Immunisation of Healthcare and Laboratory staff
advertisement
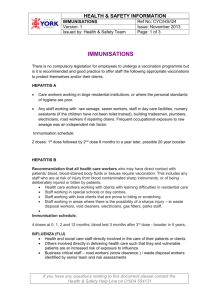
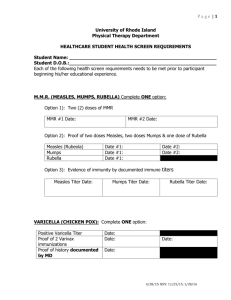
Immunisation of Healthcare and Laboratory Staff Version 3 Name of responsible (ratifying) committee Health and Safety Committee Date ratified 24.09.14. Document Manager (job title) Consultant Occupational Health Physician Date issued 07th October 2014 Review date 06th October 2014 Electronic location Health and Safety policies Related Procedural Documents Hepatitis B Virus (HBV): Protecting employees and patients. Measles, Mumps & Rubella (MMR) and Varicella (chickenpox): Occupational Health Screening and Management. Control of TB in NHS employees. Key Words (to aid with searching) Work Health Assessment; Blood borne virus; tuberculosis; BCG; hepatitis B; MMR; measles; Influenza Version Tracking Version Date Ratified Brief Summary of Changes Author 3 24.09.14 No change. Review date previous version expired. Dr S Harvey Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date 017/10/2014 (Review date: 06th October 2017 (unless requirements change) Page 1 of 9 CONTENTS Quick Reference Guide…………………………………………………………………………..page 3 Introduction………………………………………………………………………………………….page 4 Purpose……………………………………………………………………………………………..page 4 Scope…………………………………………………………………………………………………page 4 Definitions……………………………………………………………………………………………page 4-5 Duties and responsibilities………………………………………………………………………...page 5 Process………………………………………………………………………………………………page 5-7 Training requirements………………………………………………………………………………page 7 References and Associated Documentation……………………………………………………..page 7 Equality and Diversity Statement………………………………………………………………….page 7-8 Monitoring Compliance with and the effectiveness of procedural documents…………………page 9 Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 2 QUICK REFERENCE GUIDE This policy must be followed in full when developing or reviewing and amending Trust procedural documents. For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. 1. The Control of Substances Hazardous to Health (COSHH) Regulations 2002 require employers to assess the risks from exposure to hazardous substances, including pathogens (called biological agents in COSHH) and to bring into effect measures necessary to protect workers and others who may be exposed from those risks, as far as is reasonably practicable. This includes appropriate immunisation. 2. Occupational Health will identify the vaccinations required by different groups of staff and will make arrangements for these to take place. Line managers will be asked to ensure their staff attend for vaccinations where required and will be informed if their staff do not attend for vaccination and if workplace restrictions are required. 3. The four main staff groups for vaccination are: ‘staff involved in direct patient care’; ‘nonclinical staff in healthcare settings’; ‘laboratory and pathology staff’ and ‘staff handling specific organisms’. The vaccinations required for each group are set out in this policy. 4. Further specific details about each vaccination can be obtained from the individual Trust policies: ‘Hepatitis B Virus (HBV): Protecting employees and patients’; ‘Measles, Mumps & Rubella (MMR) and Varicella (chickenpox): Occupational Health Screening and Management’; ‘Control of TB in NHS employees’. 5. Influenza immunisation helps prevent influenza in staff and can reduce the transmission of influenza to vulnerable patients. At Portsmouth Hospitals NHS Trust the trivalent seasonal influenza vaccine is offered on an annual basis to healthcare workers directly involved in patient care, as well as non- clinical staff in healthcare settings, laboratory and pathology staff and staff handling specific organisms Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 3 1. INTRODUCTION The Control of Substances Hazardous to health (COSHH) Regulations 2002 require employers to assess the risks from exposure to hazardous substances, including pathogens (called biological agents in COSHH) and to bring into effect measures necessary to protect workers and others who may be exposed from those risks, as far as is reasonably practicable. Any vaccine preventable disease that is transmissible from person to person poses a risk to both health care professionals and their patients. Health care workers have a duty of care towards their patients which includes taking reasonable precautions to protect themselves from communicable diseases, including by appropriate immunisations. Immunisation of healthcare and laboratory workers may therefore be indicated to: Protect the individual and their family from an occupationally-acquired infection Protect patients and service users, including vulnerable patients who may not respond well to their own immunisation Protect other healthcare and laboratory staff Allow for the efficient running of services without disruption. The most effective method for preventing laboratory-acquired