service specification for psychiatric liaison service
advertisement

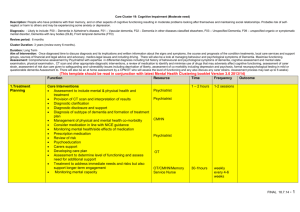
Service specification for dementia: mental health liaison service for general and community hospitals DH INFORMATION READER BOX Policy HR / Workforce Management Planning / Performance Clinical Estates Commissioning IM & T Finance Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 16035 Title Dementia Commissioning Pack Author DH Publication Date 21 Jul 2011 Target Audience PCT CEs, SHA CEs, Local Authority CEs, Directors of Adult SSs, GPs Circulation List #VALUE! Description Commissioning Packs are tools to help commissioners improve the quality of services and minimise unwarranted variation in service delivery. Each Pack provides a tailored set of guidance, templates, tools and information to assist commissioners in commissioning services from existing providers or for use in new procurements. Cross Ref Superseded Docs Action Required N/A N/A N/A Timing N/A Contact Details Gill Ayling Quarry House Leeds West Yorkshire LS2 7UE 0113 25 46359 www.dh.gov.uk For Recipient's Use Dementia Commissioning Pack Handbook Commissioning Framework & Assessment Tool 2. Care at home / care home 3. Care in hospital 5. Patient information 4. Cost / benefit tool 3. Specification 2. Action Plan / Inserts 1. Case for change 1. Early diagnosis Procurement templates and guidance 4. Antipsychotic medication Contents A. B. Key service outcomes Purpose of the service B1 National and local context B2 Note for commissioners B3 Aims and objectives Scope C. C1 Patients C2 Target groups C3 Equity of access to services C4 Geographical coverage/boundaries C5 Requests for support C6 Interdependencies with other services C7 Location of service C8 Days/hours of operation Service delivery D. Stage 0 – Organisational and service level prerequisites Stage 1 – Assessment and diagnosis Stage 2 – Supporting good clinical care Stage 3 – Discharge support Indicators E. Dashboard F. Activity G. G1 Activity plan G2 Individual patient agreements (cost per case) Finance H. Annex 1: Service accountabilities 4 5 5 8 9 11 11 11 11 11 12 12 12 12 13 14 21 29 34 38 40 41 41 41 42 43 User note This specification has been designed to assist commissioners in the delivery of a service to support general and community hospitals to deliver better care to people with dementia. The text within square brackets [ ] in this document should be completed by the commissioner in order to reflect local needs and help inform responses from the Provider(s). The specification should be read in conjunction with the ‘Action plan to improve care for people with dementia in hospital’ as the mental health liaison service is designed to be one of the priorities in the action plan to support training and organisational development objectives. The specification is not mandatory and the commissioner should review the whole of the specification in order to ensure that it meets local needs and, once agreed with the Provider, it should form part of either a renegotiated contract or the relevant section of the NHS Standard Contract. The Dementia Commissioning Pack should be used in conjunction with: Call to Action: Reducing inappropriate use of antipsychotics for people with dementia Together with the Dementia Action Alliance, the NHS Institute for Innovation and Improvement has launched a Call to Action to work together in a way that will unite us in our common cause to improve the quality of life of people with dementia and their carers by reducing the inappropriate use of antipsychotics. To find out more and access resources which will support this Call to Action please visit: www.institute.nhs.uk/qipp/calls_to_action/dementia_and_antipsychotic_drugs or you can email C2ADementia@institute.nhs.uk 3 A. Key service outcomes Expected high-level outcomes of the service are: No. Outcome 1 Reduction in the average length of stay in hospital for patients with dementia 2 Reduction in the number of people with dementia discharged directly from hospital to care homes as a new place of residence 3 Increase in the number of patients with dementia and their carers who have a positive experience of hospital care 4 Reduction in the number of people discharged from hospital on antipsychotic medication and increase in the number of people having a plan to review use of antipsychotic medication post discharge Guidance on measuring outcomes is provided in Section E. 4 Related NICE Quality Standard NHS Outcome Framework 1,3,4,8 2,4 B. Purpose of the service B.1 National and local context Up to 70% of hospital beds are currently occupied by older people1 and up to half of these may be people with cognitive impairment, including those with dementia and delirium.2 In too many cases, mental health needs will remain undetected and a mental health assessment will not be made, with the result, in some cases, that appropriate treatment is not initiated.3 The National Audit Office found that some general hospital services even worked hard not to make a diagnosis of dementia for fear it would delay discharge.4 Failure to diagnose dementia is an independent predictor of a poor outcome for the patient and for the service. People with dementia often have complex problems and may stay in hospital for longer than other people who go in for the same condition. There is often a lack of co-ordination between the hospital and care providers at the point of discharge. The longer length of stay may worsen symptoms of dementia and be detrimental to the individual’s well-being. Discharge to a long-term residential care home becomes more likely and antipsychotic drugs are more likely to be prescribed.5 Although there are examples of good quality general hospital care, where the challenges of dementia are recognised and addressed, there are also widely reported cases of substandard or neglectful care.6 1 Audit Commission (2006), Living Well in Later Life: A review of progress against the National Service Framework for Older People. 2 Royal College of Psychiatrists (2005), Who Cares Wins: Improving the outcome for older people admitted to the general hospital. 3 Arden M et al, Cognitive impairment in the elderly medically ill: how often is it missed? International Journal of Geriatric Psychiatry, 1993; 8: 929–937. 4 National Audit Office (2007), Improving services and support for people with dementia. London: TSO. 5 Alzheimer’s Society (2009), Counting the Cost: Caring for people with dementia on hospital wards. London: Alzheimer’s Society. 6 Age Concern (2006), Hungry to be Heard. London: Age Concern. 