to the arguments put forward by these groups for reimbursement parity, a major political goal. They also believe that demonstrating the ubiquity of mental illnesses such as depression in the community will aid efforts to destigmatize this condition and obtain more resources for its treatment. Revising DSM criteria to distinguish true disorders from normal sadness reactions thus appears to go against these groups’ agendas. In reality, their case might be strengthened if such a distinction was carefully made and the conceptual flaws in current criteria eliminated. The truly disordered, which includes loved ones of many members of these advocacy groups, would then presumably become more the focus of treatment and resource allocation. Pharmaceutical companies are perhaps the most visible exploiters of symptombased diagnoses. Although there is little evidence that these companies influenced the 21 development of the DSM-III, they capitalized on its symptom-based approach, which created a broader market of disorder for their products to treat. In addition, they are now major sponsors of the activities and research of psychiatrists and advocacy groups. While some concern has arisen about problems with side effects, suicide risk, and dependency, in general, the transformation of sadness into depression has been enormously profitable for these companies. Ubiquitous drug ads now promote widespread symptoms of sadness, anxiety, sleep problems and the like as signs of mental disorders. Like clinicians, the drug companies can legitimately explain that they are only using the criteria officially sanctioned by the psychiatric profession, even as they further inadvertently confuse the public about the boundary between normality and disorder. Perhaps the most successful efforts of pharmaceutical companies has been to increase the diagnosis of depressive disorder and consequent use of medication in general medical practice. The inadequate supply of psychiatrists and other trained mental health practitioners to deal with the enormous numbers of presumably depressed people that epidemiological studies uncover has served as the rationale for an urgent push to have non-mental health personnel diagnose and treat mental disorder, especially depression. Pharmaceutical companies have supported the development of symptom scales for busy physicians to use, which involve brief and easy to use checklists of context-free symptoms based on DSM criteria. These lists can be quickly and routinely administered to patients whatever the reason for their visit to the doctor. Of course, a physician’s patients, even those who are psychiatrically normal, may have much about which to be concerned, sad, or worried. The screening instruments physicians use to detect depression intentionally ignore all such contextual considerations. The result is both unsurprising 22 and shocking; in some studies, levels of mood disorders in general medical practices approach 25%. Because physicians are not trained in psychotherapeutic intervention, medication is the likely treatment. Whether medicating normally sad individuals that meet DSM criteria is helpful, harmful, or neither is a topic that has received virtually no study. The reason is simple; the DSM criteria do not allow the distinction to be made. However, research by the psychologist James Coyne indicates that medical interventions designed to prevent depression have little effect and can sometimes even worsen depression by disrupting normal coping processes and heightening patient focus on negative experiences. Whatever the answer, surely we ought to be studying this question. That would require making important distinctions between normal and disordered sadness responses. And that would in turn require honestly confronting the conceptual morass that now constitutes the diagnosis of depressive disorder. Conclusion For thousands of years, symptoms of sadness that were “with cause” were separated from those that were “without cause.” Only the latter were viewed as mental disorders. The framers of the DSM-III did not explicitly try to expand the domain of disorder and in some ways its definition of depression is more stringent than in previous manuals. The DSM-III’s decontextualized symptom-based criteria for depressive disorder had the unintended consequence, however, of greatly expanding the domain of pathological depression when applied to untreated community samples. Without 23 consideration of context, normal sadness responses of sufficient intensity became pathological. Prevalence rates of depressive disorders have correspondingly skyrocketed. Moreover, the medicalization of sadness in psychiatric diagnoses may create medicalization by laypeople as well. When the public is constantly exposed to pharmaceutical advertisements, public service messages, and news stories about depression that encompass normal sadness, and assured that no stigma attaches to such diagnoses, they naturally tend to monitor themselves for such symptoms, reframe their own experiences of sadness as signs of a mental disorder, and seek professional help for their problems. The result has been skyrocketing rates of treatment for depression that give the mistaken impression that actual rates of depression have increased. Depression can be a serious and sometimes life-threatening condition and depressive disorders must be taken seriously. In addition, in most cases, there is no good reason why people who wish to shouldn't take anti-depressant medication to treat normal sadness, if it proves safe to do so. Freud was surely incorrect, at least in relation to contemporary medical practices, to assert that “it never occurs to us” to medically treat such painful normal conditions. Whether or not public policy ought to blanketly encourage such treatment is another question. While offering skilled help to those who are suffering and can benefit from such help, whether disordered or non-disordered, is a moral imperative, it is not clear that relabeling normal forms of misery as depressive disorder is beneficial or wise public policy. To the extent that sadness results from ordinary human misery, changing or accepting the situations that led to the sadness might be as or more effective than medication or psychotherapy. As well, most sadness naturally diminishes with the passage of time even in the absence of therapeutic 24 interventions. Encouraging general physicians and mental health professionals to diagnose and treat mild depression can thus be an inefficient use of their time. The dangers of overintervention need to be balanced against those of undertreatment, and one element of such balance is a conceptually valid approach to the distinction between disorder and non-disorder. While the medicalization of sadness undoubtedly has a number of beneficial aspects, it also has many costs that should not be uncritically accepted.