Neuroscience 1 – Basic Organisation of the Nervous
advertisement

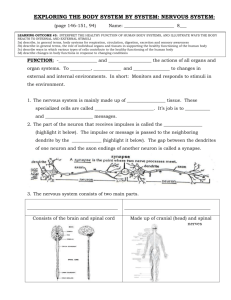
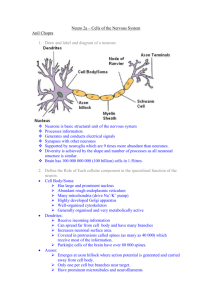
Neuroscience 1 – Basic Organisation of the Nervous system and Neurological Disorders Anil Chopra 1. Define the following terms used to describe the nervous system and explain how they interact with one another: -Central nervous system -Peripheral nervous system -Automatic nervous system -Somatic nervous system. Central nervous system: essentially the brain and spinal cord. Processes sensory and motor information and maintains internal environment. Involved with “higher functions”- memory emotion, cognition.e.t.c. Peripheral nervous system: the peripheral nerves and ganglia. Includes cranial and spinal nerves as well as their branches. It is subdivided into somatic and automatic (enteric) nervous systems to provide sensory and motor innervation to the body. Automatic nervous system: controls visceral function i.e. homeostasis, blood pressure, heart rate, breathing rate. Somatic nervous system: controls motor and sensory neurones from body wall. Other Notes: -Functions of the nervous system are mainly localised but some functional systems will consist of various structures which may be some distance apart but are connected by pathways. -Each cerebral hemisphere has a contralateral relationship with the side of the body it controls (i.e. it controls the other side), however some cerebral hemispheres represent particular higher functions such as language. -The functional unit of the nervous system is the neurone. Their cytoplasmic processthe axon-conducts impulses away from the body cell toward other neurones to muscle fibres. The points of contact one synapses. Many pathways with multiple neurones make up networks represented diagrammatically: 2. List major causes of neurological disorders and give examples. Causes of neurological disorders: Trauma e.g. spinal cord injury, skull fracture Cerebrovascular accident e.g. cerebrovascular infarct (stroke) Infection e.g. meningitis. Neoplasia. (cancer) e.g. glioma Metabolic disorders e.g. diabetic neuropathy. Genetic defect e.g. Down’s Syndrome Environmental Factors e.g. heavy metal encephalopathies. Immunological Factors e.g. multiple sclerosis Commonly, disorders arise from non neurological events. Causes of some “intrinsic” (e.g. autoimmune) neurological disorders are unknown. Loss of function => Abnormal function=> + Psychiatric disorders =altered behaviour with no signs of altered brain functions or pathology. Psychiatry and neurology overlap. 3. Give an example of a neurological disorder resulting from – Neuronal death &-neuronal dysfunction. Neuronal Death e.g. Parkinson’s disease. (Loss of dopaminergenic neurones in midbrain resulting in loss of control of voluntary movement. Also causes ach and dopamine imbalances.) Neuronal Dysfunction e.g. epilepsy (abnormal Synchronous firing of groups of neurones that can cause fits/seizures. Can spread and recruit other neurones. 4. State the difference in the regenerative capacity of injured axons between the CNS and PNS. Peripheral nervous system: nerves can regenerate after an injury, however reinnervation can often be non-specific and so some loss of function can result. Central Nervous system: axons cannot regenerate over distances that are long enough to be of any use. This is because inhibitory factors appear to be present and guidance cells are absent in fully grown central nervous systems. Intrinsic neuronal differences can also be a cause. 5. Describe the main components of a neurological examination. Diagnosis consists of 3 stages: (1) History: learn about the complaint, other condiotions, social settings, observation of the patient. (2) Neurological examination: assess…. a. Level of consciousness – Glasgow coma scale. b. Speech – just talk to patient c. Mental state and cognitive function – asking simple general knowledge/mathematical questions d. Cranial nerve function – e.g. eyelid strength, facial movements, gag reflex, smell, taste, hearing. e. Motor function – check for twitchage, feet touch, evaluation of strength of muscle groups. f. Sensory function – pain, temperature, pressure, and position tested. Usually this is repeated. 6. Outline the main electrophysiological and imaging techniques used in neurological diagnosis, noting the advantages and disadvantages. (3) Specific electrophysiological and imaging techniques Electroencephalography (EEG) Measures electrical potentials in scalp that are generated by the neurones beneath it. Produces traces known as electroencephalograms. Useful in diagnosing epilepsy and coma, good as it is non-invasive, has a very high time-resolution (milliseconds). It cannot however pick out individual action potentials. It also cannot target specific parts of anatomy. Electromyography (EMG) & Nerve Conduction Studies (NCS) The integrity of muscle, peripheral and lower motor neurones are all examined. Needles are placed into muscles and their electrical activity is measured. Nerve conduction velocity is frequently measured. Computerised Tomography (CT) X-rays are used to create 3D images and cross-sections of patients. It has a high resolution, and differences in tissue can be noted very easily. It does however deliver a high dose of radiation and is expensive. It is good for differentiating hard tissues. Magnetic Resonance Imaging (MRI) Uses changes in behaviour of hydrogen protons and a strong externally applied magnetic field is used. It is non-invasive and is good with differentiating soft tissues and can work in any plane. It is extremely expensive Angiography A contrast medium is injected and radiographs examine patients’ cerebral vessels. It is extremely useful for examining vasculature of the brain.