Community Care Outcomes Framework
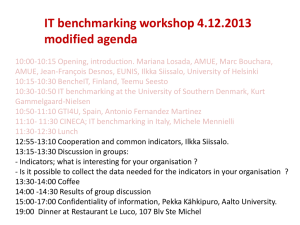
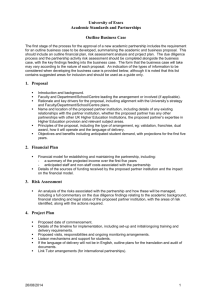
advertisement

Community Care Outcomes Framework Review of the Framework 2006 - 2011 April 2012 Contents Page 3 Executive Summary Background 5 Methodology 6 The respondents 7 Summary of responses 8 Report of workshop to consider responses 10 Discussion / Recent developments 12 Personal outcomes and integration A continued focus on personal outcomes (including the role of staff) Integration of performance frameworks Linkage between national policy and local planning and implementation – the role of Contribution Analysis Recommendations 15 Response of Community Care Benchmarking Network 16 Conclusion 18 Appendix 1 – Community Care Outcomes Framework December 2008 Appendix 2 – local use of Framework at May 2011 Appendix 3 - methodology November 2010 Appendix 4a - the Questionnaire Appendix 4b – questionnaire respondents Appendix 5 - The questionnaire responses: detailed analysis Appendix 6 – Logic modelling 19 2 20 22 25 35 38 50 Review of the Community Care Outcomes Framework Executive Summary In December 2008, following 2 years of gestation, the Scottish Government issued a set of national outcomes for Community Care – or the Community Care Outcomes Framework (CCOF). After three years of local work implementing the Framework it was agreed that 2011 was an opportune time to re-examine it and test whether it was still fit for purpose. The review was carried out by the Scottish Community Care Benchmarking Network and the Joint Improvement Team. The group gathered data through a variety of means: a questionnaire, generally administered locally in an interview setting with key informants in local partnerships or with national stakeholders (86 returned questionnaires were received– 66 as part of individual interviews and 20 as part of groups; 139 respondents overall), five benchmarking projects carried out by Community Care Benchmarking Network a survey of use of the Framework (28 partnerships responded) a policy review. In terms of use of the framework, the large majority of local partnerships are using the majority of the indicators in the Community Care Outcomes Framework to monitor their own local performance. While very few partnerships make use of the full framework, most use 10 or more of the 16 measures, and work is being done at local level to ensure reporting against the majority of measures that are not currently in use. A number of key themes emerged from the questionnaires, and these were developed at a workshop in Summer 2011. The resultant recommendations were put on hold pending the announcement about the Integration of Health and Care in Scotland (December 2011) and have now been reviewed in light of that announcement. The Network members wish to support an approach that moves to one single suite of outcomes and indicators for Integration, for tracking the progress of the Reshaping Care initiative, and for understanding our impact on the personal outcomes for adults using services or support, and their carers. To that end Community Care Benchmarking Network propose to bring the Community Care Outcomes Framework in line with the emerging suite of Outcomes for Integration and to build on the evident enthusiasm across Scotland for sustaining and building an approach which links outcomefocussed practice at the front line with an understanding of performance in improving personal outcomes. The Community Care Outcomes Framework review identifies the focus on personal outcomes as a major strength of the Framework which should be further developed, whilst recognising that we have not cracked reporting on 3 outcomes in a comprehensive and consistent way. Rather within Scotland we are at the stage of grasping what began as a grand ambition, and the Community Care Benchmarking Network members want to see that through in the context of the renewed focus on Integration of Health and Care. The recommendations of the report seek to build on the learning from the Community Care Outcomes Framework to inform the development and use of a single suite of outcomes and indicators, for both reshaping Care for Older People and the Integration of Health and Social Care, particularly in relation to personal outcomes, to continue to encourage and support local use of the Talking Points: Personal Outcomes Approach to focus practice on personal outcomes and to draw information from that process to inform performance management and joint commissioning to support local partnerships to take a whole systems approach in their use of the single suite of outcomes and indicators, and to promote the use of contribution analysis at local level to develop logic models for use in devising local joint performance management frameworks The Community Care Benchmarking Network has accepted the recommendations and sees an important future role in supporting their implementation. 4 Background In December 2008, the Scottish Government issued a set of national outcomes for Community Care – or the Community Care Outcomes Framework (CCOF). This was agreed following a considerable period of consultation with stakeholders across Scotland. There are four high level community care outcomes which challenge partner agencies to improve health, well being, social inclusion and independence and responsibility. Beneath this, sixteen measures are grouped under six themes to support local partnerships to measure progress against each of these outcomes. The framework was accompanied by guidance notes containing definitions for each of the 16 outcomes in the framework. This was to ensure a consistent approach to data collection and reporting across Scotland, for what was a new approach to reporting on community care activity and impact.1 The applicability of the framework was tested from 2007 - 2009 by seven pathfinder/ early implementer partnerships. A key part of this work was to look at how partnerships would be able to implement the framework, the enablers (e.g. IT, training) which might be required to support them and how they might translate the overarching framework into active performance management frameworks at local level.2 The report on this work highlighted the fact that there were local differences in approach and that this had an impact on the way in which the framework was being used across partnerships. 3 From the launch in 2008 up until 2011, there were a number of developments in community care and more widely relating to the way in which local partnerships are expected to measure success and progress. These may be summarised as follows: Further development of the outcomes approach All partnerships due to be compliant with National Minimum Information Standards for Assessment, Care and Support Planning and Review for people using services and for carers (2008), allowing them to report on a new set of personal outcomes indicators. Reshaping Care for Older People initiative which looked at the sustainability of the current model for health and social care services for older people given the demographic shift in the population in favour of older people. Introduction of the NHS Scotland Quality Strategy and associated Quality Measurement Framework, with impacts on the wider performance management for health and social care. 1 Community Care Outcomes Framework, Final definitions, Sept 2008, reference EI/SEP2008/Paper 3 2 Early implementers’ network: role of early implementers, August 2007, reference EA/SEP2007/Paper1 3 Report on the early implementer sites, Jane Mudd Partnership, XXXX 5 By this time, partnerships had had almost three years to work with the Community Care Outcomes Framework and it was agreed that this was an opportune time to re-examine that framework. Vision The review was informed by the following principles, agreed in advance by the members of the Community Care Benchmarking Network: The CCOF should provide a clear outcomes framework which will be meaningful to the public and practitioners are well as those responsible for managing performance and developing policies and strategies The Framework should, first and foremost, be for use locally and not for the purpose of accountability to central government It should be a performance framework which would be outcomes focussed, have improvement indicators and be based on a whole systems approach The framework should focus on the public’s experience of using services and their views on what would make an impact on improving their quality of life It should extend the use of the Talking Points: Personal Outcomes Approach or equivalent It should develop a more holistic and joined-up practice base which would focus on the individual by being person centred It should aim at an integrated health and care quality framework which is a balance of quantitative and qualitative measures. Methodology The review of the CCOF was designed to be as inclusive of stakeholder views as possible. It was seen as critical that front line managers owned and could use the performance information the framework brought together to improve services. It was also agreed that the review should consider the following: Focus on key aspects of practice, processes, systems and organisational culture Whether the Community Care Outcomes Framework should extend to other client groups, particularly mental health and learning disability groups A focus on what works within the current framework rather than seeking to create something entirely new The review was overseen by a project team made up of the Executive Group of the Community Care Benchmarking Network, representatives from the Benchmarking Network and representatives from Scottish Government and the Joint Improvement Team. The Scottish Community Care Benchmarking Network is a member-led collaboration of the health and social care partnerships in Scotland. Growing 6 out of the early implementers of the Community Care Outcomes Framework, the network now boasts almost comprehensive membership from health and social care partnerships across the country and works to its own constitution which sets out an overarching aim of contributing to “the development of national and local performance standards and good practice in Community Care” across Scotland. The Network has run five Benchmarking Projects, each focussing on a different theme within the Community Care Outcomes Framework. These have generated learning and insights about the existing measures and their efficacy in supporting improvements in performance. A report was made available in June 2011 and this fed into the present Review of the Community Care Outcomes Framework. The Review project team devised a clear project definition document, project plan and timetable. The first phase of the review began in February 2011 based on a standardised questionnaire covering both current use, and future development of, the Community Care Outcomes Framework. The group gathered data through a variety of means. A questionnaire for stakeholders on their experiences of using the CCOF and how beneficial this had been in terms of supporting local practice on outcomes. The questionnaire consisted of three sections: 1. Questions 2- 9 considered the current use of the framework. 