Call for Evidence Response
advertisement

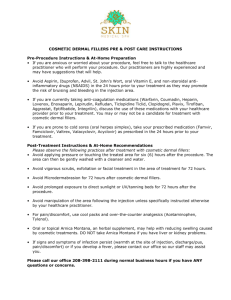
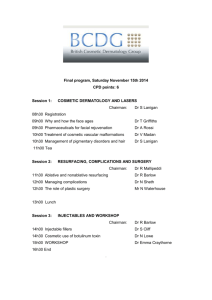
Dr Chris Jones Dirprwy Brif Swyddog Meddygol Deputy Chief Medical Officer Y Gyfarwyddiaeth Feddygol Yr Adran Iechyd, Gwasanaethau Cymdeithasol a Phlant Department for Health, Social Services and Children Date: 15 October 2012 Professor Sir Bruce Keogh Medical Director NHS England Department of Health Richmond House 79 Whitehall London SW1A 2NS Dear Bruce Review of the Regulation of Cosmetic Interventions: Call for Evidence Thank you for the opportunity to comment on the Department of Health’s “Call for Evidence” relating to the Review of the Regulation of Cosmetic Interventions. Please find below the Welsh Government’s formal response. The regulation and safety of products used in cosmetic interventions We hold the view that materials injected into the human body for non-medical purposes should be subject to the same regulation as pharmaceutical products with detailed prospective trials to establish the likely tissue response and any adverse reactions before approval for use is granted. It is noteworthy that in the USA there is a requirement for FDA approval and the number of approved dermal fillers is much smaller. These views are applicable to both temporary and permanent filling materials. The proposal in the EU regulatory advice that injectable fillers should be included in the planned implant database is welcomed. We believe that it is essential that users of dermal fillers should be able to recognise and treat complications that arise from their use. There is merit in this being under the direct supervision of a medical qualified practitioner. Parc Cathays ● Cathays Park Caerdydd ● Cardiff CF10 3NQ Ffon/Tel: 029 2082 3505 Ffacs/Fax: 029 2082 3982 Ebost/Email:chris.jones@wales.gsi.gov.uk How best to ensure that the people who carry out procedures have the necessary skills and qualifications The practice of cosmetic surgery can be demanding both in terms of surgical technique, but as importantly in decision making and judgement. In any other branch of surgery this would be expected to require a significant period of supervised training (this is best achieved by the completion of a specialist surgical fellowship exam before a period of sub-specialist training in cosmetic practice). Any practitioner should hold registration with the GMC on a relevant specialist register. It would not be appropriate for a member registered as an ENT surgeon to carry out cosmetic breast or abdominal surgery but it would be appropriate for a member of that register, suitably trained to carry out facial aesthetic surgery. A requirement for an approved period of cosmetic surgery training, before admitting rights to independent hospitals were granted (or employment in independent clinics was offered), might help ensure that appropriately trained practitioners were carrying out these procedures. Accreditation of such training by a royal surgical college or speciality association(s) would have merit and create consumer confidence. We do not support the establishment of a new specialty of cosmetic surgery – this would not be necessary and might attract people away from the core surgical specialities where they should remain. There is important shared learning and technique between cosmetic and reconstructive surgery practice. The current arrangement where non-UK trained surgeons with no UK validation of surgical competence and only basic medical qualifications can practice independently in cosmetic surgery would appal members of the public if understood and should be brought to a halt as a priority. With regard to cosmetic treatments, we have significant concerns about the variable quality and lack of training of practitioners carrying out these treatments such as fillers, laser treatments, chemical peels and Botox. There is a worrying array of “new” and “novel” treatments being offered to the public. Short (often single day) courses run by the manufacturers of these treatments and products are not adequate in our view to ensure validated competence. Establishing a licence to practice using such materials with a requirement to maintain high quality records of outcomes and adverse events related to them would be a significant step forward in improving safety and surveillance for these products. How to ensure that organisations have the systems in place to look after their patients both during their treatment and afterwards Independent hospitals and clinics as well as non healthcare establishments should operate to the same standards as the NHS in this regard. There should be careful and detailed clinical audit by all practitioners, supported by the organisation as a pre-requisite for continued practice for any cosmetic practitioner. There should also be clear and explicit arrangements for how patients/clients can access support after treatment if problems arise. No-one should be undertaking treatments or procedures if they cannot deal with the complications themselves or do not have an explicit arrangement with someone who can. Again this could form part of the requirements for a licence to practice for cosmetic practitioners and for hospitals and clinics. Everyone should have a statutory right to access their full health or beauty records with reasonable notice. Some form of ABTA style bond might help patients where businesses go bankrupt. This would need to offer cover for a period of 2 years after treatment during which the majority of problems come to light. The re-establishment of a national implant registry would be a very important component of aftercare for relevant patients. The proposal from the Australian Society of Plastic Surgeons for a common dataset internationally has merit given the global nature of cosmetic surgery. How to ensure that people considering cosmetic surgery and procedures are given the information, advice and time for reflection to make an informed choice We support the recommendations of best practice for obtaining consent in cosmetic surgery, such as those published by BAPRAS and BAAPS. We believe that such an approach should be universal and could form part of the requirements for