General Information Infections Disease and Barrier Precautions
advertisement

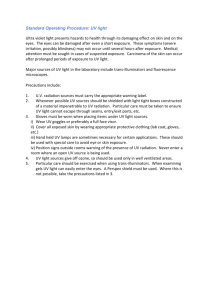
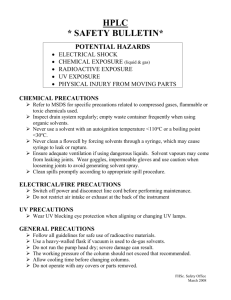
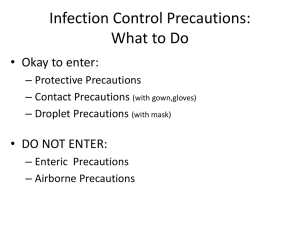
General Information Infections Disease and Barrier Precautions Page 1 Introduction Based on the latest information on the transmission of infections in hospitals, The Centers for Disease Control/Hospital Infection Control Practices Advisory Committee (HICPAC) has revised the The Guideline for Isolation Precautions in Hospitals with the recommendation that hospitals and patient care institutions implement Standard Precautions in the place of Universal Precautions. Standard Precautions correlates with Universal Precautions with minor revisions in nomenclature only. Additional categories of Airborne, Droplet, and Contact Precautions have been developed to manage specific diseases transmitted via such routes. The concept of isolating patients with transmissible diseases is the cornerstone of a hospital's program of infection prevention and control. This concept is an outgrowth of earlier practices where persons diagnosed with a transmissible infectious disease were "quarantined." Traditional systems of isolation precautions have relied on an understanding of the mechanisms by which disease can be spread and have focused the use of protective barrier equipment, such as gloves, gowns, masks, and protective eyewear in order to interrupt transmission and to break the chain of infection. Universal precautions: approaches to infection control designed to prevent transmission of bloodborne diseases, such as AIDS and hepatitis B in health care settings. Universal precautions were initially developed in 1987 by the Centers for Disease Control and Prevention (CDC) and in 1989 by the Bureau of Communicable Disease Epidemiology in Canada. The guidelines include specific recommendations for use of gloves and masks and protective eyewear when contact with blood or body secretions containing blood or blood elements is anticipated. In 1996 the CDC expanded the concept and changed the term to standard precautions Standard precautions: guidelines recommended by the Centers for Disease Control and Prevention for reducing the risk of transmission of blood-borne and other pathogens in hospitals. The standard precautions synthesize the major features of universal precautions (designed to reduce the risk of transmission of bloodborne pathogens) and body substance isolation (designed to reduce the risk of pathogens from moist body substances) and apply them to all patients receiving care in hospitals regardless of their diagnosis or presumed infection status. Standard precautions apply to (1) blood; (2) all body fluids, secretions, and excretions except sweat, regardless of whether or not they contain blood; (3) nonintact skin; and (4) mucous membranes. The precautions are designed to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources of infection in hospitals. Depending on the anticipated potential exposure, it may include only gloves, for example if you are doing a simple venapuncure or may include mask and gloves for intubation. Standard Precautions combine the major features of Universal Precautions and Body Substance Isolation (BSI) and are based on the principle that all blood, body fluids, secretions, excretions except sweat, nonintact skin, and mucous membranes may contain transmissible infectious agents. Standard Precautions include a group of infection prevention practices that apply to all patients, regardless of suspected or confirmed infection status, in any setting in which healthcare is delivered These include: hand hygiene; use of gloves, gown, mask, eye protection, or face shield, depending on the anticipated exposure; and safe injection practices. Also, equipment or items in the patient environment likely to have been contaminated with infectious body fluids must be handled in a manner to prevent transmission of infectious agents (e.g. wear gloves for direct contact, contain heavily soiled Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 1 General Information Infections Disease and Barrier Precautions Page 2 equipment, properly clean and disinfect or sterilize reusable equipment before use on another patient). The application of Standard Precautions during patient care is determined by the nature of the HCW-patient interaction and the extent of anticipated blood, body fluid, or pathogen exposure. For some interactions (e.g., performing venipuncture), only gloves may be needed; during other interactions (e.g., intubation), use of gloves, gown, and face shield or mask and goggles is necessary. Education and training on the principles and rationale for recommended practices are critical elements of Standard Precautions because they facilitate appropriate decision-making and promote adherence when HCWs are faced with new circumstances. An example of the importance of the use of Standard Precautions is intubation, especially under emergency circumstances when infectious agents may not be suspected, but later are identified (e.g., SARS-CoV, N. meningitides). The application of Standard Precautions is described below and summarized in in my attached word document which summarized most of the general information about barrier precautions and the methods to implement to implement to protect the Health Care Worker. (HCW). Barrier Protection The type of protective apparel chosen depends on the clinical situation and the type of patient care interaction that is anticipated. The selection of barrier protection, equipment, or work practice should include consideration of the following issues: Probability of exposure to blood and body