2. Questions 10 – 18 considered the future use of the framework 3. Question 19 invited respondents to provide more detail on any of the issues already covered, or to discuss issues they felt were important, but not covered in the main questionnaire. A copy of the questionnaire is included as appendix 4a to this report. Members of the benchmarking network were asked to engage with local stakeholders in completing the questionnaire. A list of possible stakeholders was distributed with the questionnaire. Members were given discretion as to how best to use the questionnaire locally – this could be done on a one-to-one basis or through focus groups. The questionnaire was complemented by a survey on the local extent of use of the 16 national measures (the Community Care Outcomes Framework). This survey was administered electronically via the Community Care Benchmarking Network. A review of policy documents relating to community care. The main aim of the review was to identify key themes contained in current policy documents and to use this as the basis of a gap analysis in terms of themes covered by the current CCOF. 7 The Respondents 28 (of 32) partnerships responded to the survey on the local extent of use of the 16 national measures. A total of 86 returned questionnaires were received– 66 as part of individual interviews and 20 as part of groups. This involved 139 respondents. 15.1% of respondents were described as ‘senior managers’; 14.4% were performance managers and a further 9.3% were information officers. The majority of respondents worked either in a local authority, CHP or CHCP, but there were also a small number from representing particular interest groups (such as carers) or national policy agendas. In addition to the 28 partnership responses to the survey on local use of Community Care Outcomes Framework, questionnaire returns were received from 24 of the 32 partnerships operating across Scotland. In addition to these, 15 responses were received from Scottish Government, including a number of officers who hold positions as policy leads. There were also a further 3 NHS, 2 scrutiny bodies and 4 third sector organisations (some organisations submitted multiple questionnaires reflecting different perspectives). A full list of questionnaire respondents by position and organisation may be found at appendix 4b to this report. Summary of Responses The large majority of local partnerships are using the majority of the indicators in the Community Care Outcomes Framework to monitor their own local performance. While very few partnerships make use of the full framework, most use 10 or more of the 16 measures. The survey indicates that the work is being done at local level to ensure reporting against the majority of measures that are not currently in use, and that there has been significant progress across Scotland in the use of the framework since 2009 when a similar survey was carried out across the 32 partnerships. There was a general endorsement of the outcomes approach and the Community Care Outcomes Framework which was seen as supporting this. There was continued support for a balanced approach combining input, output and outcome measures, but a significant feeling that the outcomes approach should be strengthened, particularly in favour of personal outcomes. The crucial role and attitude of staff in ensuring a successful transition to outcomes approaches which impacted on service user and carer experience was noted. The majority of respondents felt it was too early to say how effective the framework had been in influencing local performance or in improving outcomes for service users. 8 There was also a strong sense that the framework was not working as a whole systems approach, and that further work was needed to support partnerships in making links across individual themes and sets of measures. National policy leads also indicated an interest in how the framework could be used to reinforce the links between national policy and local planning and implementation. A final comment summarises the overall impression from the questionnaires which is one of support, but recognising that it is still early days in terms of our work to assess the impact of our work on securing better outcomes for service users. “Where would we have been without CCOF? – It has helped to move thinking but lots further to go – we’re not yet at the tipping point.“ 9 Workshop July 2011 Objectives of the Workshop 1. Agree a final set of outcomes, measures and a framework within which they fit; a Community Care Outcomes Framework “mark II” 2. Agree a shared understanding of the strategic fit with the National Performance Framework and other performance agendas Participants agreed that: There was value in continuing with the Community Care Outcomes Framework It should aim to capture outcomes for all care groups It should retain a mix of input/process/output and outcome measures Content The participants agreed the CCOF should be meaningful, person-centred toolkit that supports improvement and the objectives of the Framework should: 1. Focus on the benefits for service users and for carers 2. Provide a consistent framework for local and national reporting 3. Drive improvement across and within community care partnerships A Vision for the framework was agreed as: “A framework to understand how well we work with people to achieve their outcomes and how we could do it better” PUTTING MEASURES INTO THEMES Two broad outline versions were created and put into themes as follows; INPUTS PROCESSES OUTPUTS OUTCOMES THEMES A1 A2 A3 Q3 S1 S3 User Outcomes 10 INPUTS INPUTS BC1 BC2 PROCESSES PROCESSES OUTPUTS OUTCOMES THEMES A1 A2 A3 C1 / C2 S2 Talking Points measures Carer Outcomes OUTPUTS OUTCOMES R1 R2 Housing measure Anticipatory care (replacing R3) Telecare Re-ablement Mobility Dying where you want Living where you want BC3 THEMES Supporting independence, safety, and care at home ACTIONS / NEXT STEPS The following actions were agreed at the end of the workshop: ACTION: Populate logic model with measures relating to the 3 themes ACTION: Reword existing measures not currently included in NHS HEAT or Statutory Performance Indicators ACTION: Develop definitions for new measures based on existing models in use in East Renfrewshire and Orkney ACTION: Articulate links to NHS HEAT Local Delivery Plans and Community Planning 11 Discussion / Recent developments Personal outcomes and integration On 12 December 2011 the Cabinet Secretary for Health Wellbeing and Communities announced the Government’s plans for integration of Health and Social Care for adults in Scotland. The approach has started with the key questions about what matters most to people who use these services - what are the improvements they want to see and what are the barriers in the current system that prevent staff from using their skills and resources to best effect. As a result of this, the Government has agreed with COSLA that new Health and Social Care Partnerships will be accountable to Ministers, leaders of local authorities and the public for delivering new nationally agreed outcomes. These will initially focus on improving older people's care and are set to include measures such as reducing delayed discharges, reducing unplanned admissions to hospital and increasing the number of older people who live in their own home rather than a care home or hospital In the light of this development we understand that a single suite of health and care outcomes will be presented as part of the engagement phase of the Integration work in 2012. Those outcomes will be supported by a set of indicators, and local health and care partnerships will be held accountable for their progress against these indicators. The Community Care Benchmarking Network has considered this announcement and its implications for the review of the Community Care Outcomes Framework. The Network members wish to support an approach that sees one suite of outcomes and indicators for Integration, for tracking the progress of the Reshaping Care initiative, and for understanding our impact on the personal outcomes for adults using services or support, and their carers. To that end Community Care Benchmarking Network propose to bring the Community Care Outcomes Framework in line with this and to build on the evident enthusiasm across Scotland for sustaining and building an approach which links outcome-focussed practice at the front line with an understanding of performance in improving personal outcomes. The Community Care Outcomes Framework (2008) includes 6 measures which are explicitly based on asking individual people about their own experience of the impact of services and support. Some local partnerships have managed to collect that information from individual care and support plan reviews and to aggregate it to provide useful performance information, which in turn is used to inform future service commissioning. Community Care Benchmarking Network wish to continue to support this approach and to see it built into the outcomes and indicators used to drive the integration process. 