Table of Contents To Err is Human…. to Collaborate is Divine
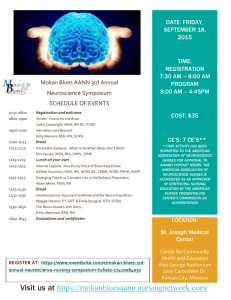
advertisement

Table of Contents To Err is Human…. to Collaborate is Divine…Collaboration: The Key to Positive Patient Outcomes and Professional Satisfaction ..................................................................2 The influence a Nurse-Driven Palliative Care Screening Tool Has on the Timing of Palliative Care Consults ......................................................................................................3 Effectiveness of Periop 101: A Core Curriculum ™ in the Orientation of the Novice Perioperative Nurse ..............................................................................................................4 Effectiveness of Nurses’ Preparedness in Education and Assessment of Patients Receiving Oral Cancer Therapies ........................................................................................5 The Impact of Pre-Procedure Phone Calls in an Endoscopy Suite ......................................6 Exploring the Role of the Nurse in the Care and Support of Autistic Children and Their Family: A Family Resilience Approach .....................................................................7 Cardiac Rehabilitation Enrollment: A Study of the Effects of Patient Education ..............8 Assessment of Education Regarding Heart Attack Symptoms and the Proper Response ...9 The Integration of Spirituality in Nursing Curriculum: Improving Spiritual Care of Patients ...............................................................................................................................10 August 2014 MSN Capstone Project Page 1 To Err is Human…. to Collaborate is Divine Collaboration: The Key to Positive Patient Outcomes and Professional Satisfaction Kimberly Johnson, MSN(c), BSN, RNC-NIC Immaculata University Significance The Institute of Medicine, and the American Association of Colleges of Nursing, are two major organizations that call for innovative measures to ensure optimal patient outcomes. Effective nurse physician collaboration is essential to achieve these outcomes. Introducing opportunities for nurses and physicians to collaborate in staff education sessions may increase the respect the two disciplines have for one another and may increase awareness of the unique knowledge and skills each contributes to the safe delivery of health care. Purpose/Aim Provide an opportunity for physician and nurses to work together in disseminating information to bedside caregivers. This collaborative effort may increase respect for individual roles, improve job satisfaction and ultimately lead to optimal health outcomes. Jean Watson’s Caring Science Theory will be applied to this as it addresses respect for roles as they impact professional satisfaction. Method This action research study will gather data from a recent hospital National Database of Nursing Quality Indicators (NDNQI) survey, focusing on questions regarding nurse physician collaboration and perception of each other’s role in health care delivery to newborns in a 12-bed Neonatal Intensive Care Nursery. A review of evidence-based research and strategies will be utilized to develop opportunities for nurses and physicians to co- present at lectures. Results/Interpretations Trust and respect for interdisciplinary roles are affected by multiple variables, which are discussed in this proposal. Results of future NDNQI survey will be analyzed to indicate if co-presenting lectures improved communication and respect for nurse physician roles. Conclusion/Implications Positive feedback came from physicians and nurses indicated interest in improving collaboration by co-presenting lectures. External variables impact ability for nurses and physicians to work collaboratively. Increased training on communication and presentation skills should be implemented to improve collaborative efforts. August 2014 MSN Capstone Project Page 2 The Influence a Nurse-Driven Palliative Care Screening Tool Has on the Timing of Palliative Care Consults Joyce R. Kish, MSN(c), BSN, RN, CCRN Immaculata University Significance Chronic illnesses such as cancer and heart disease are rising in the U.S. When the burden of treatments for the individual exceeds their benefit it is appropriate to involve the Palliative Care Team. Physicians often consider a palliative care consult (PCC) as a last resort. Palliative care offers the patient an option to focus on quality-of-life issues while allowing them to live with dignity and control. Purpose/Aim The purpose of this action research project is to identify the triggers for a PCC and use them to develop a nurse-driven palliative care screening tool. Development of a screening tool to facilitate communication between nurses and physicians will assist in identifying the need for a PCC earlier in the patient's disease process. Methods A retrospective review of 30 electronic medical records was completed for patients that received a PCC during April 2014. Through collaboration with the hospital's Palliative Care Team a nurse-driven screening tool was developed. Results/Interpretation The study revealed the top two diagnoses were acute respiratory failure and