5 Better management of mental health problems has major implications for the quality of care of people, the efficiency of general and community hospitals and the efficient utilisation of health and social care resources. When established, specifically commissioned services to improve the care of older people with mental health problems in hospital not only improve the quality of care but also have the potential to release savings:7 A hospital mental health liaison service for older people in Leeds contributed to a reduction in hospital length of stay of four days per admission for people with dementia. The National Audit Office estimates the excess cost of inappropriate care in an average general hospital to be around £6 million per year. The National Dementia Strategy (2009) states improved care in general hospitals as one of its objectives8 and specialist liaison services are advocated both in the National Dementia Strategy and in the National Institute for Health and clinical Excellence (NICE)/Social Care Institute for Excellence (SCIE) guideline on dementia.9 The service to be commissioned in this specification is a service to support general and community hospitals to deliver better care for people with dementia and will: support and advise on making the diagnosis of dementia and other mental health conditions. This includes providing a second opinion in cases of diagnostic doubt support and advise on management and care planning, including discharge planning for people with confirmed or suspected mental health problems. This includes requests for urgent attention or response to patient behavioural management difficulties to support hospital clinicians and provide a link to community services, including specialist dementia services where appropriate contribute to mental health education and training for hospital staff 7 National Audit Office (2007), Improving services and support for people with dementia. London: TSO. 8 Department of Health (2009), Living well with dementia: A National Dementia Strategy. London: TSO. 9 National Institute for Health and Clinical Excellence/Social Care Institute for Excellence (2006), Dementia: Supporting people with dementia and their carers in health and Social Care. 6 contribute to the governance, audit and development of policies and procedures for good quality mental health care. Local context [The commissioner should insert relevant information on local factors that influence the way the Provider delivers the service, e.g. issues linked with: Joint Strategic Needs Assessments (JSNA), Health and Well-being Boards’ Strategic Plans demographics epidemiology the organisations commissioning the services – and any other existing services.] 7 B.2 Note for commissioners The aim of the mental health liaison service is to provide expert mental health skills to support good quality care of patients in parts of the hospital where these skills are not already available. The responsibility for providing good quality care remains with ward staff. In some parts of the hospital, where good skills already exist, input may be low, be mainly advisory in nature and relate to more complex cases only. Where mental health skills do not exist in sufficient quantity, part of the initial function of the service may be to provide more direct support to ward staff where required and to help establish procedures, protocols, governance and audit arrangements for good quality mental health care. The service will contribute to training and education to meet skills gaps in provision so that staff become competent to deal with routine cases. As a result of these interventions, over time the nature of the support service may change to become increasingly an advisory service for more complex mental health cases. This is shown in the diagram below: Higher level of service maturity and mental health skills Commencement of service Low level of service maturity and mental health skills Time More routine liaison work More complex liaison work Assessment and diagnosis Management and care planning Discharge support Intervention is characterised more in terms of direct support and modelling of good care for ward staff Support service is characterised much more as an advisory service for more complex cases as protocols are embedded and ward staff become competent to handle routine cases Contribute to training and education and protocols, governance and audit 8 B.3 Aims and objectives The aim of the mental health liaison service is to advise on the diagnosis of people with suspected organic and functional mental health problems and to provide expert advice and support on the delivery of good clinical care, care planning and discharge planning, as required. The service shall develop the competencies of existing staff to deliver good quality mental health care and care of people with dementia and shall assist in putting in place procedures, protocols, governance and audit arrangements to support the delivery of good mental health care and the care of people with dementia. In so doing, the service shall support the efficient use of existing resources to improve standards of care. The objectives of the service are: Support and advice on assessment and diagnosis To advise and support high-quality accurate diagnosis of dementia and other mental health problems. This may mean providing advice or support in more complex cases or more routine cases as required. Support and advice on care planning, optimum care and response to behaviours that challenge To provide timely advice and support to staff to manage behaviours that challenge during the designated hours of the service as requested, and only after ward staff have followed the local protocol as appropriate and in line with NICE Clinical Guideline 103 (delirium). This includes providing urgent response advice to emergency departments and acute medical admissions units on cases where non-hospital management options might be possible. To provide advice on care planning and delivery of optimum care and to advise ward staff, patients and carers in making decisions about timely discharge and appropriate place of discharge, resulting in fewer people waiting for community discharge plans to be put in place or waiting for residential or care-home placements. This includes advice on options for support in the community, intermediate care, reablement and referral to local dementia services in order to promote early discharge opportunities. 9 Advice on other available specialist support To provide links and sharing of information with other resources that can support independent living and well-being for patients with mental health needs and their carers, including GPs, community mental health services, specialist dementia services, social care, intermediate care and memory services. Contribute to training and organisational development To provide knowledge transfer to ward staff, improving their competences and confidence in dealing with patients with organic and functional mental health needs with the result that the patients’ symptoms are less likely to deteriorate and become problematic. Where a protocol for the management of behaviours that challenge or a capacity framework do not exist, or are not being followed, to help ward staff to develop and implement them and to contribute to putting in place governance and audit arrangements. To support education and training on good clinical care for patients with mental health problems, particularly dementia, in order to promote a dignified and person-centred experience for the individual and their carer, which minimises distress and ensures that the patient is discharged without losing more functionality. 