12 A continued focus on personal outcomes (including the role of staff) The Community Care Outcomes Framework is perhaps unique in Scotland in focussing largely on the personal experience of people using support or services, and of carers. The Review has emphasised the perceived value of that approach amongst the local and national stakeholders, and the Community Care Benchmarking Network members have confirmed that they wish to continue to promote this approach, within the context of the single suite of outcomes for integration. The Community Care Benchmarking Network has developed a stream of work built around the Talking Points: Personal Outcomes Approach which seeks to promote outcome-focussed practice at the front line of health and care. Staff need to be supported to work in this way, and this fits well with the process benchmarking approach adopted by the Network. The Institute for Research and Innovation in Social Services has recently carried out a review of the Talking Points: Personal Outcomes Approach. One of the key findings is that more work needs to be done to articulate the links between person-centred practice and performance management within health and care partnerships. Community Care Benchmarking Network will work with Talking Points leads to further develop this linkage. One of the key challenges to including a focus on improving personal outcomes in performance measurement at a national level has been the requirement to meet the quality standards of national statistical releases. In order to gain support for the inclusion of personal outcomes in the suite of outcomes and indicators for integration of health and care, it will be necessary to have robust data at local partnership level which allows comparison and aggregation across Scotland. In order to achieve this, the work on the suite of Outcomes and indicators for Integration includes a proposal for a survey of the experience of people using care services or support. This might be carried out nationally or locally but would require to contain a core set of questions that are administered consistently across all partnership areas. The Community Care Benchmarking Network supports this proposal in principle and suggests that the Talking Points Outcomes Frameworks be used to generate the core questions. Community Care Benchmarking Network also emphasised the importance of continuing to support local work to gather information from individual assessments and reviews. These generate a rich source of quantitative and qualitative data which can be analysed and used locally to inform performance management and joint commissioning. This cannot be done so effectively on the basis of surveys, so any nationally agreed care user survey should augment rather than replace local work to link outcomes-focussed practice with performance management and joint commissioning. 13 Integration of performance frameworks Community Care Benchmarking Network has also agreed that it is not appropriate now to promote a refreshed Community Care Outcomes Framework as a separate entity. Rather, the experience and ongoing resource of the Network should be used to promote and support a focus on personal outcomes within the single suite of outcomes and indicators being developed for the Integration of Health and Care. The Community Care Outcomes Framework review identifies the focus on personal outcomes as a major strength of the Framework which should be further developed, whilst recognising that we have not cracked reporting on outcomes in a comprehensive and consistent way. Rather within Scotland we are at the stage of grasping what began as a grand ambition, and the Community Care Benchmarking Network members want to see that through in the context of the renewed focus on Integration of Health and Care. The second perceived strength of the Community Care Outcomes Framework is its presentation as an integrated suite of measures, to be seen as a whole and not isolated for individual attention. The review suggests that there has been less success in embedding this approach than there has been in promoting the focus in personal outcomes. This is perhaps not surprising since the Community Care Benchmarking Network has not adopted this as a key work strand to date. Nonetheless it remains important and is another strong message that the Community Care Benchmarking Network wishes to play into the development of the performance approach associated with the integration of Health and Care in Scotland. Linkage between national policy and local planning and implementation – the role of Logic Modelling Community Care Benchmarking Network has responded to the findings of the Review of Community Care Outcomes Framework about understanding the links between local actions and outcomes and national outcomes by drawing up initial logic models for the three core outcomes that emerged from the July 2011 workshop; Experience of people using service or support Experience of carers Supporting independence, safety and care at home The products of this work are at Appendix 6 to this report. The Network is building its experience of using this technique and believes that it can be highly effective as a means of building local trust and consensus around what needs to be done to improve the experience of people using services and support, and of carers. This can be developed to support a local joint performance framework. 14 Logic modelling can be seen as a strand of broader benchmarking activity and the Network is willing to support peer working whereby experienced partnerships work with others to develop local Contribution Analyses. Recommendations 1 The Scottish Government should work with all relevant stakeholders to agree a single suite of outcomes and supporting indicators for the Integration of Health and Social Care, and Reshaping Care for Older People, which clearly demonstrates the impact of these initiatives on personal outcomes for people who use care and support, and their carers. 2 Scottish Government should not promote the Community Care Outcomes Framework as a separate entity; rather, the learning from the Community Care Outcomes Framework should inform the development and use of the single suite of outcomes and indicators, particularly in relation to personal outcomes. 3(a) Local partnerships should be encouraged and supported to use the Talking Points: Personal Outcomes Approach to focus practice on personal outcomes and to draw information from that process to inform performance management and joint commissioning. 3(b) At the same time, a national care experience survey should be developed to generate objective data about personal outcomes for people using health and care services, to feed the single suite of outcomes and supporting indicators, and to sit alongside locally generated information. 4 Local partnerships should be encouraged to develop their understanding of how the various indicators in the single suite interact and influence each other. Support should be offered to partnerships to do this, as appropriate. 5 Local partnerships should be encouraged to use contribution analysis approaches to generate locally agreed logic models which explain how personal outcomes and system outcomes will be improved in the local area. 15 Community Care Benchmarking Network – proposed contribution to implementation of recommendations Recommendation Proposed Community Care Benchmarking Network contribution 1. Single suite of outcomes and indicators for integration of health and social care The SCCBN will participate; a) in the transition to an Outcomes based approach to performance 2. Community Care Outcomes Framework to be integrated into a single suite model Assist in the transition from the use of the CCOF to implementing an agreed single suite of measures. 3a. Measuring personal outcomes - Talking Points Collaborate in: b) in the development of an integrated suite of health and social care measures for all Partnership services that are both qualitative and quantitative, including personal outcomes measures, suitable for benchmarking, a) an examination of the theoretical and practical issues underpinning the capture, analysis and use of information for adults and carer outcomes in health and social care settings. b) the development of ways to link recording, aggregation of data and feedback to staff and through the outcome review process 16 Recommendation Proposed Community Care Benchmarking Network contribution 3b. Measuring personal outcomes - national survey SCCBN to regularly support collection, collation and reporting on results. Use Benchmarking activity and analysis as a step to improving results for people who use services and their carers through better and more focused reporting of joint performance 4. Whole system performance Partner in promoting and supporting improvement Facilitate the sharing and development of best practice and service excellence in Community Care through benchmarking, the exchange of information and identifying ‘what works’ 5. Contribution analysis Continue to promote and support the work of the Community Care Benchmarking Network subgroup to develop this approach - and implementation as part of Benchmarking 6.Implementing Recommendations SCCBN is remitted to act as a resource to support the development and delivery of the first 5 recommendations 17 Conclusion The review of the Community Care Outcomes Framework concluded its work on schedule in September 2011. Findings were documented and plans for development discussed. By that time it was clear that an announcement about integration was imminent and would be of relevance to the recommendations and action plan arising from the Review. The Review Project Team has worked with the Community Care Benchmarking Network membership to re-frame the recommendations of the Review and to consider the potential contribution of the Network. The role of Community Care Outcomes Framework and Community Care Benchmarking Network in developing and promoting a focus on improving personal outcomes for people using support or care services, and their carers, has led to a significant pool of expertise and experience across Scotland. Drawing on that for the next phase of integration remains critical. The Scottish Community Care Benchmarking Network will do all it can to continue to promote this focus, in line with the wishes and aspirations of those who contributed to this review. 