use of amoxycillin + clavulanic acid combination in veterinary
advertisement

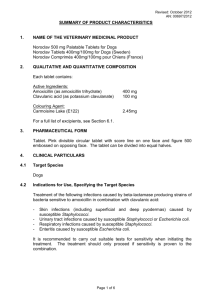
ISRAEL JOURNAL OF VETERINARY MEDICINE REVIEW: USE OF AMOXYCILLIN + CLAVULANIC ACID COMBINATION IN VETERINARY MEDICINE Vol. 57 (2) 2002 AND POSSIBLE ANTIBIOTIC RESISTANCE OF HUMAN PATHOGENS: S. P. Pozzi1 and Z. Ben-David2 1. Pfizer AHG, Ussishkin 56/2, 94541 Jerusalem; 2. Vet-Magen Ltd, POB 76, 60910 Bney-Zyion, Abstract Amoxycillin and clavulanic acid combination is used in veterinary medicine since 1980 for treating livestock and companion animals. Different presentations are in use: injectable, intra-mammary, oral tablets and bolus and oral drops. Doubts have arisen concerning the possibility of antibiotic resistance occurrence in bacteria of animal origin and possible transfer of resistance to human pathogens. A retrospective and worldwide investigation failed to reveal the occurrence of decreased susceptibility of human pathogens to amoxycillin and clavulanic acid Introduction ß-lactamines are the bactericidal antibiotics inhibiting the formation of the bacterial cell wall by interfering with final stage of peptido-glycan synthesis. Bacteria in growing phase cannot complete cell wall structure, thus the cell wall is compromised and bacteria die. Gram positive (G+) and negative (G-) bacteria have walls constructed in different way, so far showing higher or lower affinity to different classes of ß-lactamines. Resistance to ß-lactamines, may be linked either to lack of receptors on the cell wall for specific ß-lactamine (as in G-) or to the production of enzymes inactivating ß-lactamines (both types of bacteria). These enzymes, the ß-lactamases, are produced by bacteria and reversed outside the bacteria in extracellular space (G+) or in peri-plasmatic space of bacteria (G-). When ß-lactamase enzymes interact with ß-lactamines, they bind to each other. The binding causes opening of ß-lactamines structure and loss of their bactericidal activity, as illustrated in Figure 1. ß-lactamase plasmid-mediated is responsible for the rapid spread and diffusion of resistance in bacterial populations and results in the significant reduction of activity of aminopenicillins because of ability to transfer the gene encoding the mechanism of antibiotic resistance to other bacteria (2a). Chromosome-induced resistance is less important because of slow and gradual appearance and changes mainly linked with bacteria cell structure, and are not inducible (2b). Clavulanic acid produced by Streptomyces clavuligenus, has a chemical structure similar to some ßlactamines, e.g. penicillin. When clavulanic acid is present in extra-cellular space of bacteria it competitively binds with (2b) and inactivates ß-lactamases belonging to PCI class. Thus, bacteria become sensitive again to ß-lactamine (5). Clavulanic acid, with sulbactam (2a,b) and tazobactam (3), belong to a group of at least three substances with ß-lactamase inhibition activity. Slight differences with respect to pharmacology, potency and activity, are considered of little therapeutic significance (3). Clavulanic acid has good affinity for ß-lactamases plasmid-mediated and chromosome-induced, while it has a low affinity for chromosome induced cephalosporinases (2a). In veterinary medicine, a combination of amoxicillin + clavulanic acid (amoxi-clav) was designed in 1980 to overcome resistance to amoxycillin-mediated by ß-lactamases, produced by bacteria of relevant veterinary interest; among these, in particular Staphylococcus species. The mechanism of action of clavulanic acid is to form an irreversible link with ß- lactamase (2a, 4). Clavulanic