10 C. Scope C.1 Patients The mental health liaison service is designed for patients with symptoms of organic and functional mental health problems. The heterogeneity of symptoms prior to diagnosis will mean that the service shall provide advice and support for patients with a range of mental health needs including depression, delirium and/or dementia. The service shall also be accessible to people with learning disabilities. The majority of patients who are in contact with the mental health liaison service will be elderly and a significant proportion of these will have dementia or some other cognitive impairment. A Provider shall ensure that sufficient resources and skills are in place to meet the specific needs of this target group. C.2 Target groups It is not the role of the support service to carry out the functions of ward staff; the role of the service is to provide additional support and advice on diagnosis, care planning, good clinical care and discharge support. This means, for example, that ward staff should follow established pathways or protocols that relate to good mental health care prior to contacting the support service. C.3 Equity of access to services [Describe the Provider’s required policy and practices for ensuring that its services are accessible to all, regardless of age, disability, gender reassignment, pregnancy and maternity, race, religion or belief, sex or sexual orientation, and deal sensitively with all service users and potential service users and their family/friends and advocates. Explain policies and practices to actively engage with, and provide culturally sensitive services to, minority groups in the population served] C.4 Geographical coverage/boundaries [Include details of any required geographic coverage/boundaries or geographical restrictions.] 11 C.5 Requests for support The Provider shall accept requests from all parts of the hospital C.6 Interdependencies with other services [Describe any relationships between the service and other Providers of health, social care and other services in which a relationship of ‘dependency’ exists. The commissioner should consider any other existing relevant services, which may include, for example: existing support arrangements in A&E; on-call arrangements for out of hours services; services for adults; services for people with learning disabilities; and intermediate care services. The commissioner should discuss governance arrangements for the support service with the Provider, including the inter-relationship with the management of the NHS trust and reporting requirements.] C.7 Location of service [The service should be located in the general hospital with the greatest need – where a commissioner would like alternative arrangements, they should describe them here.] C.8 Days/hours of operation [Include full details of times at which the Provider offers services.] 12 D. Service delivery The following diagram sets out a pathway for a mental health liaison service. It shows four stages in the pathway and certain elements may take place in parallel rather than in series. Not all patients will require all components of the service (1–3). Stages 1 to 3 reflect the delivery of the commissioned service. Stage 0 is included in the service specification to confirm the obligations to be placed on the Stage 0 Provider by the commissioner. This is important because Stage 0 reflects the prerequisites that should be in place for Stages 1 to 3 to be effective. The Provider shall contribute to establishing procedures, protocols, governance and audit arrangements and education and training where needed in order to support good quality mental health liaison services and promote the efficient use of existing resources – although overall responsibility for this remains with the hospital NHS trust. A high-level service description is set out below. Service level 1 Advice on assessment and diagnosis Patient presentation 0 Confirm patient eligibility & contact support service 2 Advice on good clinical care 3 Patient discharged Advice on discharge Provider identifying and contacting wards where advice / support / training may be required Organisational level Assistance in establishing procedures, protocols, governance and audit arrangements Assistance in delivering education and training to support good quality mental health care 13 Stage 0 – Organisational and service level prerequisites Service level prerequisites Patient 0.1 Confirm patient eligibility 0.2 0.3 Contact the support service Share information about the service Patient presents at hospital Provider identifying and contacting wards where advice / support / training may be required Organisational level prerequisites Assistance in establishing procedures, protocols, governance and audit arrangements Assistance in delivering education and training to support good quality mental health care 14 Request for advice or support from support service Overview Stage 0 describes the prerequisites that should be in place for the mental health liaison service to be effective. Prerequisites need to be in place at an organisational level and a service level. Organisational level In order to use mental health liaison service resources efficiently and to improve capability of staff across the hospital, the NHS trust shall be responsible for putting in place procedures, protocols, governance and audit arrangements at ward level to support the delivery of good quality mental health care. The NHS trust shall also have responsibility for developing and delivering staff education and training to meet the mental health needs of patients. The mental health liaison service shall assist in the development and delivery of these objectives but shall not be responsible for them. Service level Support or advice may be requested from health professionals in relation to: assessment and diagnosis of a suspected mental health problem good health and social care for patients with a mental health problem, including care planning or discharge planning. This may include urgent response or advice on managing behaviours that challenge Staff should follow appropriate mental health procedures or protocols, prior to contacting the support service. Although the service is primarily request led, the Provider shall also have responsibility for identifying and contacting parts of the hospital where advice and support may be needed and also have responsibility for identifying training requirements and escalating issues to the Executive Board where performance fails to improve within a reasonable time period. 