cancer. Primary triggers for a PCC were pain and dyspnea. The leading reasons for a PCC were symptom management and discussion of code status. Of the 30 patients reviewed there were 10 deaths which occurred within hours and up to 11 days after the PCC. Conclusion and Implications When a PCC occurs hours or days prior to the patient dying they are deprived of the physical and psychological support the Palliative Care Team can offer. Nurses are in the perfect position to facilitate earlier PCCs. The use of a screening tool will standardize information used to communicate with the physician promoting a positive effect on earlier timing of a PCC. August 2014 MSN Capstone Project Page 3 Effectiveness of Periop 101: A Core Curriculum ™ in the Orientation of the Novice Perioperative Nurse Rosalyn J. McGrath, MSN(c), BSN, RN, CNOR Immaculata University Significance Healthcare institutions across the country are facing an unparalleled nursing shortage. Contributing factors include an aging baby-boomer population nearing retirement age and a high turnover rate among new graduate hires. Many Perioperative leaders report difficulty in filling staff positions. In a high risk clinical area such as the Perioperative Area, a quality driven, evidence-based orientation program is critical to safe patient care. Critical thinking skills must also increase in this environment due to the rapid pace and increasing acuity of patients. Nurse educators have a professional and ethical responsibility to ensure novice nurses gain the confidence and are competent to be successful in the Perioperative setting. Purpose The purpose of this action research project is to evaluate the effectiveness of Periop 101 as a learning platform for novice perioperative nurses in relation to safety, cost, confidence and competence. Method An action research approach was used to survey the perioperative staff as the novices were rotating through their clinical specialties. Also, ongoing evaluations of competencies, test scores, self-evaluation, and practice errors were examined among the novices. A cost benefit analysis was also used to determine if Periop 101 is more costeffective than a department based program. Results/Interpretation The findings in this study emphasize the effectiveness of an evidence-based, quality driven, orientation program. The implementation of Periop 101 as a learning platform enhances the skills, competence, and confidence which are fundamental to the success of a nurse new to the perioperative area. Conclusion/Implications Preparation of the novice perioperative nurse with an evidence-based quality orientation program can lead to a safe, successful and rewarding career. Novice nurses who transition from the novice to advanced beginner are competent, confident, satisfied, and committed to their organization. An area where further research is needed is in the effectiveness of the program over time. August 2014 MSN Capstone Project Page 4 Effectiveness of Nurses’ Preparedness in Education and Assessment of Patients Receiving Oral Cancer Therapies Mary C. Rooney, MSN(c), BSN, RN, OCN, CBCN Immaculata University Significance The paradigm in cancer care is changing with oral cancer therapy accounting for an estimated 25% of treatments. This shift in care provides an opportunity for nurses to be leaders in this modality of cancer treatment. Historically, nurses have been educating patients receiving cancer therapy for years, at the bedside, and in infusion suites. Nurses giving these treatments are required to be certified. With oral cancer therapy patients are responsible for obtaining, administering, adhering and managing side effects of oral cancer therapy. Education and assessment is even more important for both nurses and patients. Nurses must be prepared to take the lead in educating and assessing for barriers prior to the initiation of oral cancer therapy and provide continued support to patients to promote safety, efficacy and improved patient outcomes. Purpose This action research study will examine the preparedness and current practices among nurses in various settings who are responsible for the education and assessment of patients receiving oral cancer therapies in order to set standards to improve safety and outcomes for patients. Method An action research approach was used to survey nurses who currently work in oncology care. Causal conversations among colleagues both in the community and academic settings were conducted. Information was also obtained by professional nursing blogs and by observation. Results Information collected supports that nurses are not prepared or confident in the changing paradigm of cancer care. Among practices no standardization exists, no formal training is provided or required in contrast to parental chemotherapy administration. Conclusion Nurses need to be prepared to educate and assess patients on complex oral cancer therapies. Effectiveness will reduce adverse events, increase adherence and lead to improvements in efficacy and safety for patients. Further research is required to identify strategies to implement an educational requirement for nurses in this role. August 2014 MSN Capstone Project Page 5 The Impact of Pre-Procedure Phone Calls