infections is the adoption of safe working practices. Immunisation should not be regarded as a substitute for good laboratory practice, although it does provide additional protection. Staff who work mainly with clinical specimens or have patient contact may be exposed to a variety of infections, while staff who mainly work with specific pathogens are only likely to be exposed to those pathogens handled in their laboratory. The health assessment for laboratory staff should take into account the local epidemiology of disease, the nature of material handled, the frequency of contact with infected or potentially infected material, the lab facilities and the nature and frequency of any patient contact. Staff considered to be at risk of exposure to pathogens should be offered pre-exposure immunisation as appropriate. 2. PURPOSE To inform Portsmouth Hospitals NHS Trust employees of the requirements and duties for workplace vaccinations. These are divided into four main groups: ‘staff involved in direct patient care’; ‘non-clinical staff in healthcare settings’; laboratory and pathology staff’ and ‘staff handling specific organisms’. 3. SCOPE The policy applies to all employees of Portsmouth Hospitals NHS Trust, including staff employed on temporary or honorary contracts. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ 4. DEFINITIONS Staff involved in direct patient care This includes staff who have regular clinical contact with patients and who are directly involved in patient care. This includes doctors, dentists, midwives, nurse, paramedics and ambulance drivers, occupational therapists, physiotherapists and radiographers. Students and trainees in these disciplines and volunteers who are working with patients must also be included. Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 4 Laboratory and pathology staff This includes laboratory and other staff (including mortuary staff) who regularly handles pathogens or potentially infected specimens. In addition to technical staff, this may include cleaners, porters, secretaries and receptionists in laboratories. Staff handling specific organisms For some infections, the probability that clinical specimens and environmental samples of UK origin contain the implicated organism, and therefore present any risk to staff, is extremely low. For these infections, routine immunisation of laboratory workers is not indicated. However those working in higher risk settings, such as reference laboratories or infectious disease hospitals may have a level of exposure sufficient to justify vaccination. For example, Hepatitis A, Japanese encephalitis, meningococcal ACW135Y, typhoid, yellow fever etc. 5. DUTIES AND RESPONSIBILITIES Directors Employers need to be able to demonstrate that an effective employee immunisation programme is in place. Occupational Health The Occupational Health and Safety Service is responsible for the management of the immunisation programme. Occupational health will inform employees of the risks to their health and others if they refuse, or are a poor or non-responder to an immunisation programme. OH will inform managers when employees do not attend for appointments, refuse vaccinations or if they are contraindicated. Managers Managers must complete Risk Identification Forms for new employees and ensure these are available to Occupational Health. Managers have responsibility to ensure that any employees for whom they have line management responsibility have had all relevant workplace vaccinations. Health Care Workers Health care Workers have a duty of care towards their patients which includes taking reasonable precautions to protect themselves from communicable diseases, including by appropriate immunisations. Immunisation must not used as a substitute for good practice in relation to the prevention of infection and general measures to prevent occupational transmission of blood-borne viruses must be followed. 6. PROCESS Work Health Assessment All new employees must undergo a Work Health Assessment which will include a review of immunisation needs. The job risk assessment form will indicate which pathogens staff are likely to be exposed to in their workplace. Staff considered to be at risk of exposure to pathogens will be offered routine pre –exposure immunisation as appropriate. Staff not considered to be at risk will not routinely be offered immunisation, although post-exposure prophylaxis may occasionally be indicated. 