Old and New BPD
advertisement

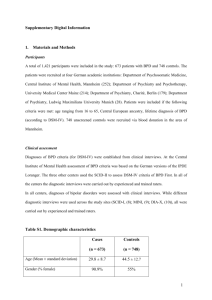
OLD BPD – NEW BPD OLD BRONCHOPULMONARY DYSPLASIA – NEW BRONCHOPULMONARY DYSPLASIA Hugh O’Brodovich MD, FRCP(C) Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA 94305 Running Title: OLD BPD – NEW BPD Address correspondence to: Hugh O’Brodovich MD, FRCP(C) Arline & Pete Harman Professor and Chairman Department of Pediatrics, Stanford School of Medicine Adalyn Jay Physician-in-Chief, Lucile Packard Children's Hospital Department of Pediatrics Stanford School of Medicine 300 Pasteur Drive , Room H310 Stanford , CA 94305-5208 Ph: (650) 723-5104 Fax: (650)725-7419 Hugh.OBrodovich@Stanford.edu 1 OLD BPD – NEW BPD Bronchopulmonary dysplasia (BPD) is the most common chronic lung disease of infants and its treatment imposes considerable health care burden and costs in the perinatal and early childhood period. Structural changes in the lung and impairment of function persist later in life, so survivors are likely at increased risk for chronic obstructive pulmonary disease (COPD), pulmonary hypertension, and perhaps other adult lung diseases. Since its first description (3), there have been remarkable changes in the clinical and pathologic phenotype. This evolution has led clinicians and researchers to use terms such as “Old BPD” and “New BPD” to differentiate the original from the currently most commonly seen phenotype. To help understand the differences between “Old BPD” and “New BPD” this brief review will utilize a “walk through history”. Neonatal Respiratory Distress Syndrome At one time the neonatal respiratory distress syndrome (nRDS) in the prematurely born human infant was called “idiopathic RDS” as we did not understand the pathophysiologic mechanisms underlying this serious disorder. Little could be done for these infants: in 1960 infants with nRDS at The Hospital for Sick Children in Toronto had a 50% mortality rate and nRDS was responsible for 30% of all hospital deaths. In 1959 Avery and Mead discovered that extracts from postmortem nRDS lungs had increased air-liquid surface tension and that they were deficient in dipalmitoyl lecithin. Although clinical trials using aerosolized lecithin followed shortly thereafter, this new “therapy” did not benefit infants with nRDS. Two decades of research would be required to identify the reasons for this failure, to determine the various components of surfactant and to create a clinically efficacious exogenous surfactant that would treat the “relative surfactant deficiency” which characterizes nRDS . During those two decades, infants with severe nRDS began to survive as neonatal intensive care units were created and physicians intervened with the use of continuous positive pressure ventilation and assisted ventilation. During that era, premature infants with nRDS either died during the few days after birth or in a comparable timeframe improved dramatically and survived with no significant long term pulmonary sequelae. Bronchopulmonary Dyplasia As a result of an improved understanding of the physiology of the premature lung, the pathophysiology of RDS and how to best utilize advances in technology, more infants began to survive severe nRDS. Some of these new survivors, however, did not show the marked improvement during the first week of life. In 1967, Bill Northway and colleagues recognized this form of unresolved lung injury and gave it the name bronchopulmonary dysplasia (BPD) (3). Although exceptions occurred, the disorder typically occurred in infants whose gestational ages (GA) were 30 – 36 weeks. More immature infants with severe nRDS rarely survived. BPD evolved in characterized stages. During the first week of life, the infant had the typical radiographic findings of nRDS (Stage I), a disorder characterized by relative surfactant deficiency, an inability to actively clear fetal lung liquid from its airspaces and 2 OLD BPD – NEW BPD an abnormal permeability of the alveolar capillary membrane permeability. However, towards the latter part of the first week post-partum there was not the typical spontaneous resolution as described above, but rather a worsening of the nRDS (Stage II). Thereafter the “stiff small lung disease”, which is characteristic of nRDS, evolved into a severe chronic obstructive pulmonary disorder which was frequently complicated by cor pulmonale (Stages III and IV). Clinically these latter stages were characterized by severe airflow limitation whilst the chest radiograph demonstrated marked over-inflation with multiple cystic areas interspersed with fibrotic linear densities. The pathologic findings of extensive airway and parenchymal damage in the presence of abnormal lung structure lead to its name, bronchopulmonary dysplasia. BPD was not diagnosed until one month of age and required the presence of 1) a respiratory disorder that began with acute lung injury; 2) postnatal age > 28 days; 3) significant clinical and radiologic findings consistent with the diagnosis and 4) blood gas tension abnormalities with PaO2 < 60 torr or PaCO2 > 45 torr whilst breathing room air at usual altitudes. Northway’s BPD, now known as “Old BPD”, is reviewed in (4). Infants who developed BPD and survived, often faced long periods of assisted ventilation followed by months to years of supplemental oxygen therapy in hospital and then at home during their phase of chronic hypercarbic respiratory failure. Their clinical course was usually very complex. They suffered from numerous complications: cor pulmonale, reactive airway disease, failure to thrive and other sequelae including significant neurodevelopmental delay. The first years of life were characterized by frequent hospitalizations. From the perspective of the respiratory system, infants usually improved significantly during the first few years of life with the vast majority of older infants and toddlers no longer needing supplemental oxygen therapy. It is presumed that, at least in part, this improvement occurred because alveolarization in the human lung continues after birth; full term healthy human infants have 20- 30 million alveoli and this number increases to approximately 300-600 million alveoli during infancy and childhood. Although patients with BPD improved, studies in the early 1990s showed that they had significant residual lung disease. The majority had significant airway obstruction and, although there was