acid prevents ß-lactamase inhibiting bactericidal activity of ß-lactamines (4). Because of its irreversible link and inactivation of ß-lactamases, clavulanic acid is able to make ß-lactamaseproducing bacteria sensitive again to a large number of penicillin and cephalosporin -class antibiotics (2a) Figure 1: mechanism of action of ß-lactamase enzymes According to Richmond and Sykes (1, modified) there are 5 classes of ß-lactamase enzymes: 1. Chromosome induced: Cephalosporinase by P. aeruginosa; C. freundii; acting on cephalosporin as substrate 2. chromosome induced and plasmid mediated (DNA transduction) - PCI by S. aureus; acting on penicillin as substrate 3. 3 plasmidium-mediated: - TEM 1, 2; SHV-1; Rob-1; CTX-1; CTZ-1; by Enterobacteriacee - PSE-1; Carb-3; by E.coli; P. aeruginosa - OXAI —7 by Enterobacteriacee Figure 2: mechanism of action of clavulanic acid In veterinary medicine, this kind of irreversible link has not been demonstrated as affected by appearance of resistance to clavulanic Acid (2b) Clavulanic acid is extremely active: concentrations of 0,01 to 0,08 mcg/ml inactivates 50% of ßlactamases, released by S. aureus MB9, E.coli K12R tem, P. mirabilis, K. aerogenes A (reference laboratory strains), which would inactivate more than 40 mcg/ml of susceptible ß-lactamines (5). In other words, concentration of 1mcg/ml of calvulanic acid is enough to “protect” 500 to 4000mcg/ml of ß-lactamine sensitive to ß-lactamases. Therefore, pharmacological preparations containing amoxyclav at ratio 4:1 or 2:1, as in human preparations, fully ensure the quantity of clavulanic acid necessary to inactivate all ß-lactamases responsible for ß-lactamine inactivation. Use of “amoxi-clav” complex in veterinary medicine Combination of amoxi-clav specifically designed for veterinary use is established in several countries since mid 1980s, as summarized in Table 1. Veterinary preparations contain amoxi-clav at a ratio of 4:1, while human preparations contains amoxy-clav at up to a 2:1 ratio, that means two-fold clavulanic concentration in respect to veterinary preparations. Use of specific veterinary preparations, instead of off-label use of human preparations, could be of utmost importance in the very rare and theoretical case in which any bacteria from animal origin and of human relevance, would loose susceptibility to amoxi-clav because of a lower concentration of clavulanic acid in respect to ßlactamase produced. The amoxi-clav combination is considered “useful” per os administration in monogastric; and intra-muscular (i.m.) administration in animal food producers, in particular for infections of the lower respiratory tract in bovine, due to Actinobacillus, Haemophilus and by Pasteurella ß-lactamase producers (2). Table 1: Number of countries, type of formulation and year of introduction of amoxi-clav association designed for veterinary use (6). Formulation Species Cattle Swine Sheep Dogs Cats Injectable X X X X X Intramammary X Bolus X Tablets X X X No. of Countries Year of introduction 38 1987 46 1986 18 1984 49 1984 Despite several years of regular use in veterinary practice the significant appearance of antibioticresistance, neither in companion animals nor livestock, have been documented. In dogs and cats, data on antibiotic resistance patterns among staphylococcal diseases (S. aureus; S. intermedius) have been collected at The Royal Veterinary College, London over the past 15 years. The authors comment on the “failure to demonstrate resistance to amoxy-clav” and that “ S. intermedius does not readily develop resistance to this substance” (7). Out of 78 recent (1995 - 2000) canine isolates of