Amount of blood or body substances likely to be encountered Probable route of transmission Gloves Gloves are worn to prevent the health care worker's hands from becoming contaminated with blood or body substances. Gloves should be worn for: Procedures involving direct contact with the blood and body substances of any patient Procedures where contact with blood and body substances might be expected to occur Procedures involving direct or potential contact with the mucous membranes of any patient. Procedures involving direct or potential contact with the non-intact skin of any patient. Non-intact skin is skin that is cut, chapped, abraded, cracked, afflicted with weeping or exudative lesions, or is otherwise broken Touching or handling any instruments, equipment, or surfaces that have been, or may have been, in contact with blood or body substances. In addition, gloves should be worn in providing care to a patient or in managing equipment when the health care worker has cuts, scratches, or other breaks in the skin on his/her hands. Sterile gloves should be used for all sterile procedures and for activities that involve contact with areas of the body that are normally sterile. There should be an adequate supply of clean disposable gloves on the standard Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 2 General Information Infections Disease and Barrier Precautions Page 3 precautions stations or in other locations that are convenient to each patient's room. Gloves used in patient's care should be worn only for contact with the patient. Once used, gloves must be discarded before leaving the patient's room. Masks Standard surgical masks are to be used: When splashing, splattering, or spraying of blood or body fluids is likely in order to prevent exposure to the mucous membranes of the nose/mouth. Additionally, eye protection is warranted in such situations as well. When within 3 feet of a patient on Droplet Precautions. When working in a sterile field to prevent droplets from contaminating the field. Surgical masks do NOT provide adequate protection for those diseases spread by the airborne route (i.e., Mycobacterium tuberculosis). For suspected or confirmed patients with pulmonary TB, a N-95/HEPA respirator must be worn. Gowns Gowns, aprons, and other protective apparel are worn to prevent clothing from becoming soiled with blood and body substances. Selection of the appropriate type of protective apparel is based on the amount of blood and body substances likely to be encountered and the probability that clothing may by soiled. Gowns should be worn: During activities that involve the management of large amounts of blood or body substances that may be difficult to contain properly. During procedures that may result in the splashing or splattering of blood or body substances. Gowns should be: Large enough to cover the clothing which is likely to be contaminated. Made of a moisture-resistant material that provides an effective barrier to body substances. Sterile gowns should be worn for procedures that require a sterile field. Gowns should be changed: After giving care to an individual patient. After performing any procedure involving instruments, equipment, or surfaces contaminated Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 3 General Information Infections Disease and Barrier Precautions Page 4 by blood or body substances. Whenever gross soiling occurs. Discard used gowns in the patient care area or in the other areas in which they were used. Protective Eyewear Protective eyewear is worn to prevent blood and body substances from contaminating the mucous membranes of the eyes. Protective eyewear is available by request for employee use and will be replaced if lost or damaged. In hospital areas where non-hospital employees routinely work, such as in the Labor and Delivery Unit, protective eyewear, as well as other barrier protection equipment, will be available in a central location for use by these persons. Protective eyewear should be worn during procedures where blood and body substances may be expected to splash or splatter. Face Shields Face shields are worn to prevent blood and body substances from contaminating the mucous membranes of the eyes, nose, and mouth during procedures which may cause splashing or splattering. If blood and body substances are expected to become aerosolized during a procedure, a mask should also be worn. Non-disposable face shields should be removed and cleaned after each use with soap and water and dried with a paper towel. If visibly soiled, wipe the face shield with a 70% alcohol solution. Respirators Respirators are masks specifically designed to filter small particles spread by the airborne route. Current OSHA standards as developed by NIOSH (National Institute for Occupational Safety & Health) require that respirators used for Airborne Precautions for supected/confirmed pulmonary tuberculosis minimally filter 95% of 0.3µm sized particles. The two respirators which meet these requirements are: the N-95 respirator and HEPA respirator. All personnel who care for a patient with suspected/confirmed pulmonary TB must wear an N-95/HEPA respirator upon entering the room of such a patient. Personnel using a N-95/HEPA respirator must be fit-tested before using either respirator. If one has been previously fit-tested for a HEPA respirator, one must be fittested again before using a N-95 respirator. Fit-testing can be arranged through YNHH Occupational Health Services (8-2462). Transmission-Based Precautions Transmission-Based Precautions are designed for patients documented or suspected to be infected/colonized with highly transmissible or epidemiologically important