15 Indicators Outcomes There is no specific indicator for Stage 0 This stage contributes to: Outcomes 1 – 4 The text below describes the infrastructure that needs to be in place at an organisational level in order to help ensure that a mental health liaison service is effective: Establishing procedures, protocols, governance and audit arrangements The NHS trust shall ensure that procedures, protocols, governance and audit arrangements are put in place across the hospital to enable staff to respond more effectively to patients with mental health problems and to help ensure that resources from the mental health liaison service are used efficiently. Where procedures and protocols do not already exist, the Provider shall assist in establishing them to support the delivery of good quality mental health care. These procedures and protocols shall include, but not be limited to: managing behaviour that challenges, in line with NICE guidelines on delirium and dementia assessing capacity within the Mental Capacity Act (2005) deprivation of liberty safeguards dementia-friendly care pathways appropriate use of antipsychotic medication for people with dementia. The Provider shall support the development of governance arrangements for the implementation and review of these procedures and shall support the implementation of audit arrangements in relation to the Royal College of Psychiatrists National Audit of Dementia Care (core audit and the enhanced audit). Although the mental health liaison service shall support the development and implementation of these actions, the overall responsibility for delivery remains with the Trust. 16 Education and training to support good quality mental health care The scale of resources available in the mental health liaison service and the scale and profile of the training challenge will mean that the Provider cannot be responsible for the delivery of all education and training to support good quality mental health care. The Trust shall be responsible for ensuring that a strategy is in place, together with sufficient resources and management supervision to deliver education and training, and the Provider shall assist in training and education as required, in relation to: establishing protocols and procedures for good mental health care training and education requirements arising from routine support requests from hospital wards or as a result of feedback from the National Audit of Dementia, other surveys or from patients and carers. Education and support should enable ward staff to handle the vast majority of routine issues relating to mental health care and over time the mental health liaison service should provide an advisory service rather than direct support. [The commissioner should note that dementia training for hospital staff may be delivered through the ‘Action plan for improved care in hospital’ which should be considered with this specification.] The text below describes the process that needs to be in place at a service level to help ensure that the support service is effective: 17 0.1 Confirm patient eligibility Hospital staff shall consider contacting the mental health liaison service for any adult where there is uncertainty about diagnosis or treatment for a mental health problem, including dementia. Because of the complexity and heterogeneity of symptoms, it is not possible to provide an exhaustive list of eligibility criteria. Instead, the request for advice or support is a clinical decision based on the possibility or knowledge that the individual has dementia or other mental health problems and expert mental health support or advice is required. This will be on the basis of presenting symptoms, a review of past history or collateral history from an informant. A request to the support service may relate to: a request for advice or support for assessment and formal diagnosis where there is uncertainty of diagnosis a request for advice in relation to care planning or addressing care needs or discharge planning advice where the patient has a diagnosed or suspected mental health problem and where staff are uncertain about the best treatment. This may include requests for urgent support or response to managing patients’ behaviours that challenge. Hospital staff shall identify patients that meet the criteria for advice or support from the mental health liaison service. Eligible patients are those who meet the general criteria set out below. Hospital staff may contact the mental health liaison service by telephone to check whether further advice or support is required. 18 Inclusion criteria The patient is presenting with symptoms of suspected mental health needs and advice on diagnosis is required. The patient has a diagnosis of mental health need and advice is required in relation to care planning, meeting good clinical care standards or discharge planning. Urgent support or response to patient behavioural management difficulties is required in cases with a known or suspected mental health need. Exclusion criteria It is not the role of the mental health liaison service to carry out the functions of ward staff nor to duplicate existing skilled provision; the role of the mental health liaison service is to provide advice and support on diagnosis, care planning, good clinical care and discharge planning. This means, for example, that ward staff should follow established protocols or procedures relating to mental health care prior to contacting the support service. 0.2 Contact the support service Hospital-based health professionals shall make contact with the service by secure email, telephone, fax or IT system, following standard arrangements that are in place in the hospital. The Provider shall respond within [one] working day of the request being made. Where a request is made for urgent attention, the Provider shall prioritise this request and respond within [one] hour. 19 0.3 Share information about the service Hospital-based health professionals shall, where relevant and where possible: provide information to the patient and carer about the service advise the patient that the support service may need to speak to the patient and another point of contact (e.g. family carer, person who resides with the patient or another person who has frequent contact with the patient) ask permission from the patient to speak to another point of contact. If the patient lacks capacity, contact a family carer or other appropriate person in line with the requirements of the Mental Capacity Act (2005). 20 Stage 1 – Assessment and diagnosis Advice and/or support 1.3 History taking Patient Patient continues to assessment 1.1 Receive request and confirm eligible patients 1.2 Initial review of presenting symptoms 1.4 1.7 1.6 Cognitive & mental state examination 1.5 Other appropriate investigations 21 Make the diagnosis Communicate the diagnosis Advise on good clinical care [2] Overview At this stage, the Provider shall deliver advice to ward staff on assessment, diagnosis and/or sharing the diagnosis. For more complex cases, or cases where there is uncertainty, the Provider upon request shall provide direct support in undertaking assessment, diagnosis and/or sharing the diagnosis. Where the initial indicators are those of delirium or other mental health need, the Provider shall follow the relevant NICE guidelines on assessment, diagnosis and treatment. The Provider shall: provide advice or support for more complex cases where there is diagnostic uncertainty or provide advice where a second opinion is requested. A diagnosis of dementia shall only be made after a comprehensive assessment by a suitably qualified professional, including, where appropriate (NICE/SCIE Clinical Guideline 42): history taking cognitive and mental state examination physical examination as needed and other appropriate investigations a review of medication. As required, the Provider shall see the patient within [one] working day of receiving the request and shall complete the diagnosis within [five] working days. Indicators Outcomes Indicator 1 This stage contributes to: There will be a reduction in average length of stay in hospital for people with dementia of [x] days Outcome 1. There will be a reduction in average length of stay in hospital for people with dementia 22 1.1 Receive request and confirm eligible patients The Provider shall check the request and confirm eligible patients within [one] working day of receiving it and shall confirm a date and time to provide advice or support. The Provider shall respond to all requests relating to adults with suspected mental health problems. The Provider shall accept or reject the request for advice or support based on a telephone query or based on information provided in the hospital’s standard service request arrangements. In some instances, advice may be provided by telephone. 