revalidation for cosmetic practice. The idea of a two-stage process with a “cooling off” period for elective cosmetic procedures is also supported and is extremely common already amongst plastic surgeons. It should be required across all practitioners (including tattooists). We do not believe that the universal referral of all cosmetic surgery patients for psychological assessment is either required or proportionate. Through their training, plastic surgeons become familiar with normal and abnormal responses to appearance and welcome the support of suitably trained psychologists (who are not widely available, in any event) for patients with evidence of dysmorphophobia or other abnormal patterns of behaviour. We strongly deprecate financial incentives such as “buy one get one free”, non-refundable deposits and discounts for quick decisions which trivialise the seriousness of cosmetic surgery and reduce the opportunity for reflective decision making by patients. There is much high quality information available from professional organisations including BAPRAS. We support anything that encourages patients to seek out such information from accredited sources and to use it to support their discussions with practitioners. What improvements are needed in dealing with complaints so they are listened to and acted upon As indicated above the keeping of good records, with easy access by the client/patient is an important component of this. The principles of redress adopted within the NHS should be considered in independent practice/establishments. Clearly published information on how to make a complaint and get help is also important. These arrangements should be reviewed when establishments are inspected. Non-UK based practitioners working in the UK must be subject to equally robust arrangements. A mandatory implant registry would allow the sharing of knowledge of problems relating to implants across the sector more effectively. Regulatory role of Healthcare Inspectorate Wales Under the present regulatory regime in Wales, cosmetic surgery carried out within the independent healthcare sector is covered by the Care Standards Act 2000 and the associated Private and Voluntary Health Care Regulations. In our view these are adequate in providing a regulatory framework that addresses the issues and questions set out in Section 3 of the DH consultation. For example: ensuring that the people who carry out procedures have the necessary skills and qualifications and appraisals are carried out; organisations have the systems in place to look after their patients both during their treatment and afterwards; organisations have policies and procedures in place so that people considering cosmetic surgery and procedures are given the information, advice and time for reflection to make an informed choice; organisations have written complaints procedure that are publically available; organisations carry out clinical audit programmes; and premises are safe and fit for purpose. The same is true of the use of class 3B or 4 lasers and intense pulsed light for cosmetic purposes. I must emphasise that Wales, unlike England, has kept the providers of these interventions within regulation. The present regulatory framework in Wales allows Healthcare Inspectorate Wales (HIW) to exercise flexibility in terms of its inspection approach so that it is proportionate to the risk posed by such interventions but at the same time provides an adequate level of assurance about the safety and quality of the services provided. With regard to the providers of other cosmetic procedures such as dermal fillers or peels, these are not regulated at present in Wales. However, there are organisations and individuals who provide a range of non-surgical cosmetic interventions; some of which are regulated and some of which are not. There is also the added complication that it is potentially the case that a provider of cosmetic interventions operating across the Wales/England border will be subject to two different regulatory requirements. The mixed economy of regulation by HIW (and possibly Local Authorities) and self regulation is potentially confusing to the public (and providers) and each offers a different level of objective assurance about the quality and safety of the services being provided. Although non-surgical cosmetic interventions are generally low risk in terms of harm, in our view it would make more sense for them all to be regulated in a consistent way. This would both provide the public with a level of assurance about the safety of those organisations and also be easier for providers to comply with. The current regulatory framework for the independent healthcare sector in Wales can allow for a flexible, proportionate approach and, even if the regulations needed amendment to accommodate new ‘listed’ procedures or a simplifying of the regulations for these procedures and providers, this would not be difficult to achieve. The NHS in Wales is not subject to a regulatory regime as exists in England but it is required to demonstrate that all health services are provided and delivered in a way that is compliant with a range of policies and standards, not least the Welsh Government’s Standards for Health Services. General comments We have also been involved recently in the Medicines and Healthcare products Regulatory Agency discussions about the review of Medical Device (MHRA) legislation in Europe. We are therefore aware that there are proposals to cover a subset of cosmetic devices (which will be in the form of a list), specifically those which are implantable or invasive devices without a medical purpose. The list at present seems reasonable, as it includes contact lenses for cosmetic reasons, fillers and lasers for hair removal. We consider this will bring substantial benefit to the quality of the devices in this sub-set, which have previously been outside the regulatory control of the MHRA. In particular, it will bring these devices into the incident reporting system which will make it mandatory for 'vigilance' reporting by the manufacturers when they become aware of adverse incidents. Yours sincerely DR CHRIS JONES Dirprwy Brif Swyddog Meddygol Deputy Chief Medical Officer