1. Staff involved in direct patient care This includes doctors, nurses, midwives, physiotherapists, occupational therapists and radiographers. All staff involved in direct patient care must be up to date with their routine immunisations, e.g. tetanus, diphtheria, polio and MMR (Measles, Mumps and Rubella). With regards to tetanus, diphtheria and polio, any missed immunisations or required updates must be obtained from the employee’s General Practitioner. The MMR vaccine is especially important in the context of the ability of staff to transmit measles or rubella infections to vulnerable groups. While healthcare workers may need MMR vaccination for their own benefit, they should also be immune to measles and rubella in order to assist in protecting patients. For more details please refer to the Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 5 separate Trust policy: “Measles, Mumps & Rubella (MMR) and varicella (chickenpox): Occupational Health Screening and Management”. BCG vaccine is recommended for healthcare workers who may have close contact with infectious patients. It is particularly important to test and immunize staff working in maternity and paediatric departments, and departments in which the patients are likely to be immunocompromised, e.g. transplant, oncology and HIV units. For more details on BCG vaccine and tuberculosis (TB) screening in employees please refer to the separate Trust policy “Control of tuberculosis (TB) in NHS employees” Hepatitis B vaccination is recommended for health care workers who may have direct contact with patients’ blood or blood-stained body fluids. This includes any staff who are at risk of injury from blood-contaminated sharp instruments, or of being deliberately injured or bitten by patients. For more details please refer to separate Trust policy “Hepatitis B Virus (HBV): Protecting Employees and Patients”. Varicella vaccine is recommended for susceptible healthcare workers who have direct patient contact. Those with a definite history of chickenpox or herpes zoster (shingles) can be considered protected. Health care workers with a negative or uncertain history of chickenpox or herpes zoster should be serologically tested and vaccine offered to those without immunity. For more details refer to separate trust policy “Measles, Mumps & Rubella (MMR) and varicella (chickenpox): Occupational Health Screening and Management”. Influenza immunisation helps prevent influenza in staff and may also reduce the transmission of influenza to vulnerable patients. Influenza vaccination is therefore recommended for healthcare workers directly involved in patient care, who should be offered influenza immunisation on an annual basis. 2. Non- clinical staff in healthcare settings This includes non-clinical ancillary staff who may have social contact with patients but are not directly involved in patient care. This group included receptionists, ward clerks, porters and cleaners. These staff should be up to date with their routine immunisations, e.g. tetanus, diphtheria, polio and MMR (Measles, Mumps and Rubella). With regards to tetanus, diphtheria and polio, any missed immunisations or required updates must be obtained from the employee’s General Practitioner. The MMR vaccine is especially important in the context of the ability of staff to transmit measles or rubella infections to vulnerable groups. For more details please refer to the separate Trust policy: “Measles, Mumps & Rubella (MMR) and varicella (chickenpox): Occupational Health Screening and Management”. At Portsmouth Hospitals NHS Trust, BCG vaccine is recommended for non-clinical staff in healthcare settings. For more details on BCG vaccine and tuberculosis (TB) screening in employees please refer to the separate Trust policy “Control of tuberculosis (TB) in NHS employees” Hepatitis B vaccination is recommended for workers who are at risk of injury from bloodcontaminated sharp instruments, or of being deliberately injured or bitten by patients. For more details please refer to separate Trust policy “Hepatitis B Virus (HBV): Protecting Employees and Patients”. Varicella vaccine is recommended for susceptible healthcare workers who have regular patient contact but are not necessarily involved in direct patient care. Those with a definite history of chickenpox or herpes zoster can be considered protected. Those with a negative or uncertain history should be serologically tested and vaccine offered to those without antibody. For more details refer to separate trust policy “Measles, Mumps & Rubella (MMR) and varicella (chickenpox): Occupational Health Screening and Management”. Influenza vaccine is offered to non-clinical staff at Portsmouth Hospitals NHS Trust on an annual basis. Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 6 3. Laboratory and Pathology Staff This includes laboratory and other staff (including mortuary staff) who regularly handle pathogens or potentially infected specimens. In addition to technical staff, this may include cleaners, porters, secretaries and receptionists in laboratories. All staff should be up to date with their routine immunisations, e.g. tetanus, diphtheria, polio and MMR (Measles, Mumps and Rubella). The MMR vaccine is especially important for those who have contact with patients. For more details please refer to the separate Trust policy: “Measles, Mumps & Rubella (MMR) and varicella (chickenpox): Occupational Health Screening and Management”. Staff regularly handling faecal specimens who are likely to be exposed to polio viruses should be offered a booster with a polio-containing vaccine every ten years. Individuals who may be exposed to diphtheria in microbiology laboratories and clinical infectious disease units should be tested and, if necessary, given a booster of diphtheria-containing vaccine. An antibody test should be performed at least three months after immunisation to confirm protective immunity and the individual should be given a booster at ten-year intervals thereafter. The cut-off level is 0.01 IU/ml for those in routine diagnostic laboratories. For those handling or regularly exposed to toxigenic strains, a level of 0.1 IU/ml should be achieved. When a history of full diphtheria immunisation is not available, the primary course must be completed and an antibody test should be performed at least three months later to confirm protective immunity. Boosters should be given five years later and subsequently at ten-yearly intervals. BCG is recommended for technical staff in microbiology and pathology departments, attendants in autopsy rooms and any others considered being at high risk. For more details on BCG vaccine and tuberculosis (TB) screening in employees please refer to the separate Trust policy “Control of tuberculosis (TB) in NHS employees” Hepatitis B vaccination is recommended for laboratory staff who may have direct contact with patients’ blood or blood-stained body fluids or with patients’ tissues. See separate Trust policy “Hepatitis B Virus (HBV): Protecting Employees and Patients”. 4. Staff handling specific organisms In addition to the vaccinations required for ‘laboratory and pathology staff’, staff handling specific organisms such as Hepatitis A, Japanese encephalitis, meningococcal ACW135Y, typhoid etc may need additional vaccinations. These staff will be identified through risk assessment by their line managers and referred to Occupational Health as required. 7. TRAINING REQUIREMENTS There are no specific training requirements. Staff requiring workplace vaccinations will be identified by Occupational Health as part of the Work Health Assessment process, and will be invited for vaccination. Where employees do not attend for vaccination, line managers will be informed by Occupational Health if workplace restrictions are required for specific employees. 8. REFERENCES AND ASSOCIATED DOCUMENTATION The following referencing format must be used: An Organisation-Wide Policy for the Development and Management of Procedural Documents: NHSLA, May 2007. www.nhsla.com/Publications/ Immunisation against infectious disease. The Green Book. Department of Health. 2006 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 7 This policy has been assessed accordingly Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviours our employees display in the workplace. Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do. We are committed to promoting a culture founded on these values which form the ‘heart’ of our Trust: Respect and dignity Quality of care Working together No waste This policy should be read and implemented with the Trust Values in mind at all times. Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date (Review date: 06th October 2017 (unless requirements change) 017/10/2014 8 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS This document will be monitored to ensure it is effective and to assurance compliance. The effectiveness in practice of all procedural documents should be routinely monitored (audited) to ensure the document objectives are being Minimum requirement to be monitored Lead Audit of Occupational Health screening process- Work Health Assessment of new PHT employees OH consultant physician Tool audit Frequency of Report of Compliance annual Reporting arrangements Lead(s) for acting on Recommendations Policy audit report to: Health and Safety Committee achieved. The process for how the monitoring will be performed should be included in the procedural document, using the template above. The details of the monitoring to be considered include: The aspects of the procedural document to be monitored: identify standards or key performance indicators (KPIs); The lead for ensuring the audit is undertaken The tool to be used for monitoring e.g. spot checks, observation audit, data collection; Frequency of the monitoring e.g. quarterly, annually; The reporting arrangements i.e. the committee or group who will be responsible for receiving the results and taking action as required. In most circumstances this will be the committee which ratified the document. The template for the policy audit report can be found on the Trust Intranet Trust Intranet -> Policies -> Policy Documentation The lead(s) for acting on any recommendations necessary. Immunisation of Healthcare and Laboratory Staff. Issue Number 3 Issue Date 017/10/2014 requirements change) (Review date: 06 th October 2017 (unless 9