1.2 Initial review of presenting symptoms The Provider shall provide advice or support on the initial review of presenting symptoms. Advice or support on the initial review shall be by a suitably qualified and trained professional who is able to determine whether presenting symptoms or indicators are likely to be those of dementia or another mental health problem such as delirium. Where the presenting symptoms or indicators are those of another mental health need other than dementia, the Provider shall follow the appropriate NICE guidelines on assessment, diagnosis and treatment. Where dementia is suspected and where further advice or support is requested, the Provider shall follow the process and timelines set out below. If the initial review indicates that an assessment should take place in the community, this recommendation shall be made to the patient’s GP. This action may be appropriate in instances where the patient is likely to be discharged before the diagnosis is complete or where there are other complicating factors, such as delirium, that mean a diagnosis is not likely to be possible until a later follow-up meeting. The numbers of recommendations to GPs for community assessments shall be recorded and shared with the commissioner. 23 1.3 History taking At the date and time agreed with the person who has made the request, the Provider shall advise on or undertake the assessment with the patient. History taking shall be undertaken by a suitably qualified and trained professional and shall include, but shall not be limited to: a subjective and objective assessment of patient’s life, social, family and carer history, circumstances and preferences, as well as their physical and mental health needs and current level of functioning and abilities, including an interview with an informant to generate a collateral history assessment of history and impacts of impairments of vision, hearing and mobility assessment of history and impacts of impairments of medical co-morbidities assessment of key psychiatric and behavioural features, including depression, wandering and psychosis risk assessment covering all areas appropriate to the individual, e.g. falls, risk to self, childcare or carer responsibilities, driving, and financial and legal issues carer assessment including stress, health and function. In undertaking the assessment, specialist input may be required from geriatricians or specialists in stroke or falls, or a wide range of other disciplines including specialist nurses, therapists, pharmacists and social workers. Appropriate quality assurance shall be in place, including appropriate supervision and quality control. The Provider shall note NICE/SCIE Clinical Guideline 42 and confirm whether the patient wishes to know the outcome of the diagnosis and with whom the diagnosis should be shared. The Provider shall also explain the process and timelines for making and communicating the diagnosis. 24 1.4 Cognitive and mental state examination The Provider shall advise on or undertake a cognitive and mental state examination. The cognitive and mental state examination shall be undertaken by a professional with specialist expertise in diagnosis and sub-typing and shall include an examination of attention and concentration, orientation, short and long-term memory, praxis, language and executive function. The Provider shall be qualified to undertake and interpret formal detailed cognitive testing using standardised instruments. However, in undertaking these tests, the Provider shall also have experience of taking in to account other factors known to affect performance (educational level, skills, prior level of functioning and attainment, language and any sensory impairments, psychiatric illness or physical/neurological problems). 1.5 Other appropriate investigations The Provider may need to advise on or arrange further investigations to inform diagnosis or sub-typing and these shall include, but not be limited to: review of medication in order to identify and minimise the use of drugs that may adversely affect cognitive functioning. This should be a shared responsibility with physicians ECG/EEG structural imaging (magnetic resonance imaging, MRI or computer tomography) formal neuropsychological testing where appropriate other investigations as appropriate. Where there is a high likelihood that the patient will be discharged before investigations are complete, the Provider shall inform the patient and, if appropriate, the carer that the patient’s GP will contact them to let them know the outcome of the investigations. The Provider shall forward results from investigations to the patient’s GP, together with recommendations for future care. 25 1.6 Make the diagnosis A diagnosis of dementia and its sub-type shall be made by health care professionals with expertise in differential diagnosis of dementia using international standardised criteria in line with NICE/SCIE Clinical Guideline 42. 1.7 Communicate the diagnosis Wherever possible, the Provider shall contact the carer within [two] working days of the diagnosis having been made in order to organise a time to communicate the diagnosis to the patient and the carer together, although in some instances the diagnosis may need to be shared separately with a carer, for example by telephone. The Provider shall note the importance of a carer being present wherever possible to provide support to the patient when the diagnosis is communicated. The Provider shall follow NICE/SCIE guidelines on sharing information with patients and their families. The Provider shall also ensure that relevant hospital health care professionals are informed of the diagnosis before it is shared with the patient or carer because this should inform their care planning and discharge planning. Where the patient has been discharged before the Provider is able to share the outcome of the diagnosis, the Provider shall contact the patient’s GP to request that they contact the patient and carer to communicate the diagnosis in person. The GP may choose to make a referral to the memory service or community mental health team to provide specialist advice and support. The Provider shall share the diagnosis with the patient’s GP and where appropriate provide recommendations on further means of support, such as the memory service, mental health services or specialist dementia services. The Provider shall