pathogens Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 4 General Information Infections Disease and Barrier Precautions Page 5 for which additional precautions beyond Standard Precautions are needed to interrupt transmission. The three categories of Transmission-Based Precautions include: Airborne Precautions Droplet Precautions Contact Precautions These categories may be combined for diseases that have multiple routes of transmission. When used either singularly or in combination, they are to be used in addition to Standard Precautions. Airborne Precautions Airborne Precautions are designed to reduce the risk or eliminate the airborne transmission of infectious agents. Airborne transmission occurs by dissemination of either airborne droplet nuclei (small-particle residue-5 um or smaller sized evaporated droplets which remain suspended in the air for long periods of time) or dust particles containing the infectious agent. Microorganisms carried in this manner can be dispersed widely by air currents and may become inhaled by or deposited on a susceptible host within the same room or over a longer distance from the source patient, depending on environmental factors; therefore, special air handling and ventilation (i.e. negative pressure isolation) are required to prevent airborne transmission. Airborne Precautions apply to patients known or suspected to be infected with epidemiologically important pathogens that can be transmitted by the airborne route, (e.g. Mycobacterium tuberculosis). Droplet Precautions Droplet Precautions are designed to reduce the risk of droplet transmission of infectious agents. Droplet transmission involves contact of the conjunctivae or the mucous membrances of the nose or mouth of a susceptible person with large-particle droplets (larger than 5 um in size) containing microorganisms generated from a person who has a clinical disease or who is a carrier of the microorganism. Droplets are generated by the source person during coughing, sneezing, or talking and/or during the performance of certain procedures such as suctioning and bronchoscopy. Transmission via large-particle droplets requires close contact between source and recipient persons, because droplets do not remain suspended in the air and generally travel only short distances, usually 3 ft or less. Since droplets do not remain suspended in the air, special air handling and ventilation are not required to prevent droplet transmission. Droplet Precautions apply to any patient known or suspected to be infected with epidemiologically important pathogens that can be transmitted by infectious droplets. Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 5 General Information Infections Disease and Barrier Precautions Page 6 Contact Precautions Contact Precautions are designed to reduce the risk of transmission of epidemiologically important microorganisms by direct or indirect contact. Direct contact transmission involves skin-to-skin contact and physical transfer of microorganisms to a susceptible host from an infected or colonized person, such as occurs when personnel turn patients, bathe patients, or perform other patient-care activities that require physical contact. Direct contact transmission also can occur between two patients (e.g., by hand contact), with one serving as the source of infectious microorganisms and the other as a susceptible host. Indirect contact transmission involves contact of a susceptible host with a contaminated intermediate object, usually inanimate, in the patient's environment. Contact Precautions apply to patients known or suspected to be infected or colonized (presence of microorganism in or on patient but without clinical signs and symptoms of infection) with epidemiologically important microorganisms that can be transmitted by direct or indirect contact. Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 6 General Information Infections Disease and Barrier Precautions Page 7 RECOMMENDATIONS FOR APPLICATION OF STANDARD PRECAUTIONS FOR THE CARE OF ALL PATIENTS IN ALL HEALTHCARE SETTINGS (See Sections II.D.-II.J. and RECOMMENDATIONS III.A.1) COMPONENT Hand hygiene After touching blood, body fluids, secretions, excretions, contaminated items; immediately after removing gloves; between patient contacts. Personal protective equipment (PPE) Gloves For touching blood, body fluids, secretions, excretions, contaminated items; for touching mucous membranes and nonintact skin Gown During procedures and patient-care activities when contact of clothing/exposed skin with blood/body fluids, secretions, and excretions is anticipated.. Mask, eye protection During procedures and patient-care activities likely to generate splashes or sprays of blood, (goggles), body fluids, secretions, especially suctioning, endotracheal intubation face shield* Soiled patient-care equipment Handle in a manner that prevents transfer of microorganisms to others and to the environment; wear gloves if visibly contaminated; perform hand hygiene. Environmental control Develop procedures for routine care, cleaning, and disinfection of environmental surfaces, especially frequently touched surfaces in patient-care areas. Textiles and laundry Handle in a manner that prevents transfer of microorganisms to others and to the environment Do not recap, bend, break, or hand-manipulate used needles; if recapping is required, use a Needles and other sharps one-handed scoop technique only; use safety features when available; place used sharps in puncture-resistant container Patient resuscitation Use mouthpiece, resuscitation bag, other ventilation devices to prevent contact with mouth and oral secretions Source: http://www.med.yale.edu/ynhh/infection/precautions/intro.html Page 7