in an Endoscopy Suite Marianne D. Saunders, MSN(c), BSN, RN Immaculata University Significance Outpatient Endoscopy Suites experience high numbers of patient no-shows and cancellations. Depending on the procedure, preparation can be complicated, unpleasant, distasteful, embarrassing, and disruptive of one’s daily routine. Colonoscopy is one endoscopic procedure that involves the ingestion of a purging agent and evacuation of the bowels. The prepping process can be daunting for some individuals, influencing their decision to make or break their appointment. Gastroenterology nurses can take an active role in educating patients on adherence to procedural instructions. Through use of preprocedure phone calls, nurses can positively influence patient outcomes and decrease the no-show rate in the Endoscopy Suite. Purpose/Aim The purpose of this action research is to develop a process to communicate with patients prior to their procedure and address the barriers to arriving to their scheduled appointment. This requires an appreciation of their knowledge base of the procedure as well as the preparatory instructions. Patients’ comprehension plays a vital role in the success of their endoscopic procedure. Method Phone calls will be made to patients one week prior to their procedure. Review of the electronic medical record will provide a guide for the nurse caller to assess the patients’ medical history, discuss and document concerns, and communicate to key medical team members in preparation for the endoscopic procedure. Results/Interpretations A weekly electronic report of patient no-shows and cancellations was compared to identical data prior to intervention of phone calls. The report demonstrated a decrease in no-show and cancellation rate of patients arriving for their endoscopic procedures. Conclusions/Implications Pre-procedural calls can identify knowledge deficits and enhance preparatory behaviors. Improved knowledge is likely to bring about a commitment to compliance and a decrease in the no-show and cancellation rates. August 2014 MSN Capstone Project Page 6 Exploring the Role of the Nurse in the Care and Support of Autistic Children and Their Family: A Family Resilience Approach Celina M. Siwula, MSN(c), MEd, BSN, RN, CSN, CLNC Immaculata University Significance Nurses are caring for an increasing number of children with autism spectrum disorders (ASD). The nurse must foster family resilience and have an understanding of the child’s perceptions and special needs in order to achieve positive outcomes for the child. Families of children with a diagnosis of ASD lead lives that are full of challenges and adversity. Family resilience theory must be fostered by cultivating family strengths and providing supports. Purpose/Aim The purpose of this action research is to explore the application of family resilience theory in the care and support of children with ASD in the school setting. The aim of this study is to improve care and achieve positive outcomes for the children and their families. Methods Following a pre-intervention survey, a family resilience pamphlet was given to each participant to reinforce knowledge about the use of family resilience theory. This was followed by an informal discussion and a simulation activity that provided each participant with a series of stimulatory interruptions that are common to children with an ASD. A debriefing session was held after the simulation. A post-intervention survey was done to determine if the interventions improved care and outcomes. Results/Interpretation The results of this study suggest that patients with an ASD benefit when nurses who care for them understand and foster family resilience. After participating in the simulation, participants had a clearer understanding of the struggles of the ASD patient and positive patient and family outcomes were demonstrated. Conclusion/Implications The fostering of the theory of family resilience should be further investigated with a broader sample which includes other members of the multidisciplinary team of which the nurse is a part. August 2014 MSN Capstone Project Page 7 Cardiac Rehabilitation Enrollment: A Study of the Effects of Patient Education Lisa Springer, MSN(c), BSN, RN, PCCN Immaculata University Significance Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in the U.S. Despite the American Heart Association (AHA) support of cardiac rehabilitation (CR) in the secondary prevention of CVD, less than one-third of patients enroll after an acute coronary syndrome (ACS). CR develops health habits that lower coronary risk profile and improve quality of life after a cardiac event. The AHA calls for the study of interventions to understand how nurses can promote CR enrollment and build a transition from hospital to home. Purpose The action research project will study the effects of a nurse intervention focused on patient education to improve CR enrollment among individuals hospitalized for ACS. The study uses Leventhal’s Self-regulatory Model (SRM) as a framework to influence health beliefs and health behaviors in relation to five attributes of ACS and rates of CR enrollment. Method A Clinical Nurse Leader (CNL) applies the five attributes of ACS using an