communicate the diagnosis to the patient and carer in simple, direct language avoiding use of medical jargon and shall communicate in a warm, caring and respectful manner. Diagnoses and actions fall in to five categories: 26 Diagnosis Action 1. No organic or functional mental health problem Communicated to requesting clinician and GP 2. Other mental illness (including depression or delirium) Advice communicated to requesting clinician including the initiation of urgent treatment or referral to other services – GP informed 3. Dementia (no medication) Talk through support available via local support organisations or via the community mental health team if needed – GP informed 4. Dementia (medication) Talk through available medication and support available via local support organisations and arrange follow-up by community mental health team if needed – GP informed 5. Possible dementia Communicated to requesting clinician and GP with advice to refer to memory service, if available, if symptoms persist or increase 1. No organic or functional mental health problem Where the diagnosis is one of no organic or functional mental health problem, the patient and the requesting clinician shall be notified of this outcome and this information shall be shared with the patient’s GP. 2. Other mental illness (including depression or delirium) The Provider shall share the diagnosis with the patient and requesting clinician and where appropriate the Provider shall advise on the initiation of urgent treatment or referral for physical or mental disorder if required. The Provider shall give the requesting clinician advice on further treatment needed and shall share this information with the patient’s GP. 27 3. Dementia (no medication) The Provider shall inform the requesting clinician and give a clear and full explanation to the patient and carer of: 1. The diagnosis 2. The prognosis 3. The treatment plan/next steps. The Provider shall address any initial concerns or requests for information from the patient or the carer. The diagnosis shall be shared with the patient’s GP. 4. Dementia (medication) Where medication is indicated, the Provider shall follow the same process as that outlined above, but shall discuss medication as part of the treatment plan. 5. Possible dementia Where the diagnosis is unclear, the Provider shall share the information with the requesting clinician, the patient and the patient’s GP. The patient shall be discharged to their GP who shall be encouraged to refer the patient to the memory service, if available, if the clinical picture changes or if the recommendation is that issues relating to delirium are complicating a possible diagnosis of dementia. [The commissioner should note the importance of a protocol being in place with GPs to ensure that communication of diagnosis takes place, when required.] 28 Stage 2 – Supporting good clinical care Advice on optimum clinical care (2.1) Advice on care planning Check medication & use of psychotropic medication Urgent response & support for patient behavioural management difficulties 29 Advice on capacity decisions and Mental Capacity Act Overview The Provider shall provide timely support and advice to requesting clinicians to help deliver good clinical care of patients with dementia and other mental health needs where there is uncertainty around the optimum treatment. This advice shall include, but not be limited to: care planning checking medication and advising on appropriate use and the use of alternatives to prescribing antipsychotic drugs urgent response and support for patients presenting with behaviours that challenge advice on capacity decisions and the Mental Capacity Act (2005). In most instances, the Provider shall have an advisory role; however, in some cases (e.g. in relation to urgent response) the Provider may provide more direct support to ward staff, if required. Indicators Outcomes This stage contributes to indicators 1–4 This stage contributes to: Outcomes 1–4 2.1 Advice on optimum clinical care One of the roles of the mental health liaison service is to build skills in other health care professionals and improve the standard of care for people with mental health problems and their carers. The service shall respond to requests for advice and support within [one] working day of the request being made and in some cases advice may be given over the telephone. Where urgent attention is requested, the Provider shall respond as soon as possible and within [one] hour. The Provider shall model good clinical care that is patient focused and ensures positive patient experience, including promoting dignity and privacy. The Provider shall comply with good practice from available evidence and policy, including: 30 NICE Clinical Guidelines for dementia/depression/delirium Living Well with Dementia: A National Dementia Strategy (Department of Health, 2009) Who Cares Wins: Improving the outcome for older people admitted to the general hospital (Royal College of Psychiatrists, 2005) The Use of Antipsychotic Medication for People with Dementia: Time for action (Banerjee S, 2009) National Service Framework for Older People (Department of Health, 2001) Discharge workbook Ready to go? (Department of Health, 2011). Health professionals may seek advice and support from the Provider in relation to: Care planning The Provider shall provide advice on care planning to ensure that mental health needs of patients are addressed and to ensure that outcomes of assessments are incorporated into care plans. The Provider shall be available to advise on optimum patient care as it pertains to mental health and shall provide care plans to address and help manage issues that shall include but not be limited to: inappropriate behaviour low mood self-harm psychosis. 31 Checking medication and advising on appropriate use of psychotropic medication in discussion with physicians Older people are particularly susceptible to the effects of combinations of medication. The Provider shall be available to check medications and their combinations and to provide advice on the possible effects, prior to initiation. This includes all psychotropic medications (antipsychotic, anti-depressant and mood stabilisers). In cases of poor reaction or lack of efficacy, the Provider shall provide recommendations regarding changes to medication prescribed for a mental health need, if safe to do so, and advise on alternative strategies as appropriate. The Provider shall give advice on the initiation, maintenance and cessation of psychotropic medication, in line with NICE guidelines. This shall include advice as to whether usage should be reviewed, reduced or stopped post discharge. The Provider shall ensure that the patient’s GP is informed of any decisions made and shall advise the patient’s GP about any review of medication, post discharge, where appropriate. Urgent response and support for patients presenting with behaviours that challenge The Provider shall offer advice and support to staff to help manage behaviours that are ‘out of character’ or behaviours that challenge and which may relate to symptoms of a mental health problem. Ward staff are expected to follow local protocols for deescalation in line with NICE