Emergency Protocol
advertisement
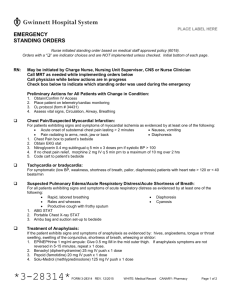
PLACE LABEL HERE
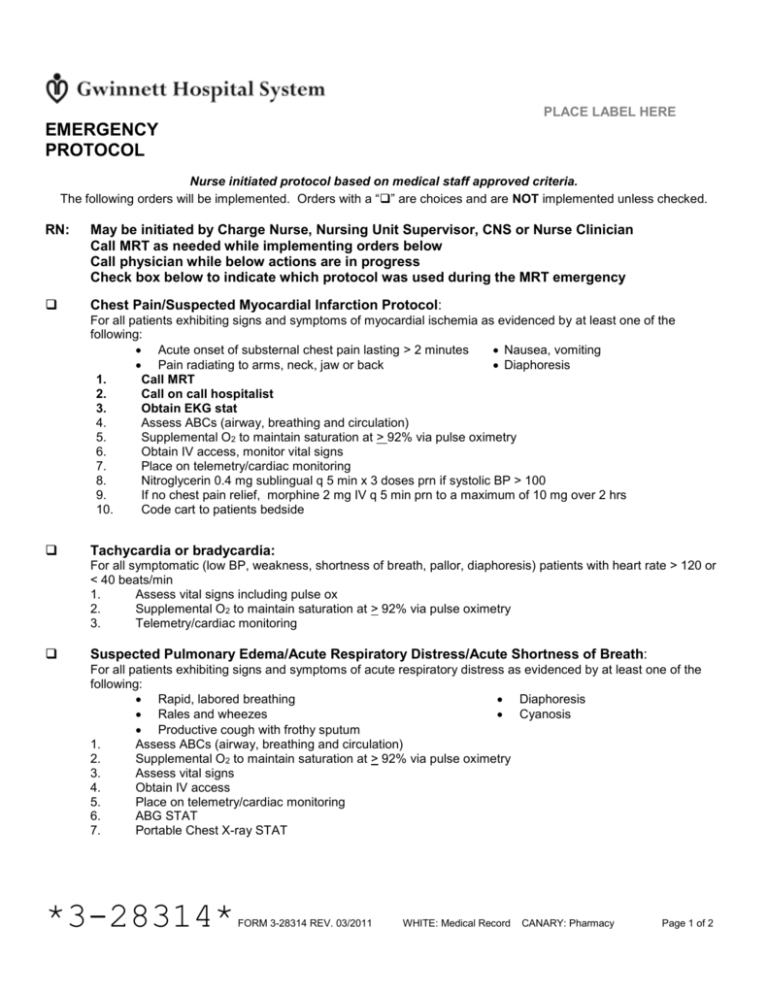
EMERGENCY
PROTOCOL
Nurse initiated protocol based on medical staff approved criteria.
The following orders will be implemented. Orders with a “” are choices and are NOT implemented unless checked.
RN:
May be initiated by Charge Nurse, Nursing Unit Supervisor, CNS or Nurse Clinician
Call MRT as needed while implementing orders below
Call physician while below actions are in progress
Check box below to indicate which protocol was used during the MRT emergency
Chest Pain/Suspected Myocardial Infarction Protocol:
For all patients exhibiting signs and symptoms of myocardial ischemia as evidenced by at least one of the
following:
Acute onset of substernal chest pain lasting > 2 minutes
Nausea, vomiting
Pain radiating to arms, neck, jaw or back
Diaphoresis
1.
Call MRT
2.
Call on call hospitalist
3.
Obtain EKG stat
4.
Assess ABCs (airway, breathing and circulation)
5.
Supplemental O2 to maintain saturation at > 92% via pulse oximetry
6.
Obtain IV access, monitor vital signs
7.
Place on telemetry/cardiac monitoring
8.
Nitroglycerin 0.4 mg sublingual q 5 min x 3 doses prn if systolic BP > 100
9.
If no chest pain relief, morphine 2 mg IV q 5 min prn to a maximum of 10 mg over 2 hrs
10.
Code cart to patients bedside
Tachycardia or bradycardia:
For all symptomatic (low BP, weakness, shortness of breath, pallor, diaphoresis) patients with heart rate > 120 or
< 40 beats/min
1.