18 Appendix 1 Outcomes Framework for Community Care 2009-10 National Outcomes Improved health Improved social inclusion Improved well-being Improved independence and responsibility Performance measures and data sources Themes User/Carer Experience Code S1 Measure % of community care service users feeling safe. Type Outcome Data Source / Status Data drawn from NMIS E/N N S2 Outcome Data drawn from NMIS N Outcome Data drawn from NMIS N Output HEAT Standard E Output A2 % of users and carers satisfied with their involvement in the design of care package. % of users satisfied with opportunities for social interaction. No. of patients waiting in short stay settings, or for more than 6 weeks elsewhere for discharge to appropriate setting. No. of people waiting longer than target for assessment, per 000 population. No. of people waiting longer than target time for service, per 000 population. Output A3 % of carers who feel supported and capable to continue in their role as a carer. % of user assessments completed to national standard. % of carers’ assessments completed to national standard. % of care plans reviewed within agreed timescale. No. of emergency bed days in acute specialties for people 65+, per 100,000 pop. No. of people 65+ admitted as an emergency twice or more to acute specialties, per 100, 000 pop. Percentage of people 65+ admitted twice or more as an emergency who have not had an assessment. Shift in balance of care from institutional to ‘home based’ care. % of people 65+ with intensive needs receiving care at home. % of people 65+ receiving personal care at home. Outcome Pending Implementation of Lord Sutherland’s Review of Free Personal Care Pending Implementation of Lord Sutherland’s Review of Free Personal Care Data drawn from NMIS N S3 A1 Faster access Support for carers C1 Q1 Quality of assessment and care planning Q2 Q3 R1 R2 Identifying those at risk Moving services closer to users patients R3 BC1 BC2 BC3 Measures: 6 (7) outcomes 7 output Process N Output Data drawn from NMIS and local systems Data drawn from NMIS and local systems Data drawn from NMIS Outcome HEAT target (T12) E Outcome National Indicator reported in Scotland Performs E Output Measure administered through ISD E Input No overarching measure Input/ Outcome Output (proxy) HEAT target (T8). Measure administered through ASD Measure administered through ASD Process 2 process 2 (1) input NMIS is National Minimum standards for assessment, shared care and support plans and review (July 2008) HEAT is the NHS Scotland suite of measures and targets on which NHS Boards base their annual Local Delivery Plans. All references here are to HEAT 2009/10. ISD is the Information Services Division of NHS Scotland ASD is the Analytical Services Division of Scottish Government E – existing - measure in place in 2008 or before N – new - measure defined December 2008 19 N N E&N E Appendix 2 Local use of Community Care Outcomes Framework as at May 2011 20 Partnership S1 S2 S3 A1 A2 A3 C1 Q1 Q2 Q3 R1 R2 R3 BC1 BC2 BC3 Dundee No No No Yes Yes Yes No Yes Yes Yes Yes Yes Yes Yes Yes Yes Orkney Islands Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Western Isles Yes Yes Yes Yes In Progress No In Progress In Progress Yes Yes Yes Yes Yes West Dunbartonshire Yes Yes Yes Yes Yes Yes Yes Yes Yes In Progress Yes Yes Yes Yes Yes Yes Argyll and Bute yes yes yes Yes Yes Yes yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Perth and Kinross No Yes No Yes In Progress In Progress In Progress In Progress In Progress In Progress Yes Yes Yes Yes Yes Yes North Lanarkshire Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Fife Council/NHS Fife No No No Yes Yes Yes Yes Yes Yes Yes Yes Yes CEC In Progress In Progress In Progress Yes No No In Progress Yes Yes Yes Yes Yes Yes Midlothian Yes Yes Yes Yes Yes In Progress In Progress In progress Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Stirling In Progress In Progress In Progress Yes Yes Yes In Progress Yes Yes In Progress Yes Yes Yes Yes Yes Yes North Ayrshire yes Yes Yes Yes In Progress Yes Yes Inprogress Yes Yes Yes Yes Yes Yes East Ayrshire In Progress In Progress In Progress Yes Yes No In Progress In Progress In Progress In Progress Yes Yes Yes Yes Yes Yes East Dunbartonshire In Progress In Progress In Progress Yes Yes Yes In Progress No No No Yes Yes Yes Inverclyde In Progress In Progress No Yes Yes Yes In Progress Yes No No Yes Yes Yes Yes Yes Yes West Lothian In Progress In Progress In Progress Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Clackmannanshire In Progress In Progress In Progress Yes Yes Yes In Progress Yes Yes No Yes Yes Yes In Progress Yes Yes Aberdeenshire In Progress In Progress In Progress Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Aberdeen In Progress In Progress In Progress Yes Yes Yes Yes Yes Moray Yes Yes Yes Yes Yes Yes City of Glasgow In Progress No Renfrewshire No South Ayrshire In Progress In Progress In Progress Yes Shetland In Progress In Progress No Yes Yes Yes In Progress No Scottish Borders Yes yes yes no no yes Yes Yes East Renfrewshire yes Yes No yes yes Yes In Progress Yes No Yes In Progress Yes No Yes In Progress No Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes In Progress Yes Yes Yes No Yes Yes Yes Yes Yes Yes Yes No Yes Yes Yes Yes Yes Yes In Progress In Progress In Progress yes Yes Yes y Yes Yes Yes still to be finalised) Yes to be finalised) guidance progress Instill times guidance No (waiting No (waiting times Yes In Progress No Yes Yes In progress Yes East Lothian S Lanarkshire Highland Falkirk 21 No No In progress Yes No Appendix 3 Methodology 1. Scope of the Review 1.1 Performance Framework In August 2010, a Benchmarking Network workshop considered where the review should focus its energies from the range of outcome-focussed performance measures in use in Scotland – see diagram below National purpose National Outcomes National Indicators ~ NHS Quality Measures Menu of Local Indicators ~ HEAT Local Joint Performance Frameworks Single Agency indicators Departmental performance indicators Local team performance indicators Individual personal objectives It was anticipated that The National Performance Framework would be reviewed in 2011 following the May 2011, Parliamentary elections. The NHS Quality Strategy, announced earlier in 2010 proposed a Quality Measurement Framework that will encompass three levels of measures, underpinning the three quality ambitions. (See http://www.scotland.gov.uk/Resource/Doc/311667/0098354.pdf). Analysis and consultation was taking place with a view to agreeing 12 national Quality Outcome Measures (Level 1) by October 2010 for implementation alongside the related set of HEAT targets (Level 2) for 2011/12. It is clear that with 5 of the 16 measures refer explicitly to people over 65, the current suite of measures is weighted towards older people. However, since 2006 work with other areas of policy in Scottish Government and local partnerships has sought to promote a model whereby the Community Care Outcomes Framework is genuinely an overarching framework for all of community care, with specific client group measures or service-based measurement fitting underneath this umbrella. This makes sense in trying to align reporting within a single performance framework and representatives from the Community Care Benchmarking Network, Scottish Government and the NHS Quality Strategy Team had been discussing the potential for alignment of the two frameworks and all were present at the workshop in August 2010. 22 1.2 Scoping and Planning Given the investment going back to 2006 by Scottish Government, Health and Care Partnerships and other stakeholders, the importance, complexity and the potential longer term impact of the proposed review demanded an approach which was well structured and resourced. This required skills of leadership and project management as well as technical knowledge and expertise. The workshop agreed to follow project management principles, based on Prince 2 methodology. This led to a Governance, Structure and Management framework being agreed giving us; A project board A project team A project manager A reference group This hierarchical structure should give clear lines of accountability with roles and responsibilities agreed, as well as providing support and guidance for completing specific tasks and/or objectives, including the need to have wider stakeholder involvement and/or buy in to the review, e.g., COSLA, ADSW, and NHS Scotland. The Benchmarking Network and Joint Improvement Team partners agreed an outline Project Definition document to Review the Community Care Outcomes Framework as follows: Scope: 1. To review the Community Care Outcomes Framework (2008) through evaluating its application and impact in all 32 Community Care Partnerships. 2. To make recommendations on improving its content in order to facilitate more effective, and wider application through local partnerships working to support people to live full and positive lives in their own homes or in a homely setting. Objectives: Identify and involve stakeholders in review process Review and analyse linkages with all relevant policy initiatives and performance frameworks in health and care, identifying synergies and gaps Determine most appropriate model linking Community Care Outcomes Framework to National Performance Framework and supporting systems Review name “Community Care Outcomes Framework” and recommend new name if appropriate Evaluate work undertaken by local partnerships since April 2007 23 Evaluate benefits derived from use of individual measures and groups of measures Determine what measures should be removed, possible improvements to existing measures and any new measures Report to Health and Care Delivery Group by September 2011 Project start date: November 2010 Project Sponsor: Project finish date: September 2011 Partnership Improvement and Outcomes Division Project Managers: Co-ordinator of Community Care Benchmarking Network and Lead on Community Care Outcomes Project Board: Outcomes Approach to Community Care Co-ordinating Group Project Team: from SCCBN, Scottish Government and ISD 1.3 Project Team The Project Team met 4 weekly from November 2010 to October 2011 managing the following project plan. January 2011 PLAN - Preparation of tools to collect data and other intelligence from stakeholders February DO - Consult stakeholders. Conduct interviews and surveys March REVIEW (1) - Examine the work undertaken by local Partnerships in applying the Community Care Outcomes Framework April to May REVIEW (2) – Carry out survey of all stakeholders June REVISE - Evaluate ‘what works’ - Agree a framework, a final set of outcomes and measures - A shared understanding of the strategic fit with the National Performance Framework and other performance agendas July to August REPORT - Feedback findings and recommendations to Stakeholders September 2011 REPORT – Submit report to Health and Care Delivery Group 24 Appendix 4a Questionnaire Community Care Outcomes Framework Review Stakeholder Questionnaire 1. Responder’s organisation : Position (please mark an ‘x’ in the most appropriate boxes which reflects the contribution from an individual response or from a group): NHS Local Authority Politician / NHS Board member Director of Social Work CHP General Manager Planning Lead Performance Manager Team leader Carer National Policy lead Joint Working Manager Senior Manager Information Staff Frontline practitioner Service user Focus Group Other (please specify) Section 1: Questions about the current use of the framework (Please note: A one page summary of the Community Care Outcomes Framework is appended as an aide memoire) 2. Which statement best describes how the framework has – or measures from the framework – been used in your area? a) To carry out a whole-systems analysis of performance of local community health and care services b) To investigate parts of the whole system using some of the measures c) We haven’t used the framework d) Other (please describe) 25 NB: If possible, can you provide us with copies of the relevant documents which show how it has been used? 3. Have you used some of the measures or themes more than others? If so: a) Which ones? (a copy of the framework appears at the end of this questionnaire) b) Why? 4. The framework includes hard measures (egg. A1, R1), and also soft measures (S1-3 and C1) aimed at capturing user/carer experience. a) Do you have systems in place to collect the measures related to quality of assessment and planning (measures Q1-3)? Yes No If yes, what do you use the information for? Is it used on a regular basis? If no, what have been the barriers to data collection? 