individualized teaching plan during one-to-one sessions. The CNL education session focuses on perception of ACS as controllable, serious, and caused by internal factors related to CVD that are amenable to change through CR enrollment. Trends in relation to the efficacy of patient education and CR enrollment are under examination for 12 weeks. Results/Interpretation Baseline data for the past 6 months indicates that 18% of patients treated for an ACS have enrolled in CR at the study site. An improvement in CR enrollment rates will support the use of patient education as a therapeutic nursing intervention. Future Implications Further research on using the model as a nurse intervention in other cardiac illnesses may prove useful to promote CR as a transitional program from hospital to home. Nursing plays a key role in the study of interventions to advance cardiac outcomes and promote quality of life. August 2014 MSN Capstone Project Page 8 Assessment of Education Regarding Heart Attack Symptoms and the Proper Response Duane Stanton, MSN(c), BSN, RN Immaculata University Significance Cardiovascular disease is the number one cause of death in the United States. One form of heart disease, myocardial infarction (MI) is responsible for the majority of these deaths. Studies show that more than half of cardiovascular deaths are due to acute myocardial infarction (AMI), causing a quarter of a million people to die within one hour of symptom onset and before reaching a hospital. The majority of patients do not seek care within two hours of symptom onset. Two factors that cause delay are seeking the opinion of others and not calling EMS. Purpose Knowledge and recognition of heart attack symptoms is important in order to respond appropriately. The aim of this study was to explore if heart attack education at one hospital effectively addresses heart attack symptoms and the appropriate response. Items of interest were whether education was consistent across all units, and whether spouses and significant others were targeted to receive the same education- as consultation with others has been shown to affect delay in seeking care. Methods Interviews were conducted with staff whose responsibilities include education of patients admitted with AMI. Information collected included material used for education, when education was delivered and by whom, and whether education was identical for all heart attack patients. Results/Interpretation The process of education of AMI patients was uneven across all units, the word “inconsistent” was used by staff to describe the education process. An inconsistent approach to the education of these patients, who are at risk for a subsequent MI, for how to respond in the event of an MI is concerning. Conclusion/Implications The educational process should be delivered more uniformly. Patient’s significant others should be specifically targeted to receive the same information as the patient, to act as a support in case of recurrent MI. August 2014 MSN Capstone Project Page 9 The Integration of Spirituality in Nursing Curriculum: Improving Spiritual Care of Patients Lauren E. Stoltzfus, MSN(c), BSN, RN Immaculata University Significance Caring for a patient as a whole, including their mind, body, and spirit, is essential in overall patient care and patient satisfaction. Spirituality, specifically, can play a significant role in a patient’s life as he/she experiences illness, challenges, and even death. Often nurses have difficulty in providing spiritual care because of the lack of preparedness provided in their basic nursing education. By incorporating spirituality into nursing curriculum, nurses will promote their own spiritual growth, thus laying an essential foundation for providing spiritual care to others. Purpose The purpose of this action research study is to examine if the integration of spirituality into nursing curriculum improves students’ ability to recognize and care for patients’ spiritual needs. Methods An action research method was used to assess the incorporation of the concept of spirituality into the Medical Surgical I course of a practical nursing program. The utilization of case studies, role play, and lecture educated the nursing students on how to assess a patient’s spirituality as well as meet his/her spiritual needs. After implementing lessons on spirituality, the effectiveness of the teaching was evaluated by NCLEX style pilot questions and nursing care plans of the researcher’s clinical group of students. Results/Interpretation The findings in this study revealed that integrating spirituality into the Medical Surgical I nursing course allowed spiritual growth among practical nursing students. Furthermore, addressing the spiritual needs of patients occurred more frequently. Conclusion/Implications Having an understanding of one’s own spirituality allows nursing students to better care for their patients and their spiritual needs. Threading spiritualty throughout the nursing program rather than one course will allow for further spiritual growth and essentially allow for patient’s spiritual needs to be met. In conclusion, providing spiritual care will improve overall patient satisfaction. August 2014 MSN Capstone Project Page 10