Assess vital signs including pulse ox
2.
Supplemental O2 to maintain saturation at > 92% via pulse oximetry
3.
Telemetry/cardiac monitoring
Suspected Pulmonary Edema/Acute Respiratory Distress/Acute Shortness of Breath:
For all patients exhibiting signs and symptoms of acute respiratory distress as evidenced by at least one of the
following:
Rapid, labored breathing
Diaphoresis
Rales and wheezes
Cyanosis
Productive cough with frothy sputum
1.
Assess ABCs (airway, breathing and circulation)
2.
Supplemental O2 to maintain saturation at > 92% via pulse oximetry
3.
Assess vital signs
4.
Obtain IV access
5.
Place on telemetry/cardiac monitoring
6.
ABG STAT
7.
Portable Chest X-ray STAT
*3-28314*
FORM 3-28314 REV. 03/2011
WHITE: Medical Record
CANARY: Pharmacy
Page 1 of 2
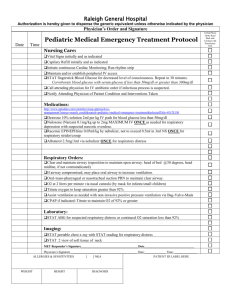
PLACE LABEL HERE
EMERGENCY
PROTOCOL
Nurse initiated protocol based on medical staff approved criteria.
The following orders will be implemented. Orders with a “” are choices and are NOT implemented unless checked.
Narcotic-Induced Respiratory Depression Protocol:
For all patients, if following administration of an opiate (narcotic) analgesic the patient exhibits signs and
symptoms of respiratory depression as evidenced by respiratory rate 8 breaths per min or apnea or agonal
respirations
1.
Assess ABCs (airway, breathing and circulation)
2.
Assist ventilation with bag valve mask and supplemental O2 if required
3.
Supplemental O2 to maintain saturation at > 92% via pulse oximetry
4.
Obtain IV access
5.
Assess vital signs
6.
Narcan (naloxone) 0.4 mg in 10 ml Normal Saline (0.04 mg/ml). Administer 1 ml IV q 2 min prn until
respiratory rate > 10 or a max of 2 mg (5 doses)
7.
If IV route is not available, administer undiluted Narcan (naloxone) 0.4 mg SQ or IM q 5 min prn until
respiratory rate > 10 or a max of 2 mg (5 doses)
8.
Call MRT If patient shows sign of respiratory instability, 2 or more doses of Narcan (naloxone)
administered, or suspected Benzodiazapine induced respiratory depression {examples include: Versed
(midazolam), Xanax (alprazolam), Ativan (lorazepam), Valium (diazepam)
Stroke Alert Protocol:
For all patients exhibiting signs and symptoms of an acute stroke as evidenced by:
Sudden numbness or weakness
Sudden dizziness/loss of balance or coordination
Sudden severe headache
Sudden confusion or trouble speaking/understanding
Sudden dimness/loss of vision
Staff nurse:
1.
Recognize stroke symptoms
2.
Establish time of symptom onset
3.
Activate “Stroke Alert” by notifying charge nurse in The Center for Neuroscience or GMC-D-ICU (see
policy #500-41)
4.
Assess vital signs
5.
Supplemental O2 to maintain saturation at > 92% via pulse oximetry
6.
Finger stick glucose STAT
Stroke Alert Nurse:
1.
Assess NIH Stroke Scale
2.
Assist with ordering tests/labs (all ordered stat): “Stroke Alert CT of head”, CP7, CBC, PT/PTT
3.
Notify Stroke Study Physician of above and provide attending physician name and phone number
4.
Transfer to Center for Neuroscience or GMC-D-ICU, if the patient is eligible for tissue plasminogen
activator (tPA), stroke study, or per physician order
5.
Call physician for Stroke Alert Tissue Plasminogen Activator (Activase) orders if a candidate (form #
16239)
Suspected/Active Bleeding Protocol:
1.
2.
Stat CBC, PT/PTT, Type and Screen
If Hgb < 7 and patient is symptomatic, type and cross 2 units of packed red blood cells
________ ________ ____________________________________________
_________________________
Date
Time
Per Protocol (# 6019)/Physician Name/Nurse Signature and/or Physician Signature & Number
FORM 3-28314 REV. 03/2011
WHITE: Medical Record
CANARY: Pharmacy
Page 2 of 2