26 b) Do you have systems in place to collect the measures related to user/carer experience (measures S1-3 and C1)? Yes No If yes, what do you use the information for? Is it used on a regular basis? If no, what have been the barriers to implementation? 5. Has your partnership found an effective way to report on the user/carer experience measures (S1, S2, S3 and C1)? If so, please describe how you have done this. 6. Has your partnership developed any measures locally that you have found to be useful in measuring performance? If so, please tell us what they are. 27 7. Are there any measures in the existing framework that you think need to be reworded to make them clearer? If so, please tell us which ones, and your suggested changes. 8. To what extent has the framework helped you to: a) Understand the performance of your local community health and care services and the interplay of the range of factors? Please explain b) Influence the performance of your local community health and care services and the interplay of the range of factors? Please explain 28 9. Overall, how effective has the framework been in improving personal outcomes for people using community health and care services or support? Please give a rating from 0 to 10, where 0 means not effective at all or Don’t know 0 1 2 3 4 5 6 7 8 9 10 o Why you have given this rating? o If your view is that the framework has been effective in improving personal outcomes, please describe some examples of this happening? 29 Section 2. Questions about the future of the framework 10. What should the framework seek to achieve in future? 11. What groups of clients should the framework address? 12. Is the Community Care Outcomes Framework the right title for this purpose? If no, please offer suggested alternatives. 30 13. How important is it that the framework continues to include a mix of quantitative (‘hard’) and ‘soft’ measures? o Please rate on a scale of 0 to 10, where 0 is not at all important and 10 is vital or Don’t know 0 1 2 3 4 5 6 7 8 9 10 o Why you have given this rating? 14. The current framework includes measures on input, process, output and outcome measures. Is the balance right? 31 15. How important is it for you that we have a framework of defined measures: For use in your locality (Please rate on a scale of 0 to 10, where 0 is not at all important and 10 is vital) or Don’t know 0 o 1 2 3 4 5 6 7 8 9 10 Why you have given this rating? For use across Scotland, to allow you to compare performance across areas? (Please rate on a scale of 0 to 10, where 0 is not at all important and 10 is vital) or Don’t know 0 o 1 2 3 4 5 6 7 8 9 10 Why you have given this rating? 16. What would be useful to support the partnership in their use of the framework in future? From internal sources From the Community Care Benchmarking Network From the Scottish Government From others? 32 Section 3. Implementation of a personal outcomes approach 17. On a scale from zero to ten, how would you rate progress within your partnership area in implementing a personal outcomes approach? Zero would be “implementation has not begun” Ten would mean “fully implemented” or Don’t know 0 o 1 2 3 4 5 6 7 8 9 10 Why you have given this rating? 18. If you have made progress in implementation, which of the following do you currently use the personal outcomes approach for? Assessment Performance Management Joint Commissioning 33 19. Please include any other comments relating to your experience of using the Community Care Outcomes Framework if you feel these have not already been covered. Thank You 34 Appendix 4b Questionnaire Respondents by position and organisation Total Number of Responses Organisation Partnerships NHS Scottish Government Scrutiny Body 3rd Sector Number of responses 24 3 15 2 4 (Some organisations submitted multiple questionnaires) Breakdown of respondents by organisation Organisation Respondents Aberdeenshire Council 3 x Strategic Development Officer, Head of Service, Information Officer Aberdeenshire CHP Planning lead NHS Grampian Performance manager, project manager older people services, joint working manager, senior manager and frontline practitioner Care Commission Regulator Clackmannanshire Director of Social Work 2 x Senior Manager Information Staff Policy & Planning Support CHP General Manager Dundee Partnership CHP General Manager Head of Community Care Performance Manager Dundee CHP Planning and Development Manager Strategy & Performance Manager Senior officer (Information - Community Care) Senior Officer (Outcomes) East Ayrshire Director of Social Work, CHP Facilitator; Senior Manager, Community Care: Planning Lead/Performance Manager East Dunbartonshire Council Information staff/ performance manager East Dunbartonshire CHP Planning / performance manager East Renfrewshire CHCP Performance manager, team leader, commissioning and development co-ordinator, joint working manager, team leader. NHS Lothian Strategic Programme manager (community planning) Edinburgh Senior manager (operations) , R & I manger, joint programme manager & planning lead Senior manager( performance and information) Fife Team leader, senior manager, information staff Glasgow City Council Social Planning Manager - Service-wide Work Services Performance Manager - Service-wide Performance Manager - Adult Services NHS Greater Glasgow & Clyde, CHP Sector Director 35 Glasgow City CHP Health Scotland Highland Inverclyde CHCP Midlothian Moray CHSCP Reshaping care for older people NHS Ayrshire and Arran NHS Ayrshire and Arran and North Ayrshire council North Ayrshire Council NHS Tayside NHS Lanarkshire North Lanarkshire Social work services Orkney CHCP Scottish Excel Scottish Care VOCAL Scottish Government (Joint Outcomes Team – Integration and Service Development Division) Scottish Government (Policy for Carers) Scottish Government ISD COSLA South Ayrshire Council CHP Planning Manager Local Government Health Improvement Programme Manager Carer, senior manager, Service Manager Performance and Planning ASM Research 3 x senior manager , director of social work Community Care Team (Elgin- . collective response from 6 Community Care Officers including Team Manager), head of community care, NHS business manager Lead officer, lead officer for Lanarkshire partnership for Change Fund programmes Planning lead/ performance manager Joint working manager 2 x Performance Manager, team leader, 2 x Local Authority officers Senior manager Senior manager, team leader Head of social work department, performance manager joint working manager, senior manager, information staff, performance manager, planning lead National policy Lead Chief executive of Scottish care National Policy lead and senior manger National policy lead, team leader Policy for carers team leader Information Adviser Lead for mental health benchmarking Joint working manager Improvement program manager 3 x National policy lead Strategist/Facilitator (policy into practice) JIT policy implementation Strategic Lead, Quality Team in Health Directorate Group National Health and Care Policy lead Chairperson Manager, Strategic Service Planning (LA) CHP Partnership Facilitator(NHS/LA) Manager, Older People’s Services (LA) Research Officer (LA) 36 South Lanarkshire Carers’ Network Stirling Council Social care Service SWIA West Dunbartonshire West Lothian CHCP Western Isles Community Health and Social Care Partnership JIT NHS Performance Forum South Lanarkshire CHP, NHS Lanarkshire South Lanarkshire Council Renfrewshire Council Dumfries and Galloway Dumfries and Galloway social work services Chairperson Performance and Quality Assurance Business Support Senior Practitioner, Occupational Therapy Occupational Therapist Team Manager, Direct Provisions Manager, Carer’s Centre Head of service – resources and performance national policy lead, senior manager, frontline practitioner, CHP general manager, planning lead, performance manager, team leader carer Information Staff , senior manager, performance manager Performance manager Senior Manager (planning lead) Planning and performance manager (emphasis of job on performance) Performance Manager, input from both CHP and SW staff Performance and improvement lead officer Operations Manager 37 Appendix 5 – the Questionnaire Responses: detailed analysis Question 2 asked partners to select a statement which best describes how the framework, or measures from the framework, had been used in their areas. There were 70 responses to this question from 25 partnerships. The majority of respondents stated that their partnerships were using the framework to investigate parts of the system using some of the measures. However, there was a significant minority (13%of respondents) who felt that they were using the framework to carry out a whole systems approach. However, a closer look at responses shows that there is a difference in opinion even within partnerships. When grouped, it is clear that no single partnership answered consistently that the framework was used to carry out a whole systems analysis. This would suggest that partnerships are using the framework to investigate parts of the system using some of the measures. Question 3 asked whether partnerships used some measures more than others and for any reasons behind this use. There were 70 responses to this, from 25 partnerships. This information was supplemented by the responses to the survey on local use. Overall, the measures most used at local level are: A1: delayed discharges BC2: Intensive homecare R1: emergency bed days BC3: personal care at home R2: number of older people admitted twice or more as an emergency R3: number of older people admitted twice or more as an emergency who have not had an assessment All of these measures either are or have been required as part of other reporting systems such as the NHS HEAT targets (Health improvement, efficiency, access, treatment) or local authority Statutory Performance Indicators (SPIs). Measures least used are: S1: % community care service users feeling safe S2: % of users and carers satisfied with their involvement in designing their care package S3: % of users satisfied with opportunities for social interaction C1: support for carers Q1: % user assessments completed to national standard Q2: % carers’ assessments completed to national standard Q3: % care plans reviewed within agreed timescales These appear to be in progress across most partnerships suggesting that the majority of partnerships are developing measures which will sit against the national framework. 