have
advertisement

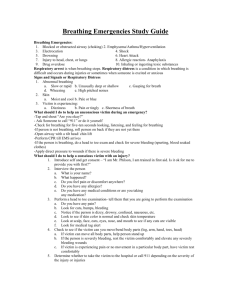
Chapter 3 – CPR-PR Taking Action and Caring for Breathing Emergencies Epinephrine Administration 2 million people in the US are at risk for anaphylaxis and each year 400 to 800 people die Symptoms: Swelling of the face, neck, hands, throat, tongue, or other body part Itching of tongue, armpits, groin or any body part Dizziness Redness or welts on the skin Red watery eyes Nausea, abdominal pain or vomiting Rapid heart rate Difficulty breathing or swallowing Feeling of construction in the throat or chest Epinephrine is a medication prescribed to treat the signs and symptoms of these reactions. Call EMS if anyone has ANY of the above symptoms Use an epinephrine auto-injector when a victim: Relates a history of allergies or allergic reactions Is having an allergic reaction Requests assistance to administer epinephrine Provides the epinephrine or auto-injector Has a family member who relates a victim’s history of allergies or allergic reactions and provides the victim’s auto-injector. Before assisting or administering epinephrine: Summon more advanced medical personnel Check the label to ensure that the prescription is for the victim See if they have already taken a dose – if so, do NOT give another unless instructed by medical personnel Ensure that the prescription has not expired Ensure that the medication is clear and NOT cloudy or discolored Read and follow instructions provided To administer: 1. locate the middle of outer thigh or upper arm to use as injection sight 2. grasp the auto-injector firmly and remove the safety cap 3. hold the auto-injector at a 90 degree angle 4. firmly jab the tip into the thigh. You will hear a click – hold in place 10 seconds. 5. Remove from the thigh and massage the injection site for several minutes Breathing emergencies should be detected during the initial assessment. It occurs when someone's breathing is so impaired that life is threatened. Occur in two ways: breathing is difficult (respiratory distress) breathing has stopped (respiratory arrest) When breathing stops: 0 minutes: Breathing stops. Heart will soon stop beating. 4-6 minutes: Brain damage possible. 6-10 minutes: Brain damage likely Over 10 minutes: Irreversible brain damage certain Breathing emergencies can be caused by: - Obstructed airway (choking) - Illness (ex-pneumonia) - Certain respiratory conditions (asthma, emphysema) - Electrocution - Shock - Drowning More causes of breathing emergencies: - Heart attack or heart disease - Injury to the chest or lungs - Drugs - Poisoning, such as inhaling or ingesting toxic substances - Allergic reactions to food, insect stings, or other allergens - Hyperventilation SIGNALS OF RESPIRATORY DISTRESS Abnormal breathing: breathing is slow or rapid (slow respirations are less than 8 per minute for adults and less than 10 per minute for children/infants breaths are unusually deep or shallow gasping for breath wheezing, gurgling or making high pitched noises Abnormal skin appearance: at first, skin is unusually moist skin & appear flushed later skin may be pale, ashen, or bluish appearance when victim’s skin, or nail beds appear blue = cyanosis Victim feels: - short of breath - dizzy or light headed - pain in chest or tingling in hands and feet - apprehensive or fearful Common conditions causing respiratory distress: 1) Asthma Facts – narrows air passages Triggered by – Allergic reaction to pollen/food/a drug/ insect stings Emotional stress/physical activity Signs & symptoms – Struggle to breathe Wheezing when exhaling 2) Emphysema Facts – lungs lose ability to exchange carbon dioxide and oxygen effectively. Caused by – smoking; usually develops over many years. Signs & symptoms – Shortness of breath Possible coughing, cyanosis, or high fever Advanced cases: restlessness, confusion, weakness 3) Hyperventilation Facts – Rapid breathing upsets body’s balance of oxygen and carbon dioxide Triggered by - Fear/anxiety - Injury to head/severe bleeding/illness - Asthma - Exercise Signs & symptoms – Shallow, rapid breathing Dizziness Numbness in fingers/toes 4) Anaphylaxis (Severe Allergic Reaction) Facts – Swelling of air passages restricts breathing. Triggered by – Food/insect stings/a drug Signs & Symptoms - Skin Rash Tightness in chest/throat Swelling of face/neck/tongue Care for Respiratory Distress: - Summon advanced medical personnel - Have the victim rest in comfortable position. - Keep victim from getting chilled or overheated. - Reduce heat; add moisture. - If authorized, help victim take any medications. - Summon more advanced medical personnel. - Monitor vital signs. Key Points of Respiratory Arrest: - Life threatening - Commonly caused by illness, injury, or choking - Often preceded by respiratory distress - Body systems will progressively fail RESCUE BREATHING Given to victims who are not breathing but still have signs of circulation Works because you inhale 21% oxygen and exhale 16% oxygen Make sure you follow BSI (body substance isolation) precautions Steps for Adults: 1Airway - tilt head & check breathing (use head-tilt/chin-lift) 2Check breathing 3-5 sec. 3Give 2 slow breaths that last 1 second for adults (use a breathing barrier) 4Check for signs of circulation no more than 10 sec. and look for severe bleeding 5Summon advanced help if you have not already done so 6Begin rescue breathing Give 1 breath every 5 sec. for adults Breaths should last approximately 1 second 7Do this for two minutes, remove the mask and recheck for signs of circulation and breathing for no more than 10 seconds. Do Not Stop Rescue Breathing Unless: Victim begins to breathe on his/her own Victim has no signs of circulation (begin CPR) Another trained person takes over EMS personnel arrive on the scene & take over You are too exhausted to continue The scene becomes unsafe 123456- Special Considerations 1. 2. 3. 4. 5. 6. Air in stomach Gastric distension Vomiting Mouth-to-nose breathing Mouth-to-stoma breathing Victim with dentures Suspected head, neck, or back injuries Try to minimize movement of the head and neck when opening the airway. Try to open the victim’s airway by lifting the chin without tilting the head back. Perform a jaw thrust – works better using BOTH hands. Place hands under the angles of the jaw and lifting Rescue Breathing for Children & Infants Uncorrected breathing emergencies in children and infants are the primary cause of cardiac arrest. Rescue breathing is the same as for adults, EXCEPT: 1 breath every 3 seconds use less air for each breath – breathe only until you see the chest rise you do not tilt a child’s or infant’s head as far back as an adult. Tilt it JUST enough so that air will go through breaths last only 1 second for infants, cover both the mouth and nose after 2 minutes of rescue breathing recheck breathing and pulse for no more than 10 seconds. Airway obstruction – most common cause of respiratory emergencies Common causes of choking include: trying to swallow large pieces of poorly chewed food drinking alcohol before or during meals -alcohol dulls the nerves that aid swallowing, making choking on food more likely) wearing dentures – harder to sense whether food is fully chewed eating while talking excitedly or laughing or eating too fast walking, playing, or running with food or objects in the mouth First Aid - Airway Obstruction - Conscious victim Conscious choking victim Get permission, identify yourself If coughing, encourage him to keep coughing Give 5 back blows with the heel of your hand Give 5 abdominal thrusts Yourself Obese or pregnant victim – chest thrusts Child Infant Care for an Unconscious Choking Adult: When you attempt 2 rescue breaths they do not go in: 1. Reposition the head 2. Give 2 slow breaths again. If they still don’t go in, assume the airway is blocked 3. Give 5 chest thrusts – adult about 1 ½ to 2 inches; child 1 to 1 ½ inches 4. Look inside victim’s mouth 5. Grasp tongue and lower jaw – if you see an object, take it out 6. Give 2 slow breaths – if they still don’t go in, repeat steps 1-6 Once air goes through, check for signs of circulation. Make sure you take the person to emergency department even when object is dislodged – may have internal damage due to thrusts and/or some of the material may still be in lungs. Care for an Unconscious Choking Infant Check for consciousness, and breathing If no breathing, attempt 2 slow breaths 1- If they do not go in, reposition the head and give 2 more breaths. If they still don’t go in, assume the airway is blocked 2- Give 5 back blows 3- Give 5 chest thrusts 4- Look for the object 5- IF you see it, try to remove with your little finger 6 – Open the airway and give two slow breaths 7-Keep repeating steps 1-6 until breaths go in, then check for signs of circulation.