B. bronchiseptica from 13 separate sources in UK, all were sensitive to amoxy-clav, 13 years following its introduction (8). A total of 318 pyoderma isolates (S. aureus131; S. intermedius 187) from dogs in France have been tested for antimicrobial susceptibility during 1986 - 1996. The authors report “more than 95%” were susceptible to amoxy-clav (9). In food-producing animals, formulations of amoxi-clav are used for short-term (a few days) treatment in acute infections. There is no indication for long-term therapy, by any route. This shorttime use in individual animals (there is no formulation suitable for group/mass treatment) is particularly unlikely to select for resistance, since repeated and long-term therapy is not involved. In swine, data on 1969 bacterial strains of P. multocida; A. pleuropneumoniae; H. parasuis; S. suis; E. coli; Salmonella species, tested in Italy, during 1995-2000 did not demonstrate development of resistance to amoxi-clav; In comparison to a progressive pattern of microbial resistance to many antimicrobial agents, especially by P. multocida and A. pleuropneumoniae (10). The Swedish Veterinary Antimicrobial Resistance Monitoring quotes 3 cases out of 260 of amoxyclav resistance in pigs; 0 out of 293 in cattle; 5 out of 274 in chickens (11). Furthermore “the association amoxi-clav is already quoted as “registered for use in bovine” (2). The use in cattle is also supported by Soback (12). The efficacy of amoxi-clav in treatment of common respiratory diseases caused by Pasteurella (Mannheimia) haemolytica has been widely confirmed by practical experience in the field. Relative to intra-mammary administration, 484 S. aureus isolates from the bovine mammary gland have been isolated in 1999 and 2000 in Italy and tested, among others, against amoxy-clav. Their susceptibility was 99,6% in 1999 and 100% in 2000 (13). Cases of antibiotic-resistance by some Gram-negative bacteria - P. aeruginosa; Serratia; E. coli JT 414 must be related to an intrinsic mechanism of resistance, because of production of a different type of ß-lactamase and not due to a decrease of activity of Clavulanic acid on these bacteria (2a, 5). Amoxy-clav is not recommended for use in horses because of occurrence of diarrheal disease (2b). In countries in which amoxi-clav is used in veterinary practice, is there an increase in resistance to amoxy-clav in pathogens of human relevance? There is a general lack of data to show that use of antibiotics in animals has a significant impact on resistance in humans. This is particularly true where G +, non-zoonotic bacteria (the usual target of the use of amoxy-clav) are concerned. A retrospective study to 1990, summarized up in Table 2, quotes more than 50 studies (14 to 55) relative to ß-lactamines - Clavulanic acid activity in human medicine in the period 1985-2001 in countries in which veterinary preparations of amoxy-clav are used. Table 2: Summary of studies relative to ß-lactamines— clavulanic acid activity in human medicine between 1985-2001 (Ref. 14 - 55). No. of Countries No. of isolates Type and no. of studies Resistance or MIC* Pharmacolo- Clinical observations Susceptibility 17 >32000 31 gical models 7 8 No. of patients No. of clinics >1100 40 *Minimal Inhibiting Concentration The review did not reveal any significant change in susceptibility of pathogens of human relevance to ß-lactamines - Clavulanic Acid. There are no evidences of generalized decrease in susceptibility of examined pathogens (14, 16, 24, 25, 27-29, 31, 33, 35, 39-45, 52, 53) and no increase of relative MICs (46, 47, 49, 55). Cases of reduced sensibility to ß lactamine- Clavulanic acid