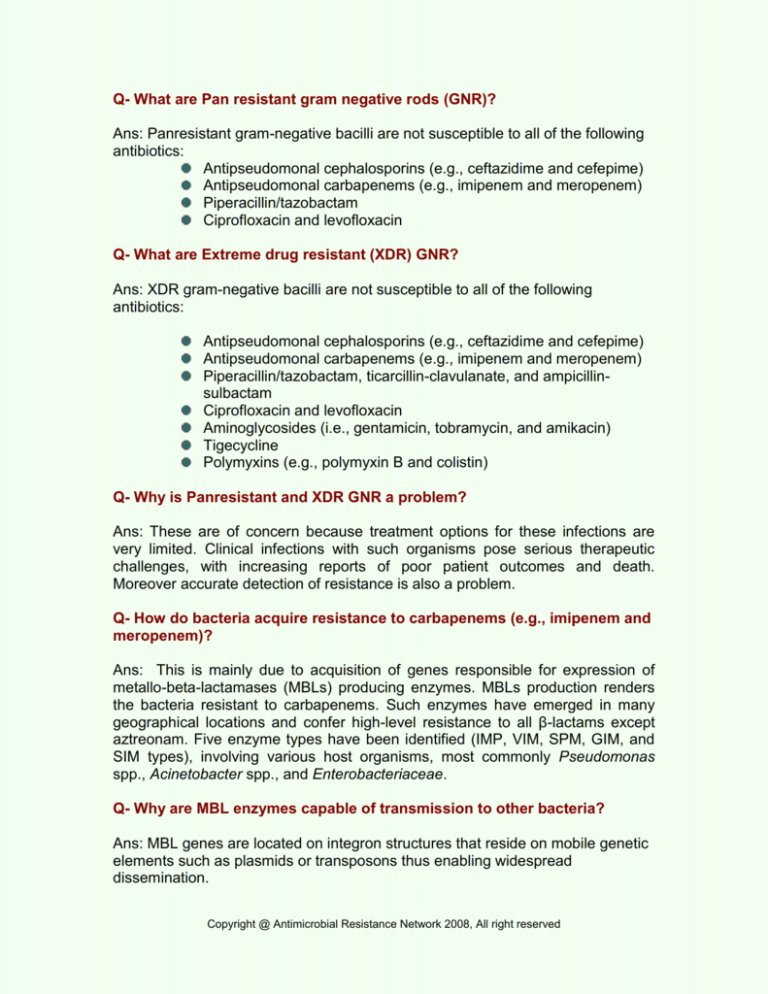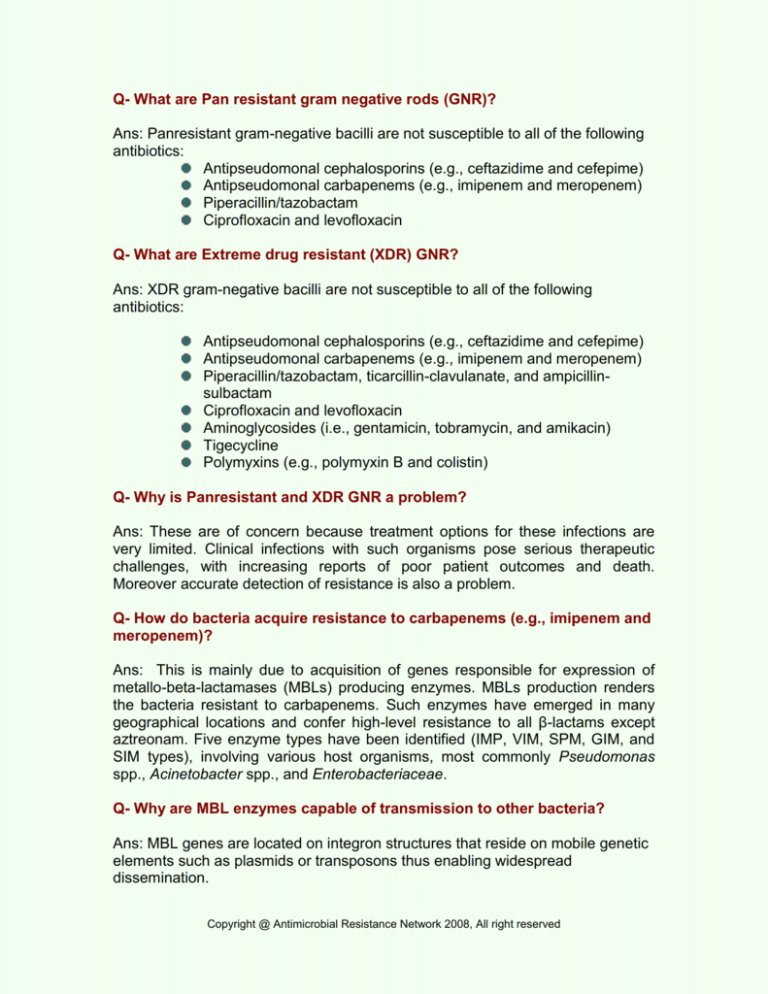
Q- What are Pan resistant gram negative rods (GNR)?