38 Overall, this suggests that most partnerships are either reporting or developing mechanisms to report against the majority of measures in the Framework. Responses also suggest that while many partnerships acknowledge that the indicators they use is driven by the information that is available, they also reported considerable developmental work in relation to outcome focussed measures such as S1-S3 and C1 (support for carers). Question 4 focused on the softer measures around the quality of assessment and care planning and service user/ carer experience. There were 70 responses to this, of which 60 answered either ‘yes’ or ‘no’ (remainder were ‘Not applicable’). Of these 60 responses, 45% answered ‘yes’ without any qualification; 30% answered ‘no’ without any qualification; the remaining 25% responded that they collected some but not others. The least likely to be collected was Q2, with Q3 being the most likely to be collected. A review of comments suggested that some partnerships which answered ‘no’ to this question, also collect some of the data, particularly around Q3. Respondent comments focussed on the Q1, Q2 and Q3 measures with some reference to carers’ assessment (proxy for C1) but there were very few references to the user/ carer experience set of measures. In one case, reference was made to NMIS compliance, but this was not explored in terms of use of data locally. Comments highlighting barriers pointed to issues around definition and data reliability which made collecting and using this data problematic. There was also evidence of work to develop systems to collect this type of data in the future. This was also evident in the survey of measures used locally. It should also be noted, that the survey highlights considerable work on all user and carer experience measures. Question 5 continued to focus on S1, S2, S3 and C1, this time asking whether partnerships had found effective ways of reporting on them. A significant proportion of respondents reported that they collect user feedback via surveys, which may either be annual or one off. There is also evidence of work to embed questions on user experience into assessment and review processes – this has already been done in some areas. Fewer respondents mentioned carer experience. Those that mentioned this noted work that was frequently being done in partnership with voluntary sector organisations working with carers to gather data on carer experience. Question 6 asked partnerships to identify any local measures which were useful in measuring performance. Some partnerships pointed out that they did not develop indicators per se, but rather used indicators which already existed in other contexts (e.g. HEAT). A number of partnerships highlighted the fact that they were developing indicators to support service redesign, reablement was mentioned in particular. Almost all partnerships stated that they used a range of indicators and measures to report local performance. Some partnerships gave examples of these, while others merely summarised local arrangements such as “a whole 39 range of measures” and “performance framework based on a basket of measures approach”. Those indicators which have been identified can be grouped under a number of headings. The largest single set of these related to assessment, possibly not surprising given that the national outcomes measures least used related to quality of assessment and care management. A number of measures relating to reablement are also used reflecting the development of reablement approaches since the completion of the CCOF. Other headings included housing, technology (telehealth/ telecare), hospital discharge, care home, and acute hospital measures. There were also some relating to the person such as capacity issues, guardianship and employability. These local suites of indicators were linked to a range of agendas at local level. These included Single Outcome Agreements, Joint priorities for community care and HEAT. There were also some references to local work on health improvement, children’s services, primary care measures, and older people. The relationship between these local suites of measures and the CCOF is not made explicit in answers to this question. Question 7 asked whether there were any measures in the existing framework that should be reworded to make them clearer. Not all responses answered this question. Those that did covered all 16 of the measures in the existing framework, though there was a clear emphasis on some measures more than others. The table below shows those measures which respondents felt should be reworded, and the number of respondents which answered in this way: Measure S1 S3 Q2 S2 Q1 BC2 BC1 A2 A1 A3 Q3 R1 R3 % of community care services users feeling safe % of users satisfied with opportunities for social interaction % carers assessments completed to national standard % users and carers satisfied with opportunities for social interaction % user assessments completed to national standard % of people 65+ with intensive needs receiving care at home Shift in balance of care from institutional to home based care Number of people waiting longer than target for assessment, per 000 population Number of patients waiting in short stay settings or for more than 6 weeks elsewhere for discharge to appropriate setting Number of people waiting longer than target time for service, per 000 population % of care plans reviewed within agreed timescale Number of emergency bed days in acute specialities for people 65+ per 100,000 population % of people 65+ admitted twice or more as an Frequency 17 10 9 8 8 7 5 5 4 4 4 4 4 40 C1 R2 BC3 emergency who have not had an assessment % of carers who feel supported and capable to continue in their role as carer Number of people 65+ admitted as an emergency twice or more to acute specialities, per 100,000 % of people 65+ receiving personal care at home 3 1 1 Some respondents also suggested alternative wording, though the majority did not. The majority of criticism related to definitions, and the need for greater clarity around some of these, particularly where measures were either subjective or broad. Other comments concentrated on the fact that the measures were frequently proxies for outcomes, and that some measures needed to be updated to reflect new approaches, such as reablement and Self Directed Support. Question 8 in the questionnaire asked partnerships to consider two related issues: The extent to which the framework has helped them to understand the performance of local health and care services and the interplay of factors impacting on this The extent to which the framework has influenced this performance 71 of the 86 returns answered this question. Of these 71, 37% (23) felt that the framework was helpful to some extent both in understanding local performance and in influencing this performance. Comments from respondents indicate that they have found the emphasis on outcomes has been beneficial; other comments suggest that the framework has enabled them to raise the profile of performance management for health and social care and allowed partnerships to consider the interaction across a range of areas which impact on the bigger picture. However, a significant minority of 18% (16) felt that the framework was not helpful when understanding the performance of local health and care services. Comments on this highlight weaknesses due to lack of comprehensive reporting against some measures, and the fact that many measures are single agency specific and merely brought together in the reports rather than linking together activity in a meaningful way. It is also noted the even among respondents who were positive about the framework, they felt that other factors influenced local performance. The main one of these is the set of HEAT targets for the NHS. There were some suggestions that local authorities might be more influenced by the CCOF than NHS partners. A further 7% (5) respondents felt it was too early to say whether the CCOF had been helpful or had influenced local performance. Issues raised here included the need for further development on a number of indicators and the lack of benchmarking across partnerships. Question 9 asked respondents to consider how effective the framework had been in improving personal outcomes for people using community health and social care services. This was first using a rating from 0 (low effectiveness) to 41 10 (high effectiveness) and then to explain the answer. There were 64 answers to this question. 