are mainly associated with G- bacteria, in particular S. enterica serotype Typhimurium, (18); Salmonella and Shigella strains (32); E.coli (34; 36; 37); H. influenzae (50). Apparently reduced sensibility is due to TEM-1 ß-lactamase hyper-producing isolates (36) or high level of ß-lactamine hydrolysis rather than to the Clavulanic Acid resistance properties (18). On the other hand, ß-lactamine- Clavulanic acid presents the lowest resistance level in E. coli (37) while implementation of guidelines for antibiotics use (38, 39) was followed by increase of susceptibility of E. coli (39). In a previous wider study (42), which includes over 1500 publications over 15 years, no evidence for any significant increase in resistance to amoxy-clav was demonstrated. With this past experience, it appears highly improbable that the use of amoxi-clav in animals will have any influence whatsoever on the susceptibility of human pathogens. Any concerns regarding resistance in humans would best directed at its use in human patients (38, 39). Conclusions There is no evidence, either from in vitro or laboratory studies or veterinary clinical practice, of the appearance of antibiotic resistance to Clavulanic acid. Indeed, the term “antibiotic resistance” may be considered not fully appropriate. Clavulanic acid does not act on bacteria direct, rather on ß-lactamase, while the real bactericidal activity is mediated by the antibiotic associated with clavulanic acid, either amoxicillin or ticarcillin (2b). Clavulanic acid may induce ß-lactamase production in ß-lactamine susceptible Enterobacter and Providencia, nevertheless resistance to clavulanic acid has not yet been described in practice (2b). There are no authors reporting contra-indications for its use in companion animals or food producing animal because of fear of antibiotic-resistance increase. On the contrary, the association amoxy-clav is largely and extensively recommended and registered in many countries, including the USA and the European Union, The combination amoxy-clav is also approved and used in several countries with different administration routes: p.o.; i.m; sub cutaneous (s.c.); i.ma. for milk-producing cows and sheep. Widespread use of veterinary preparations over a period of many years has shown no sign of compromising the sensitivity of human pathogens to the action of ß-lactamines by clavulanic acid. Moreover, the activity of the combination has been maintained despite vast numbers of humans receiving ß-lactamines - clavulanic acid therapy, both in hospitals and in the community. This widespread use in man gives rise to the conditions where resistance might be anticipated - yet it has remained notably rare (42). In parallel, about 50 publications, in countries in which veterinary amoxi-clav is used, do not quote significant changes in antimicrobial resistance of ß-lactamines - Clavulanic acid toward a wide range of human pathogens. LINKS TO OTHER ARTICLES IN THIS ISSUE References 1. Richmond, M.H. and Sykes, R.: The beta-lactamase of Gram- bacteria and their possible role. Adv. Microb. Physiol. 9; 3, 1973. 2. a) Prescott, J., Baggot, D., Antimicrobial Therapy in Vet.Med. ch. 8; 143-158. Italian Ed on 2nd USA Ed. 1996. b) Prescott, J., Baggot, D., Antimicrobial Therapy in Vet.Med. ch. 3; 25-42. Italian Ed on 2nd USA Ed. 19963. 3. Katzung, B. G.: Basic & Clinical paharmacology. Ch. 43; 754-773; 2000. 4. Booth, N. and McDonald, L.: Veterinary Pharmacology and Therapeutics. ch. 49; 874-902. Italian Ed. on 6th USA Ed. 1991. 5. Cole, M.: Clavul.-potentiated amoxicillin mechanism of action against penicillin resistant bacteria., BVA Congress Proc., UK; 1991. 