bronchial hyperreactivity, most of the deficit in FEV1 was not reversible with bronchodilators. “New BPD” Basic, translational and clinical research during the 1970s and 1980 led to dramatic improvements in the management of prematurely born infants with acute respiratory disease. In addition to many improvements in general intensive care, for example better nutrition and fluid balance, the most important interventions in relation to the lungs might be summarized as follows: 1) an improved understanding of the hormonal regulation of fetal lung maturation leading to the use of antenatal corticosteroids to mature the lung’s surfactant synthetic pathways prior to preterm delivery; 2) the identification of the various component of surfactant and their properties leading to the routine use of exogenous surfactant therapy for nRDS; 3 OLD BPD – NEW BPD 3) the recognition that the airway pressures that were “usually used” during assisted ventilation were causing lung injury; 4) a better understanding of physiologic effects of pH, PaCO2 and PaO2. Interventions 3) and 4) led physicians to have an “enhanced tolerance” of “abnormal” blood gases. Together this led to less hyperoxia and “gentler” ventilation which diminished treatment – related lung injury and led to a virtual disappearance of “Northway’s BPD” in the infants who were born at 30 – 36 weeks GA. The above improvements in clinical care also led to a dramatic improvement in the survival of very low birth weight (VLBW) infants who, at birth, weighed <1,500 gm. Physicians recognized that these markedly premature infants also frequently developed a chronic lung disease (CLD). However, although they required long term ventilator support and/or supplemental oxygen therapy, their CLD had a significantly different clinical phenotype from “Northway’s BPD”. Often there was minimal or mild nRDS during the first days post partum and the infant did not progress through the typical Stages I, II, III and IV of BPD described above. Their chest radiograph usually did not demonstrate the cystic areas with interspersed fibrosis and pathologic studies revealed profound differences in the histopathology of the lungs of such infants. There were only minor changes in the airways; the major abnormality was a marked reduction in the total alveolar number and alveolar surface area arising from a marked impairment of alveolar development (2). There no longer was a “B” in the “BPD” and there was minimal evidence of fibrosis in the interstitial or alveolar airspaces. Given the significant clinical, radiologic and pathologic differences between this new type of CLD in the prematurely born, this CLD seen in VLBW infants is now commonly referred to as “New BPD” (see review (1)). Since “New BPD” occurs in VLBW infants and there is a different phenotype there needed to be a change in diagnostic criteria from those utilized by Northway and colleagues. The current NIH consensus diagnostic criteria for BPD in infants born less than 32 weeks gestational age (5) is that mild BPD is diagnosed when the infant requires supplemental oxygen at 28 days after birth but is in room air at a post menstrual age (PMA) of 36 weeks. Moderate BPD is diagnosed when the infant reaches 36 weeks PMA and although still requires supplemental oxygen the requirements are for an FIO2 < 0.3. Severe BPD is diagnosed when a 36 week PMA infant requires an FIO2 > 0.3 and continuous positive airway pressure or mechanical ventilation. In contrast to the criteria for Northway’s BPD (“Old BPD”) neither radiographic nor clinical findings are part of the diagnostic criteria. Although much of the clinical phenotype is different, long term follow up studies of “New BPD” have demonstrated significantly impaired pulmonary function when survivors are studied during their school age and adolescent years (reviewed in (1)). Since even full term healthy infants who suffer from childhood respiratory disorders can have a predisposition to chronic obstructive pulmonary disease (COPD) one can speculate that “New BPD” will predispose adults to an even earlier onset of serious morbidity and mortality from COPD. Numerous mammal, primate and human studies have been undertaken in an attempt to better understand the pathogenesis of “New BPD”. A crucial point is that VLBW infants are born with lungs that are only in the canalicular and early saccular 4 OLD BPD – NEW BPD stages of lung development. This contrasts with the infants who developed “Old BPD”; they were typically born after 30 – 36 weeks gestation and at the time of birth their lungs that had reached the alveolar stage of fetal lung development. The VLBW infant’s more immature lungs are frequently exposed to different phenomena that are known to alter lung development. For example, exposure to glucocorticosteroids can impair alveolar septation, inflammatory mediators arising from low level or overt chorioamnionitis can result in alveolar simplification and vascular injury and fetal growth restriction can negatively affect lung development. A currently favored hypothesis is that a failure of normal angiogenesis causes or contributes to the failure of normal alveolar development. Two recent twin studies support a strong genetic contribution to the risk of new BPD and suggest that heritability (h2) for new BPD is at least as large and probably greater than that for systemic hypertension (h2 ~30%), cancer (~40%), and psychiatric disorders (~60). How these various factors interact and result in failure of the distal lung unit to undergo normal development, and result in fewer and larger “alveoli”, is largely unknown. 1. Baraldi E and Filippone M. Chronic lung disease after premature birth. N Engl J Med 357: 1946-1955, 2007. 2. Margraf LR, Tomashefski JF, Jr., Bruce MC and Dahms BB. Morphometric analysis of the lung in bronchopulmonary dysplasia. Am Rev Respir Dis 143: 391400, 1991. 3. Northway WHJr, Rosan RC and Porter DY. Pulmonary disease following respiratory therapy of hyaline-membrane disease: Bronchopulmonary dysplasia. N Engl J Med 276: 357-367, 1967. 4. O'Brodovich H and Mellins RB. Bronchopulmonary dysplasia: Unresolved neonatal acute lung injury. Am Rev Respir Dis 132: 694-709, 1985. 5 OLD BPD – NEW BPD 5. Walsh MC, Szefler S, Davis J, Allen M, Van ML, Abman S, Blackmon L and Jobe A. Summary proceedings from the bronchopulmonary dysplasia group. Pediatr 117: S52-S56, 2006. 6