26 stated that they did not know and did not give a rating 2 responded that it was not applicable 36 responses provided a rating. These ranged from 0 – 10, with an average of 4.8. Many of the comments suggested that it was too early to tell whether the framework had been effective, or that the ongoing development of many of the indicators meant that the whole system which the framework attempted to represent was not yet operating. There was also a sense that the framework concentrated too much on outputs rather than personal outcomes. However, those who gave high ratings of effectiveness largely felt that the Framework reiterated the outcomes approach and helped to raise the profile of this way of working in social and community care. It was suggested that it provided an effective means for shifting local performance management, though this was limited by how much practitioners understood the outcomes approach. The following comments highlight this: “Really ties into what matters to people. Good balance if the assessment process is right and people have the correct assessment skills – this is key to outcomes.” “I don’t think it has been embedded enough in practice. Talking Points has had more impact.” “Framework has helped system focus much more on outcomes for users/carers – not just inputs/processes and proxies for joint working. But inevitably not all staff “get it” yet”. Questions 10 – 16 were concerned with the future of the framework. Question 10 asked “What should the framework seek to achieve in future?” Three main issues were identified: Achieve improvement in personal outcomes (26%) Improved partnership working (14%) Effective way of benchmarking (13%) A small proportion also suggested that it should be used to demonstrate national policy, become more outcomes focussed and include improved support for carers. Some of the comments made by respondents were clear that the current framework does not focus sufficiently strongly on people’s experiences of using services and the outcomes that they have achieved as a result. There was also a strong sense that any future framework should be developed to ensure consistency in data recording and reporting across agencies which 42 would allow different data sets to be matched, thereby reducing unnecessary duplicate or repeat reporting of data in different formats. For example, one respondent commented: “It should seek to achieve an understanding of a service user’s pathway and show an evidence trail that demonstrates progress towards person centred outcomes, based on quality.” This idea of the pathway was also mentioned by a (different) respondent under question 9. In both cases the comment underpins an idea of the whole system approach which might be provided by the framework. Responses to question 10 also show a difference in opinion as to the future direction of the framework. While the emphasis is on a framework that is centred on outcomes, and particularly personal outcomes, there is a significant minority which seems to be suggesting a framework that will allow consistent reporting across Scotland which will allow for benchmarking and comparisons. This type of response is more common from respondents who work in information management or performance. Question 11 asked which groups of clients the framework should address. 81 of the 86 returns answered this question. The top four groups identified were: All community care client groups (36%) Learning disabilities (15%) Older people (10%) All adult community care groups (10%) Comments varied from those who felt that the framework should not change, to those who felt that it needed to be clearer about whether it was a generic framework for community care, or go down a more specialist route for one particular care group. A number of respondents suggested having an overarching framework with different sections or tabs relating to different client groups sitting beneath this. Examples of comments include: “Looks like a framework of measures for the 65+ age group. Should consider its relevance to reshaping care policy and/or develop a generic overarching framework with bespoke measures for different services.” “The framework appears to be trying to do too much. A decision needs to be made on the focus of the framework. If the focus is to remain on older people, then outcomes can be clarified for this client group. If the framework is to be generic for all community care service users, then the specific 65+ measures should be removed.” “No reason to change the way it is currently set out. It implies a bias towards older people, this reflects the real pressures that health and care services are under, and also the pressures on carers – many of whom are older people.” 43 Question 12 then asked about the name of the future framework and whether the Community Care Outcomes Framework was the right title. Of 86 responses, 43% of these said that this was not the right title; 36% said that it was the right title and 21% did not answer. A number of alternative suggestions were made. Many of these suggested alternative names based on outcomes, but a number reflected the fact that some respondents felt that the framework should be focussed on indicators and measures rather than personal outcomes. A sample of suggestions taken from across the range of suggestions gives a flavour of this variation: Older people’s outcomes framework National community care performance information framework National community care benchmarking framework Community support outcomes Joint performance outcomes Integrated health and social care outcomes framework Question 13 asked how important it was that the framework should include both quantitative and qualitative measures. This was based on a rating from 0 (not important) to 10 (very important) and reasons for giving this rating also requested. There were 74 responses to this question, and 87% of respondents rated this at 8 or higher. The most common reason for this response was that a mixture of measures is required, with 19 responses highlighting the need for ‘balance’. Most of the comments made a case for including qualitative data. One comment suggested that qualitative measures give the framework credibility; another suggested the need to counterbalance the measures so they are ‘not too HEAT driven.’ Many of the respondents thought that the qualitative measures were necessary to add meaning, to ‘get beneath’ or ‘test assumptions behind’ the quantitative measures. A meaningful framework needs both. We need to understand ‘what’ we are doing and ‘why’ we are doing it. Several people highlighted that increased understanding of the outcomes for people using services was necessary to improve service planning, workforce planning and to increase productivity. There was a view that listening to service users and carers could ‘tell you what really makes a difference.’ Eight respondents felt that there should be an increased focus on personal outcomes. However, concerns about qualitative data management were raised by six respondents. One commentator argued that there would be no point in including softer measures ‘if we are unable to quantify them’, while another thought that though the soft measures are challenging, they should remain because they will encourage partners to be more creative. Two respondents 44 thought that the soft measures are too prescriptive and should be determined locally. A minority of three respondents thought that the quantitative measures should be given preference from a benchmarking perspective, because easier to compare, more robust and less subjective. One thought that the need for proxies and process measures would continue until ‘outcomes can be successfully measured’, and another that triangulation was required to make soft data dependable. Two respondents thought that the qualitative and quantitative data should be gathered separately rather than forming one framework, although one of the two thought the data should be interpreted together. Question 14 explored the balance across measures further asking whether the balance between input, process, output and outcomes measures in the current framework is correct. Of the 86 respondents, only 45 answered this question: 27 replied yes and 12 no. A further six said that they didn’t know. Most did make comments which covered a range of views. As with the comments for question 13, 8 respondents said that there should be an increased focus on personal outcomes. Three argued that the framework should be completely about outcomes, with no need for processes and inputs at the national level. More often however, the view was expressed that the outcomes measures needed to be balanced with other types of measure. One respondent was concerned that all other measures might be overlooked ‘in the current ideological discourse about “outcomes”. Overall, there was a suggestion that the balance should be shifted to an increased emphasis on outcomes, with fewer input and process measures in the framework. It was also proposed that greater thought might be given to input measures, identifying those that have a particular impact on achieving specified outcomes. Echoing an issue raised with regard to question 13, two respondents raised concern about the costs and time involved in analysing qualitative data. A more common view was that work was still required to make use of the data in the round and to realise the potential to ‘see the whole picture.’ One suggested that logic modelling could be applied to the framework to link inputs and activities to intermediate and long term outcomes. Another suggested developing a data logic structure to estimate outcomes. One person commented that in its current form the framework is a long way from its potential to improve services because of the skill and knowledge required to drill down in each measure to get to the contributory factors to see what needs to change. Three respondents raised questions about the labelling of some of the current measures, particularly highlighting whether the categorisations of R1 outcome, R2 - outcome, BC1 - input were correct. 45 Question 15 had two distinct parts. The first asked how important it was that we have a framework of defined measures for use at locality level; part two asked how important it was to allow partnerships to compare performance across Scotland. Respondents were asked to rate these on a scale of 0 (low) to 10 (high), and then give reasons for their rating. In terms of the importance for localities, 81% of respondents rated this as being very important (ratings of 8-10). The main reasons why it might be beneficial for localities are as follows: Beneficial for trends/ comparisons/ planning and target setting Useful for internal and external benchmarking Way of evidencing practice and competence Useful to evidence effectiveness of policy and practice change Provides structure clarity and direction re, what we are trying to achieve Help to identify where performance is strong or needs to improve Will help demonstrate improvement in whole system outcomes Supports the development/analysis of other measures locally, influenced by the CCOF Needs to provide clear definitions to allow better performance management and benchmarking Some of these were also highlighted as being significant in terms of comparing performance across Scotland. The main themes identified against this are: Useful for internal and external benchmarking Useful to evidence effectiveness of policy and practice change Help to identify where performance is strong or needs to improve Supports the development/analysis of other measures locally, influenced by the CCOF Needs to provide clear definitions to allow better performance management and benchmarking Could allow better dialogue around data capture and consistent reporting Fundamental to good practice and sharing for improvement Identify and tackle variation to improve performance Needs to be valid benchmarking in terms of comparisons and context With regard to national comparisons, a number of partnerships raised concern that this