6. Pfizer, A.H.G.: Synulox: Regulatory data on file; 2001. 7. Lloyd, D.: Sensitivity to antibiotics amongst cutaneous and mucosal isolates of canine pathogenic staphylococci in the UK, 1980 - 1996. Vet. Dermatol. 7; 171, 1996. 8. Speakman, A., Dawson, S., Corkill, J., Binns, S., Hart C. and Gaskell, R.: Antibiotic susceptibility of canine B. bronchiseptica isolates. Vet. Microbiol. 71(3-4); 193, 2000. 9. Pellerin, J., Bourdeau, P., Sebbag, H. and Person J.: Epidemiosurveillance of antimicrobial compound resistance of S. intermedium clinical isolates from canine pyodermas. Comp. Immun. Microbiol. Infect. Dis. 21(2); 115, 1998. 10. Barigazzi G.: In vitro susceptibility of bacteria from pigs to various antibacterial agents in Italy 19942000. XXVII SIPAS proc., 295, 2001. 11. Swedish Veterinary Antimicrobial Resistance Monitoring, Bengsson & Walfen Ed., SVA, Uppsala, Sweden, 24, 2000. 12. Soback, S.: Clav.potentiated amoxycilline: in vitro antibacterial activity and oral bioavailability in calves. J. Vet. Pharmacol. Ther. 10; 105, 1987. 13. Carnevali, N. and Nocetti, M.: Antimicrobial susceptibility of S. aureus strains isolated from bovine milk during five years. XXXIII SIB proc. 131, 2001. 14. Vanhoof, R., Carpentier, M., Glupczynsky, Y., Gordts, B., Magerman, K., Mans, Y., Nyssen, H., Simon, A., Surmont, I., V.d. Vyevere, M., V.Landuyt, H., Nimmen, L., V.Noyen, R.: Surveillance of pneumococcal resistance in Belgium during winter 1996-1997. Acta Clin. Belg. 53(4); 275, 1998. 15. Yourassowsky, E., V.d. Linden, M., MacGilavry, G. and Glucpczynsky, Y.: Is there in Belgium an increase in resistance to the combination amoxiclav of E.coli as reference bacteria? Acta Clin. Belg. 47(1); 15, 1992. 16. Vanhoof, R., Carpenter, M., Delannoy, P., Fagnart, O., Lontie, M., Mans, I. and V.Nimmen L.: Study of the in vitro activity of amoxiclav and other beta-lactam antibiotics against E. coli isolated urine specimens. Acta Clin. Belg. 56(1); 32, 2001. 17. Tremblay, L., L’Ecuyer, J., Provencher, P. and Bergeron, M.: Susceptibility of H. influenzae to antimicrobial agents used in Canada. Canadian Study Group. C.M.A.J. 143(9); 895, 1990. 18. Leflon-Guibout, V., Speldooren, V., Heym, B. and Nicholas-Chanoine, M.: Epidemiological survey of amoxiclav resistance and corresponding molecular mechanisms in E. coli isolates in France: new genetic features of bla (TEM) genes. Antimicr. Ag. Chemot. 44(10); 2709, 2000. 19. Poirel, L., Guibert, M., Bellais, S., Naas, T. and Nordmann, P.: Integron and carbenicillinase mediated reduced susceptibility to amoxiclav in isolates of multidrug resistant S.enterica serotype typhimurium DT104 from French patients. Antimicr. Agen. Chemot. 43(5); 1098, 1999. 20. Madinier, I., Fosse, T., Hitzig, C., Charbit, Y. and Hannoun, L.; Resistance profile survey of 50 periodontal strains of A.actinomyectomcomitans. J. Periodont. 80(8); 888, 1999. 21. Weber, P., Plaisance, J. and Mancy, C.: Comparative epidemiology of the resistance of enterobacteriaceae, Staphylococcus and Pseudomonas aeruginosa to floroquinolones in an outpatient study. Presse med. 24(21); 979, 1995. 22. Carsenti-Etesse, H., Durant, J., DeSalvador, F., Bensoussan, M., Bensoussan, F., Pradier, C., Bernard, E., Mondain, V., Thabaut, A. and Dellamonica, P.: Possible prevention of an in vitro selection of resistant S. pneumoniae by beta lactamase inhibitor. Eur. J. Clin. Microbiol. 13(12); 1058, 1994. 23. Defouilloy, C., Fremaux, A., Mehdaoui, A., Geslin, P. and Bignon, J.; Resistance of S. pneumoniae to penicillin. Bacteriological resistance/clinical resistance. Pathol. Biol. 42(5); 475, 1994. 