April 4, 2014 - Transplant Pro
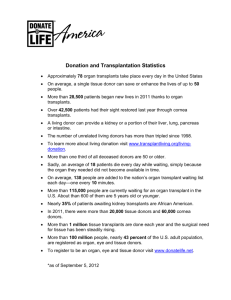
advertisement

AGENDA Region 8 Meeting Kansas City Airport Hilton Kansas City, MO April 4, 2014 8:30 Registration and Continental Breakfast 9:00 Welcome/Opening Remarks 9:15 Harvey Solomon, MD Region 8 Councillor Fall 2013 Regional meeting summary Committee nominations Fall 2014 meeting date Non-Discussion agenda process OPTN/UNOS Update (30 minutes) Kenneth Andreoni, MD OPTN/UNOS President 9:45 OPTN/UNOS Committee Reports and Voting on Public Comment Proposals Moderator: Harvey Solomon, MD Transplant Coordinator Committee Andrew Webb, RN, BSN Proposal to Notify Patients Having an Extended Inactive Status (10 minutes) The goal of this proposal is to promote effective and safe care for organ candidates by increasing awareness of their inactive waiting list status. Published literature suggest that the longer candidates wait for an organ while in an inactive status, the less likely they are to receive a transplant. In addition, the Committee is concerned that candidates are not consistently informed of their status nor do they understand what it means to have an inactive status. Thoracic Transplantation Committee Scott Silvestry, MD Committee Update (5 minutes) Proposal to Continue the Adolescent Classification Exception for Pediatric Lung Candidates (10 minutes) On June 10, 2013, the OPTN/UNOS Executive Committee approved a temporary policy permitting lung candidates less than 12 years old to request an exception from the Lung Review Board (LRB) to be classified as an adolescent candidate for the purposes of prioritization by lung allocation score (LAS) for lung offers from donors 12 years of age and older. Unless further action is taken by the Board of Directors, the “adolescent classification exception” will expire on July 1, 2014. Because the temporary policy permits young pediatric lung candidates who may be suitable for lung offers from larger donors to apply for an exception, the Thoracic Committee proposes removing the July 1, 2014, deadline from the policy making this a permanent policy change. The Thoracic Committee also proposes additional language to clarify the data reporting requirements for candidates with approved adolescent classification exceptions. Operations and Safety Committee Committee Update (5 minutes) Nancy Long, RN, BA, CCTC Proposed ABO Blood Type Determination, Reporting, and Verification Policy Modifications (15 minutes) Member feedback has long noted the complex phrasing and requirements related to ABO blood type determination and verification. These requirements are a fundamental step in safe and successful organ transplantation. The Committee is proposing clarifications and improvements to these requirements. These recommendations are based, in part, from a Failure Modes and Effects Analysis (FMEA) conducted to proactively identify areas of risk related to ABO processes in deceased donation. This policy proposal is only one facet in the Committee’s approach to improving ABO blood type determination and verification. Other strategies to minimize identified risks and maximize human factors engineering include member education and competency training, programming changes to UNet℠, and collaboration with the Electronic Tracking and Transport (ETT) project to improve technological capabilities. This policy proposal contains the following features: Clarified existing requirements related to commonly asked questions Strengthened safety components to ensure the correct organ is transplanted into the correct recipient and that the match is ABO compatible or intended incompatible Modified the timing of deceased donor blood type determinations and reports prior to executing the match run with an exception for accelerated donor cases Modified the timing and scope of verifications for deceased and living donor organ recoveries Clarified specific verification elements and sources Better aligned OPTN and Centers for Medicare and Medicaid Services (CMS) requirements Added conditional requirements to check in organs upon arrival and to perform a pre-transplant verification Added a requirement for qualified health care professionals to perform ABO reporting and verification functions Made deceased and living donor standards more consistent Membership and Professional Standards Committee Christie Thomas, MB, FRCP, FASN, FAHA Committee Update (5 minutes) Proposal to Allow a MPSC Recommendation to the Board of Directors for Approval Consideration of a Non Qualifying Transplant Program Applicant Located in a Prescribed Geographically Isolated Area (10 minutes) The proposed bylaw language makes available a mechanism by which the MPSC may make a recommendation to the Board, and the Board may consider and approve the designation of transplant programs who currently cannot meet key personnel qualifying criteria because the applicant is located in a geographically isolated area. Currently, if an applicant cannot meet the program requirements, then the application is closed by the MPSC as rejected, leaving the applicant to appeal to the HHS Secretary for any further approval consideration of the closed application. Living Donor Committee Krista Lentine, MD, PhD Proposal to Modify Existing or Establish New Requirements for the Informed Consent of all Living Donors (10 minutes) This proposal would modify existing policy and establish new policy requirements for the informed consent of all living donors. This proposal is in response to a directive from the Health Resources and Services Administration (HRSA) to develop such policy, and is based on recommendations from a Joint Societies Steering Committee composed of representatives of the American Society of Transplantation (AST); the American Society of Transplant Surgeons (ASTS) and the North American Transplant Coordinators Organization (NATCO) to the Living Donor Committee. Policy to standardize the informed consent of living kidney donors has already been established. This proposal would modify some elements of exiting policy for the informed consent