Ans: Panresistant gram-negative bacilli are not susceptible to all of the following
antibiotics:
Antipseudomonal cephalosporins (e.g., ceftazidime and cefepime)
Antipseudomonal carbapenems (e.g., imipenem and meropenem)
Piperacillin/tazobactam
Ciprofloxacin and levofloxacin
Q- What are Extreme drug resistant (XDR) GNR?
Ans: XDR gram-negative bacilli are not susceptible to all of the following
antibiotics:
Antipseudomonal cephalosporins (e.g., ceftazidime and cefepime)
Antipseudomonal carbapenems (e.g., imipenem and meropenem)
Piperacillin/tazobactam, ticarcillin-clavulanate, and ampicillinsulbactam
Ciprofloxacin and levofloxacin
Aminoglycosides (i.e., gentamicin, tobramycin, and amikacin)
Tigecycline
Polymyxins (e.g., polymyxin B and colistin)
Q- Why is Panresistant and XDR GNR a problem?
Ans: These are of concern because treatment options for these infections are
very limited. Clinical infections with such organisms pose serious therapeutic
challenges, with increasing reports of poor patient outcomes and death.
Moreover accurate detection of resistance is also a problem.
Q- How do bacteria acquire resistance to carbapenems (e.g., imipenem and
meropenem)?
Ans: This is mainly due to acquisition of genes responsible for expression of
metallo-beta-lactamases (MBLs) producing enzymes. MBLs production renders
the bacteria resistant to carbapenems. Such enzymes have emerged in many
geographical locations and confer high-level resistance to all β-lactams except
aztreonam. Five enzyme types have been identified (IMP, VIM, SPM, GIM, and
SIM types), involving various host organisms, most commonly Pseudomonas
spp., Acinetobacter spp., and Enterobacteriaceae.
Q- Why are MBL enzymes capable of transmission to other bacteria?
Ans: MBL genes are located on integron structures that reside on mobile genetic
elements such as plasmids or transposons thus enabling widespread
dissemination.
Copyright @ Antimicrobial Resistance Network 2008, All right reserved
Q- Why MBLs production is necessary to detect in a routine clinical
laboratory?
Ans: Globally occurrence, types, and rate of dissemination of MBLs is increasing,
therefore early detection is critical. The benefits of such include timely
implementation of strict infection control practices as well as clinical guidance
regarding the potential risks for therapeutic failure. Moreover, given the poor
outcomes, such as death, persistent fevers, and infection relapse, laboratory
detection of carbapenem-susceptible MBL-carrying organisms should be
considered to be of paramount clinical importance.
Q- Is MBLs production easy to detect in laboratory?
Ans: No, because as seen with extended-spectrum β-lactamases (ESBL) and
AmpC-type β-lactamases, MBL-carrying organisms can appear susceptible to
carbapenems using current Clinical and Laboratory Standards Institute (CLSI) or
British Society for Antimicrobial Chemotherapy (BSAC) breakpoints. As a result
of being difficult to detect, such organisms pose significant risks, particularly due
to their role in unnoticed spread within institutions and their ability to participate in
horizontal MBL gene transfer with other pathogenic hospital-related organisms.
Q- How MBLs producing strains are detected in the laboratory?
Ans: The gold standard is the detection of MBL producing gene by molecular
techniques. However this is not practical and cost effective for most of the
laboratories in Pakistan. Therefore phenotypic methods have been developed
including
Double-disc synergy tests (DDSTs)
Using a ceftazidime disc and a 2-mercaptopropionic acid (MPA)
disc
Imipenem disc and an EDTA disc
Double Etest (Imipenem on one side and Imipenem+EDTA on other
side
Although different phenotypic methods have been described, the CLSI (along
with other international committees) currently does not include standardized
recommendations for MBL screening. However organisms that appear to be
carbapenem susceptible on antimicrobial susceptibility testing but that have
phenotypic or genotypic evidence of production of carbapenemases should be
regarded as nonsusceptible to all carbapenems.
Copyright @ Antimicrobial Resistance Network 2008, All right reserved
Q- What should be done to prevent spread of these strains in the
hospitals?
Identify high-risk colonized patients (especially international
medical transfers
or those sharing a room with persons who are known to be
colonized or
infected) by use of rectal swabs plated onto selective media
Perform molecular epidemiologic analysis of strains recovered from
infected or
colonized patients
Institute contact isolation precautions for all patients infected or
colonized with
carbapenem-resistant or carbapenemase-producing organisms
Enhance hand hygiene
Enhance environmental cleaning
Copyright @ Antimicrobial Resistance Network 2008, All right reserved
Copyright @ Antimicrobial Resistance Network 2008, All right reserved