guidelines for dementia and delirium, prior to calling the mental health liaison service. The Provider shall respond to requests from hospital staff and offer advice and support as appropriate, in line with NICE guidelines for dementia and delirium. The Provider shall prioritise these requests for support and shall respond within [one] hour. 32 Advise on capacity decisions and the Mental Capacity Act (2005) The Provider shall give advice on capacity decisions and compliance with the Mental Capacity Act, where required. Where appropriate the Provider shall reinforce the message that a diagnosis of dementia does not mean that a patient does not have capacity. In most instances, ward staff should be competent to make capacity decisions and shall follow their own framework to assess capacity before contacting the mental health liaison service. However, help and advice may be sought from the Provider, where: the level of capacity is genuinely unclear, or a significant decision is to be made (e.g. a change in relation to the place of residence). Where the decision is likely to be in relation to a new place of residence, the Provider shall engage with health professionals, patient and carers in a timely manner in order to try and ensure that discharge is not unduly delayed. In most instances, ward staff should be able to make ‘best interest decisions’ on behalf of the patient and shall only seek advice from the mental health liaison service for more complex cases where there is doubt and as required, for example in relation to: risk issues safeguarding issues. Where requested to do so by a patient or carer, family member or health or mental health professional, the mental health liaison service shall provide advice on sources of independent advocacy support. The Provider shall assist the Trust to develop, implement and review protocols for Deprivation of Liberty Safeguards. 33 Stage 3 – Discharge support 3.1 Review information 3.3 3.2 Advise patient & carer(s) Request for advice or support 34 Advise health and social care professionals Patient discharged 3.4 Contact patient’s GP Overview Planning for discharge should start as early as possible and the Provider shall reinforce this message as part of their contact with health care professionals. This is particularly important for patients with dementia and other mental health problems. The Provider shall provide advice on effective discharge arrangements to patients, carers and health and social care professionals on a request basis. The Provider shall promote Department of Health guidance on discharge: Ready to go? Planning the discharge and the transfer of patients from hospital and intermediate care (Department of Health, 2010). Discharge planning remains the responsibility of the ward staff and adult social care and the mental health liaison service shall advise and contribute to discharge planning as necessary and appropriate. Indicators Outcomes Indicator 2 This stage will contribute to: There will be [x] fewer people discharged directly to a care home as a new place of residence Outcome 2. There will be a reduction in the number of people with dementia discharged directly from hospital to care homes as a new place of residence Indicator 4 There will be [x%] of people who are on antipsychotic medication at point of discharge who have a plan to review use post discharge Outcome 4. There will be an increase in the number of people having a plan to review the use of antipsychotic medication post discharge Page 35 3.1 Review information Discharge planning and support should start as early as possible in the hospital stay. In order to advise on discharge planning, the Provider shall review all relevant information relating to each patient’s (and carer‘s) needs and preferences. The Provider shall review the most recent patient notes and shall consult with hospital professionals for their views and also with patients and carers to understand their needs and preferences. The Provider may also contact community mental services or social services if required. 3.2 Advise patient and carer(s) The Provider shall consult with the patient and carer(s) to ascertain their needs and preferences and shall provide advice to ensure that decisions comply with the Mental Capacity Act (2005). The Provider shall share information that gives the patient and their family an accurate overview of strengths, needs and relative risks, promoting independence and choice. Patients and carers shall be assisted to achieve a timely discharge back to familiar surroundings wherever possible. 3.3 Advise health and social care professionals The Provider shall provide advice from a mental health perspective regarding the recommended place of discharge. Advice shall enable health and social care professionals to take risks and manage risk as appropriate in relation to where the patient should be discharged to and shall provide information about relevant services to facilitate timely discharge. This may include, but shall not be limited to services provided in: social care, community support, housing, primary care intermediate care reablement step-down care. Page 36 The Provider shall reinforce the message that intermediate care or rehabilitation pathways are appropriate for and should be accessible to people with dementia and shall always be considered where the patient is at risk of admission to long-term residential care. 3.4 Contact GP The Provider shall ensure that a letter summarising the main points of the care plan, together with a copy of care plan, is provided to the patient’s GP and, if appropriate, that the care plan is copied to other relevant mental health services. Page 37 E. Indicators When reporting progress against outcomes, the commissioner may wish to consider the measures and indicators set out below: Outcome There will be a reduction in average length of stay in hospital for patients with dementia There will be a reduction in the number of people with dementia discharged directly from hospital to care homes as a new place of residence11 Expected outcomes Yr 1 Yr 2 Yr 3 TBA TBA TBA TBA TBA TBA Indicator description Indicator threshold Measurement Remedy Annual average length of stay in hospital for patients with dementia compared with annual average in baseline year [TBA]10 (x) average length of stay in hospital for patients with dementia in operational year Conversation at quarterly review Annual number of people discharged directly from hospital to care homes as a new place of residence compared with baseline year [TBA]12 (y) average length of stay in hospital for patients with dementia in baseline year [Commissioners to insert any bespoke consequences to apply in accordance with Clause 31.6 of the NHS Standard Contracts.] (x) – (y) = change in average length of stay in hospital for patients with dementia (x) number of people discharged directly to care home as a new place of residence in operational year (y) number of people discharged directly to care home as a new place of residence in baseline year (x) – (y) = change in number of people discharged directly to care home as a new place of residence 10 Indicator thresholds should be set annually at the expected outcome target. 