24. Ruckdeschel, G.: Respiratory tract infections: how frequent is antibiotic resistance? In vitro activity of older and recent antibiotics against the significant pathogens. Forts. Med. 112(33); 485, 1994. 25. Sugita, R., Komatsu, N., Deguchi, K., Naito, M., Yoshida, Y., Watanabe, H., Senba, T., Harada, S., Fukamoto, K. and Fujimaki, Y.: A clinicobacteriologic study on amoxiclav in pediatric sinusitis. Jpn. J. Antib. 52(10); 613, 1999. 26. Sugita, R., Harada, S., Deguchi, K., Fujimaki, Y., Naito, M., Komatsu, N., Nomura, T., Okano, K., Tanaka, M., Shimizu, K., Watanabe, H., Kimura, S., Yoshida, Y., Senba, T. and Uchida, T.: A clinicobacteriological study on amoxiclav in pediatric acute otitis media. Jpn. J. Antib. 52(10); 595, 1999. 27. Esposito, S., DeRitis, G., D’Errico, G., Noviello, S. and Ianniello, F.: Clinical comparison of cefaclor bid versus amoxiclav or erythromicin three times daily in the treatment of patients with streptococcal pharyngitis. Clin. Ther. 20(1); 72, 1998. 28. Zanchi, A., Mencarelli, M., Sansoni, A., Rossolini, A. and Cellesi, C.: Antibiotic susceptibility of 206 H. influenzae isolates collected from children in central Italy. Eur. J. Epid. 10(6); 699, 1994. 29. Henderson, G., Garner, J. and Morris, A.: Antimicrobial susceptibility of anaerobic bacteria in Auckland 1987-90. NZ Med. J. 105(926): 11, 1992. 30. Janicka, G., Wojcechowska, D., Harenska, K., Porada, J. and Klyszejko, C.: The resistance to betalactam antibiotics of lactose+ and lactose- stains of E. coli. m, Acta Microbiol. Pol. 46(4); 399, 1997. 31. Trucco, O., Prado, V., Garreaud, C. and Paya, E.: Antimicrobial activity of amoxicillin versus amoxiclav. In vitro study against S. aureus, H. influenzae and A. baumanii strains. Rev. Med. Chil. 121(8); 916, 1993. 32. Miro, E., Mirelis, B., Navarro, F. and Prats, G.: Detection of resistance to the amoxiclav combination in Salmonella and Shigella. Enf. Infec. Microbiol. Clin. 14(1); 31, 1996. 33. Prieto, J., Aguilar, L., Gimenez, M., Toro, D., Gomez-Lus, M., DalRe, R. and Balcabao, I.: In vitro activities of amoxiclav at concentrations achieved in human serum against the resistant subpopulation of heteroresistant S. aureus: a controlled study with vancomycin., Antimicrob.Agen.Chemot.42(7); 1574, 1998. 34. Garcia - Rodriguez, J.: Bacteriological comparison of cefixime in patients with noncomplicated urinary tract infection in spain. Preliminary results. Chemot. Act. 1; 28, 1998. 35. Paniagua, G., Monroy, E., Garcia, O. and Vaca, S.: Effect of betalactamase inhibitors on MIC of ampicillin and amoxicillin for S. aureus strains. Rev. Latinoam. Microbiol. 40(3-4); 128, 1998. 36. Oliver, A., Perez-Vazquez, M., Martinez-Ferrer, M., Baquero, F., DeRafael, L. and Canton, R.: Ampicillin-sulbactam and amoxiclav susceptibility testing of E. coli isolates with different betalactam resistance phenotypes. Antimic. Agen. Chemot. 43(4); 862, 1999. 37. Kahlmeter, G.: The ECO-SENS Project: a prospective, multinational, multicentric epidemiological survey of the prevalence and antimicrobial susceptibility of UTI — interim report. J. Antimicrob. Chemot. 46; 15, 2000. 38. Verzasconi, R., Rodoni, P., Monotti, R., Marone, C. and Mombelli, G.: Amoxiclav versus amoxicillin plus gentamicin in the empirical initial treatment of UTI in hospitalized patients. Schweiz. Med. W’sch. 125(33); 1533, 1995. 39. Natsch, S., Conrad, C., Hartmeier, C. and Schmid, B.: Use of amoxiclav and resistance in E. coli over a 4 year period. Infect. Contol. Hosp. Epidemiol. 19(9); 653, 1998. 40. Cokca, F. and Altay, G.; Development of resistance in bacteria interacting with sub inhibitory antibiotic concentrations. Mikrobiol. Bul. 26(4); 333, 1992. 