should not take away from the local prerogative to target areas of local concern, and that comparisons of performance across Scotland should not be used as a form of scrutiny but rather in the context of sharing learning and good practice. Question 16 asked respondents to consider what support they might require in the future use of the framework. Respondents were asked to choose from four options: From internal sources From the Community Care Benchmarking Network 46 From the Scottish Government From others Many respondents selected more than one option and all four were identified as being important. The Benchmarking Network and the Scottish Government were identified most frequently by respondents (69% each) but internal supports followed close behind with 56% of respondents selecting this option. Respondents were also invited to add comments to support their answer. In terms of the Benchmarking Network, a number of respondents qualified their answers by stating the type of support that the Network might provide. This included actual benchmarking, support for consistent approaches across Scotland, and a forum to share good practice. Other themes that were raised in comments include: Need for improved systems to collect data as per minimum information standards Need to address duplication in reporting – this may mean a single set of indicators that satisfy a number of different audiences Need to support data production with high quality analysis, including whole system analysis. Need for stability in reporting requirements to measure improvement over time Need for commitment from all parties Question 17 asked respondents to rate progress within partnerships in terms of implementing a personal outcomes approach from 0 (not begun, to 10 (fully implemented). They were then asked to justify their rating. There were 69 answers to this question, 10 of which were ‘don’t know’ and 59 of which provided ratings. 35 responses gave a rating of 4-6, the average rating being 5.4. It is interesting to note, that where partnerships submitted a number of individual responses, there was not necessarily consistency in the rating provided. For example, one Partnership submitted 6 responses, three from the Council alone, and 3 from the CHP. The responses from the Council were 4, 4 and 6; the three responses from the CHP were ‘don’t know’, 3 and 6. This variation was evident in a number of other partners, though there was no set pattern which suggested that Councils rated implementation more or less highly than NHS partners. Variation in Scottish Government responses was even more marked. Of nine responses, there were three ratings given: 1, 6 and 8. Comments to justify the rating highlighted a number of themes. The most commonly cited was a general difficulty in embedding a cultural change to a focus on outcomes, or ‘doing with’ rather than ‘doing to’. Successes in implementing the approach were felt to be prevalent in small pockets, aided by a well articulated vision and a good understanding of outcomes and desire to improve service provision at senior management level, No common barriers to achieving the required culture shift were identified, though a professional 47 opposition to outcomes approaches, resource constraints and the poor reputation of electronic Single Shared Assessment were all mentioned. Several responses to justify a positive rating mentioned the link between the implementation of the outcomes approach and the use of Talking Points, in particular how well this had been embedded in assessment and review processes. However, several references to Talking Points also noted that implementation had been at small scale or pilot level and that more work was needed to embed it more consistently across partnerships. The role of data systems to support embedding the outcomes approaches in local information systems was also a common theme. This was seen to be consistent with a good understanding of the strategic importance of outcomes at senior management level. Question 18 asked respondents to identify which of three options their partnerships currently used the personal outcomes approach for. These options were: Assessment Performance management Joint commissioning There were 59 responses to this question, 8 of which gave a N/A response. The largest response was assessment, with 37 respondents stating that they used the outcomes approach for this. Performance management was the next largest group with 30 respondents identifying this; fourteen respondents stated that they used the outcomes approach for joint commissioning. A number of responses noted that they used the outcomes approach for more than one option. Again there is some evidence of inconsistency in answers provided by different respondents from particular partnerships. This is true within single organisations (i.e. different respondents from CHP X) as well as differences in response from different organisations within the partnership (i.e. CHP X and Council X). The final question invited respondents to consider any additional information which they would like to note or issues relating to their experience of using the framework that they would like to raise. As expected, this resulted in a wide range of answers, and it is difficult to identify common issues. However, there are a number of themes which recur. Some of these reiterate comments already made in the questionnaire, for example about the ratio of inputs-outputs and outcomes, and a number of people raising the issue about consistency and priority for measures in the CCOF across Scotland. It was also stated that the CCOF needs to avoid being seen as an optional extra – one respondent mentioned its absence in discussions on applying the Change Fund and the reshaping care for older people agenda. The comment below captures some of this concern: It is the groups’ view that the current Community Care Outcome Framework is becoming less relevant as other policy directives gain 48 momentum. (Reshaping OP services, Mutual Care, Community Capacity Building Life stage Planning, Equalities and Diversity agenda) Overall, the comments are supportive of the current approach, with many respondents feeling that the potential in the framework has not yet been realised and that it provides a sound foundation for future development. However, there were a number of comments that highlight the shortcomings of the whole system approach which the framework was supposed to promote. A number of respondents expressed a sense that the framework did not link up processes across organisations. The following quotes are representative of this type of comment: The Framework has taken discrete parcels of info that are available and presented them. What we need to do is support a person-based approach locally by joining up health and social care data (e.g. social care data and emergency admissions and deaths) so that there is a good joint ‘information reservoir’ as put forward in the Interlink Paper (February 2011) The CCOF is a mix of measures applicable to ‘social’ care and ‘health’ but do not provide scope for measuring joint performance. You either ‘fit’ into a category that applies to your organisation or do not. Therefore, the 16 measures are not easily applicable to all Community Care parties and ‘slanted’ towards local authority reporting. The framework is geared to 65+ but should be applied to all ages for example Disability services and Mental Health Services. Respondents also suggested potential areas for development. These might include developmental measures and there should also be links into other organisations, including the nascent SCSWIS. Again, there was a repeated call for consistency in language and data collection, and the need to streamline reporting mechanisms to avoid duplication or repeat reporting. This was also seen as important given the financial constraints under which partnerships would be working in the coming years. Measures need to be expressed in a consistent manner across all statistical reporting without repetition, overlap or differences in data dictionaries A final comment summarises the overall impression from the questionnaires which is one of support, but recognising that it is still early days in terms of our work to assess the impact of our work on securing better outcomes for service users. Where would we have been without CCOF? – It has helped to move thinking but lots further to go – we’re not yet at the tipping point. 49 Appendix 6 – Logic modelling The logic model tool has developed over the last quarter of a century and has its origins in programme management and evaluation. Logic modelling is a flexible approach that can be used for many scenarios – from small-scale projects to national strategies. In using the logic model approach we start with outcomes and the inputs, activities and outputs that lead toward these outcomes. Feedback loops are built into the model by way of evaluative performance measures. In logic modelling it’s important to be specific about what we mean by outcomes. Outcomes refer here to end impact, i.e., the changes that occur or difference made for individuals, families, groups of people or communities as a result of the implementation of certain plans. The logic model approach also locates this within a context of assumptions and external factors. One example is given below. A sub-group of the SCCBN, involving City of Edinburgh, East Renfrewshire and South Lanarkshire partnerships, used a logic model approach in the review of the Community Care Outcomes Framework. The approach was employed in considering health and quality of life, independence and safety, and the carers themes. The sub-group also considered dementia using the same approach. Logic modelling helped in coming up with a representation of desired outcomes, the resources and people involved in contributing to these outcomes. At the same time it supports focused thinking about key measures of process and outcome. The approach promotes 50 evaluation and benchmarking in examining how well intended outcomes were delivered, change in behaviour or knowledge, the extent of participation, the effectiveness of activities, and how these potentially relate back to how resources are deployed. Experience of using logic models in this limited way within the SCCBN suggests wider benefits from the approach. There are strengths in the approach related to linking issues to interventions and to outcomes which could be applied more widely in the work of SCCBN. An example of this would be work to support the development of local frameworks to report performance on Reshaping Care for Older People. 51