of living kidney donors and establish new requirements for all other categories of living organ donors. Proposal to Modify Existing or Establish New Requirements for the Psychosocial and Medical Evaluation of all Living Donors (10 minutes) This proposal would modify existing policy and establish new policy requirements for the psychosocial and medical evaluation of all types of living donors. This proposal is in response to a directive from the Health Resources and Services Administration (HRSA) to develop such policy, and is based on recommendations from a Joint Societies Steering Committee composed of representatives of the American Society of Transplantation (AST); the American Society of Transplant Surgeons (ASTS) and the North American Transplant Coordinators Organization (NATCO) to the Living Donor Committee. Policy to standardize the medical evaluation of living kidney donors has already been established. This proposal would modify some elements of existing policy for the psychosocial and medical evaluation of living kidney donors and establish new requirements for the psychosocial and medical evaluation for all living organ donors. Kidney Transplantation Committee Clifford Miles, MD Committee Update (10 minutes) Kidney Paired Donation (KPD) Histocompatibility Testing Policies (15 minutes) This proposal includes requirements for histocompatibility testing on donors and recipients in the OPTN KPD Program. It includes required methods for HLA typing, antibody screenings, and crossmatching; a list of HLA types that must be reported for donors and candidates; and processes that must be followed for identifying unacceptable antigens and in the event of unacceptable positive crossmatches. Histocompatibility Committee Brian Freed, PhD, D(ABHI) Committee Update (5 minutes) Expanding Candidate and Deceased Donor HLA Typing Requirements to Provide Greater Consistency Across Organ Types (15 minutes) The proposed changes make the HLA typing methods and list of HLA loci to be reported consistent for deceased donors across all organ types. The required methods and list of HLA loci to be reported will apply both when OPTN policy requires HLA typing be performed and reported on the deceased donor prior to allocation (i.e. for kidney, kidney-pancreas, and pancreas allocation) and in instances where HLA typing is required only if requested by the candidate’s transplant program (i.e. for heart, heart-lung, and lung allocation). The proposal includes new requirements for reporting HLA-DQA and HLA–DPB for deceased donors. The time period for reporting deceased donor HLA typing remains different by organ type to meet varying clinical requirements for timing of transplants. The proposal newly requires HLA typing to be performed and reported for deceased liver donors if requested by a transplant program and makes HLA typing requirements for deceased pancreas islet donors and candidates consistent with those for deceased pancreas donors and candidates. Pediatric Transplantation Committee Update (10 minutes) Richard Hendrickson, MD 12:00 Lunch (provided) **There will be a breakout during lunch for liver programs to meet and discuss regional and national liver issues** Ad Hoc Disease Transmission Advisory Committee Scott Biggins, MD Proposal to Align OPTN Policies with the 2013 PHS Guideline for Reducing Transmission of Human Immunodeficiency Virus (HIV), Hepatitis B Virus (HBV), and Hepatitis C Virus (HCV) Through Solid Organ Transplantation. (15 minutes) The Final Rule §121.4 (OPTN policies: Secretarial review and appeals.) notes that the OPTN Board of Directors is responsible for developing policies that are consistent with recommendations of the Centers for Disease Control and Prevention (CDC) to test potential organ donors and following transplant recipients to prevent the spread of infectious disease. The June 19, 2013, release of the PHS Guideline for Reducing Human Immunodeficiency Virus (HIV), Hepatitis B Virus (HBV), and Hepatitis C Virus (HCV) Through Organ Transplantation led to a systematic review of related OPTN policies. This proposal seeks to modify some existing policy language and also create new policies to reflect recommendations outlined in this updated PHS document. Liver and Intestinal Transplantation Committee Ruben Quiros, MD Committee Update (15 minutes) Proposal to Cap the HCC Exception Score at 34 (15 minutes) Candidates with a MELD/PELD score exception for HCC receive high priority on the liver waiting list, especially as their exception scores may increase automatically every three months. Increasingly, there are candidates with multiple HCC exception extensions who are now receiving regional offers under the “Share 35 Regional” policy implemented in June 2013. These candidates are likely to have a much lower risk of disease progression or dropout (i.e., removal from the waiting list for death or being too sick) than candidates with calculated MELD/PELD scores of 35 and higher. This proposal would cap the HCC exception score at 34, in effect giving candidates with calculated MELD/PELD scores of 35 and higher a better opportunity to receive regional offers under the new policy. Proposal to Delay HCC Exception Score Assignment (15 minutes) Candidates with a MELD/PELD score exception for HCC receive high priority on the liver waiting list, especially as their exception scores may increase automatically every three months. These candidates have significantly lower dropout rates (i.e., removal from the waiting list for death or for reasons related to the HCC) than non-HCC candidates, with the exception of those areas of the country with lengthy waiting times. The proposed solution to address the disparities in drop-out rates between patients with HCC exceptions and those without is to delay the score assignment by 6-months. Simulation modeling has shown that this would equalize the transplant and dropout rates for those with and without HCC exceptions. In areas of the country with shorter waiting times to transplant, the delay will also allow a window of time for