41. Seetulsingh, P., Hall, L. and Livermore, D.: Activity of clavulanate combinations against TEM-1 beta lactamase producing E. coli isolates obtained in 1982 and 1989., J. Antimicrob. Chemot. 27(6); 749, 1991. 42. Rolinson, G.: A review of the microbiology of amoxiclav over the 15 year period 1978-1993. J. Chemot. 6(5); 283, 1994. 43. Simpson, I., Durodie, J., Knott, S., Shea, B., Wilson, J. and Machka, K.: Effects of following National Committee for Clinical Laboratory Standards and Deutsche Industrie Norm-Medizinische guidelines, country of isolate origin and site of infection on susceptibility of E. coli to amoxiclav (Augmentin)., J. Clin. Microbiol. 36(5); 1361, 1998. 44. Felmingham, D., Robbins, M., Tesfaslasie, Y., Harding, I., Shrimpton, S. and Grunenberg, R.: Antimicrobial susceptibility of community-acquired lower respiratory tract bacterial pathogens isolated in the UK during the 1995-1996 cold season. J. Microbiol. Chemot. 41(3); 411, 1998. 45. Barrett, S., Savage, M., Rebec, M., Guyot, A., Andrews, N. and Shrimpton, S.: Antibiotic sensitivity of bacteria associated with community-acquired UTI infection in Britain. J. Antimicrob. Chemot. 44; 359, 1999. 46. Singh, K., Reves, R., Pickering, L. and Murray, B.: Comparative in vitro activities of Amoxiclav, cefuroxime, cephalexine and cephalotin against trimethoprim-resistant E. coli isolated from stools of children attending day-care centers. Antimicrob. Agen. Chemoter. 34(11); 2047, 1990. 47. Appelbaum, P., Spangler, S., Shiman, R. and Jacobs, M.: Susceptibilities of 540 anaerobic G- bacilli to amoxicillin, amoxicillin BRL 42715, amoxiclav, temafloxacin and clindamycin. Antimicrob. Agen. Chemot. 36(5); 1140, 1992. 48. Powers, R.: Open trial of oral fleroxacin versus amoxiclav in the treatment of infections of skin and soft tissue. Am. J. Med. 94(3A); 155, 1993. 49. Spangler, S., Jacobs, M. and Appelbaum, P.: In vitro susceptibility of 185 penicillin-susceptibile and resistant pneumococci to WY-49605, a new oral penem, compared with those to penicillin G, amoxicillin, amoxiclav, cefixime, cefaclor, cefpodoxime, cefuroxime and cefdinir. Antimcorb. Agen. Chemot. 38(12); 2902, 1994. 50. Doern, G., Brueggemann, A., Pierce, G., Holley, H. and Rauch, A.: Antibiotic resistance among clinical isolates of H influenzae in the USA in 1994 and 1995 and detection of betalactamase positive strains resistant to amoxiclav: results of a national multicenter surveillance study. Antimicr .Agen. Chemot. 41(2); 292, 1997. 51. Jacobs, M. and Bjaksouzian, S.: Evaluation of H influenzae isolates with elevated MOCs to amoxiclav. Diagn. Microb. Infect. Dis. 28(3); 105, 1997. 52. Thornsberry, C., Ogilvie, P., Kahn, J. and Mauriz, Y.:Surveillance of antimicrobial resistance in S pneumoniae, H influeanzae and M. catarrhalis in the USA in 1996-1997 respiratory season. Diagn. Microbiol. Infect. Dis. 29(4); 249, 1997. 53. Jacobs, M., Dagan, R., Appelbaum, P. and Burch, D.: Prevalence of antimicrobial resistant pathogens in middle ear fluid: multinational study in 917 children with acute otitis. Antimicrob. Agen. Chemot. 42(3); 589, 1998. 54. Davies, T., Pankuch, G., Dewasse, B., Jacobs, M. and Appelbaum, P.: In vitro development of resistance to five quinolones and amoxiclav in S pneumoniae. Antimicrob. Agen. Chemot. 43(5); 1177, 1999. 55. Butler, D., Gangnon, R., Miller, L., Poupard, J., Felmingham, D. and Grueneberg, R.: Differences between the activity of penicillin, amoxicillin, and amoxiclav against 5252 S pneumoniae isolates tested in the Alexander Project 1992-1996. J. Antimicrob. Chemot. 43(6); 777, 1999. LINKS TO OTHER ARTICLES IN THIS ISSUE 1.