11 Commissioners should note issues around data availability and consider how these may be overcome. 12 Commissioners will need to determine a baseline position prior to agreeing expected outcome measures. Page 38 Conversation at quarterly review [Commissioners to insert any bespoke consequences to apply in accordance with Clause 31.6 of the NHS Standard Contracts.] Outcome There will be an increase in the number of patients with dementia and their carers who have a positive experience of hospital care Increase in the number of people having a plan to review use of antipsychotic medication post discharge 13 Expected outcomes Yr 1 Yr 2 Yr 3 TBA [85%] 100% TBA 100% 100% Indicator description Indicator threshold Measurement Remedy Percentage of patients and carers surveyed satisfied with the service (based on >50% of people who have had contact with the support service returning the survey) [85%]13 (x) Number of surveys with satisfactory score Conversation at quarterly review Percentage of people who are seen by the service and who are on antipsychotic medication at point of discharge who have a plan to review use post discharge (y) Total number of surveys received [x/y] x 100 = percentage of patients and carers who are satisfied with the service [100%] Number of people seen by the support service who are on antipsychotic medication at point of discharge and who have in place a plan to review use post discharge. Indicator thresholds should be set annually at the expected outcome target. Page 39 [Commissioners to insert any bespoke consequences to apply in accordance with Clause 31.6 of the NHS Standard Contracts] Conversation at quarterly review [Commissioners to insert any bespoke consequences to apply in accordance with Clause 31.6 of the NHS Standard Contracts] F. Dashboard The Provider shall report performance using the dashboard template below: Proforma mental health liaison service dashboard report Activity by ward Financials Liaison service originated contacts Savings: Year to date 16 1010 1000 990 980 970 960 950 940 930 920 14 12 £000s Requests made in month £000s Spend:Year to date Ward 10 8 6 4 2 0 Budget Actual Budget Spend: Current month £000s Ward B Ward C 510 500 490 480 470 460 450 440 430 420 £000s Ward A Budget Performance Outcome Reduction in average length of stay in hospital for people with dementia Month X Actual Savings: Current month Actual 9 8 7 6 5 4 3 2 1 0 Budget Actual Provider analysis Yr to date Provide a description of the key performance issues for the provider. Where possible this information should be benchmarked. Where relevant, outline contractual levers being used, e.g. withholding monies Reduction in number of people with dementia discharged directly from hospital to care homes as a new place of residence Increase in the number of patients with dementia and their carers who have a positive experience of hospital care Reduction in the number of people discharged from hospital on antipsychotic medication and increase in number of people with a plan for review post discharge Patient complaints: The commissioner should agree these information requirements with the Provider and these should be inserted into the NHS Standard Contract. Page 40 G. Activity G.1 Activity plan Item Activity for period Assessment and diagnosis (contact) Assessment and diagnosis (advice only, no contact with patient) Management and care planning (contact) Management and care planning (advice only, no contact with patient) Discharge support (contact) Discharge support (advice only, no contact with patient) TOTAL G.2 Individual patient agreements (cost per case) Page 41 H. Finance Annual contract value Service Basis of contract Currency Price Cost per case Total Page 42 Thresholds Total annual expected cost (£) Annex 1: Service accountabilities [The service accountabilities of the hospital trust, the Provider and the commissioner are summarised below. Any changes to these assumptions will need to be reflected in the specification.] Trust Governance and reporting Responsible for establishing scope and boundaries with other services and putting in place protocols to manage service requests (for example between the mental health liaison service and any working-age service) Responsible for establishing management and reporting arrangements between the support service and the Trust. Procedures and protocols Responsible for establishing and implementing procedures and protocols at ward level to improve mental health care. These procedures and protocols should support good quality care, but also help ensure that efficient use is made of the resources available in the mental health liaison service The mental health liaison service can provide support for this but cannot be responsible for it Training and organisational development Responsible for the delivery of training to meet mental health needs and for promoting awareness and profile across the hospital The mental health liaison service can provide support for this but cannot be responsible for it Accommodation and infrastructure Responsible for providing accommodation within the hospital and access to required IT infrastructure Page 43 Provider Identifying need and support The service is based on requests for advice and support; however, the Provider also has the responsibility for identifying areas of the hospital where advice and support may be required. It is responsible for identifying training requirements and, where service remains unsatisfactory for a short period of time, for escalating issues to the management of the Trust for resolution. Assessment and diagnosis Advice and support. The mental health liaison service will provide advice on any aspect of assessment and diagnosis. Only where there is doubt about optimum clinical care will the service provide direct support to carry out one or more functions of the assessment and diagnosis process. Care planning Advice. The mental health liaison service will provide relevant care plans and will provide advice on their implementation. Checking medication Advice. The mental health liaison service will provide advice on medication. This should include contacting the patient’s GP to ensure that review arrangements are in place for the continuing use of antipsychotic medication, post discharge, where appropriate. Urgent response and management Advice and support. The mental health liaison service will provide advice in relation to patient behavioural management difficulties and may provide direct support for cases that require urgent response, as appropriate. Mental Capacity Act (2005) Advice. The mental health liaison service will provide advice on the Mental Capacity Act (2005) for more complex cases where there is doubt about how to provide optimum care. Discharge support Advice. The support service will provide advice to discharge teams and should provide links and information about other services to facilitate timely discharge. Page 44 Commissioner GP protocols For the service to be effective, the commissioner should note that protocols should be in place with GPs regarding communicating diagnosis, where this is required, and reviewing the use of antipsychotic medication post discharge from hospital. Page 45