centers to observe candidates with rapidly growing tumors who may have very poor outcomes with a transplant. At least one study indicates that candidates with HCC exceptions in regions with shorter waiting times to transplant, where this “biologic test” is not met due to rapid transplantation, have worse post-transplant outcomes. Proposed Membership and Personnel Requirements for Intestine Transplant Programs (in collaboration with the Membership and Professional Standards Committee) (15 minutes) The proposed bylaw will define a designated intestine transplant program and establish minimum qualifications for primary intestine transplant surgeons and physicians. The proposal includes a full approval pathway and a conditional approval pathway to obtain the requisite experience to perform primary surgical and medical care. The intent is to set minimum standards where none currently exist without compromising quality or restricting new program formation. Minority Affairs Committee Update (5 minutes) Christie Gooden, MD Pancreas Transplantation Committee Update (5 minutes) Zoe Stewart, MD, PhD Patient Affairs Committee Update (5 minutes) Corrie Wright, MS Transplant Administrators Committee Update (5 minutes) Katie Evers, RN, BSN, MBA Non-Discussion Agenda Harvey Solomon, MD (5 minutes) ** As a reminder, these items require a vote but will not be presented or discussed** Proposal to Require the Collection of Serum Lipase for Pancreas Donors (Pancreas Transplantation Committee) This document proposes to make serum lipase a required field in Policy 2.8.E Required Information for Deceased Pancreas Donors, as well as required in DonorNet®, in order to make electronic pancreas offers. Currently, serum lipase is a listed field in DonorNet®, but is not required in order to make electronic pancreas offers. Serum lipase level(s) in deceased donors are reliable indicators of pancreas function and quality. As such, the serum lipase values assist in making an informed clinical decisions regarding electronic pancreas offers. The proposal also proposes to create a new field in DonorNet ® where OPOs will report the upper limit of normal (i.e. maximum normal value or highest reference value) of the laboratory’s normal serum lipase reference range. The reason for programming this new field is because laboratories’ measurement ranges vary for serum lipase. As a result, a serum lipase value may have two different meanings at two different laboratories. This results in varying “normal” serum lipase values across the country. This new field will provide a reference point regarding the serum lipase value to the physician making the decision whether to accept the pancreas. Proposal to Require the Reporting of Aborted Living Donor Organ Recovery Procedures (Living Donor Committee) Promoting patient safety is a critical component of the OPTN’s mission. The OPTN seeks to protect the safety of transplant candidates, recipients, and living donors, but living donors are unique in that they put themselves at risk without any potential benefit to their own health. Due to a variety of reasons, including last minute recipient or donor health problems and unforeseen donor anatomy issues, living donor organ recovery procedures occasionally need to be aborted after anesthesia has been administered, but before the recovery of the organ. Monitoring the safety of these prospective donors is an important part of the OPTN’s goal of promoting living donor safety. The OPTN relies on the UNetSM Improving Patient Safety Portal for notification of patient safety concerns and living donor adverse events. Under this proposal, an aborted living donor organ recovery procedure would become a new category of living donor adverse event that recovery hospitals would need to report through the UNetSM Improving Patient Safety Portal. Additionally, the proposal would clarify current living donor adverse event reporting requirements by eliminating some redundant sections of policy. Proposal to Clarify Data Submission and Documentation Requirements (Membership and Professional Standards Committee (Membership and Professional Standards Committee) Policy 18.1 (Data Submission Requirements) requires members to submit data to the OPTN through the use of standardized forms. However, Policy 18.1 does not explicitly state that the data submissions must be accurate or that members must be able to provide documentation to verify the accuracy of their data submissions. The MPSC historically has agreed that the need for accurate data is implied within Policy 18.1, as is the member’s obligation to provide documentation to verify the data’s accuracy. This proposal’s goal is to amend Policy 18.1 to explicitly state that the data must be accurate and that members must provide documentation to support their data. Proposed ABO Subtyping Consistency Policy Modifications (Operations and Safety Committee) This proposal seeks to make all ABO subtype references consistent throughout OPTN policies. Current references use different terms, such as A2 and non-A1, which are intended to mean the same thing but may be confusing. The more technically accurate description uses the “non” preface as routine testing only detects the presence or absence of A1 and other rare subtypes other than A2 do exist. In 2011, the OPTN published guidance on this issue. The proposed changes will align references with this guidance using the terms blood type A, non-A1 and blood type AB, non-A1B. Proposal to Allow Non-substantive Changes to the OPTN Policies and Bylaws (Policy Oversight Committee) On occasion, clerical errors are identified in the Policies and Bylaws. These clerical errors are non-controversial things like obvious misspellings and mis-numbering of lists. There is nothing in the Bylaws or Policies that allow staff to make these non-substantive changes. This proposal would allow staff to make non-substantive changes without needing approval by the Executive Committee or Board of Directors. The Executive Committee would review these changes retrospectively. 3:30 Adjournment