INFECTION - NHS Tower Hamlets CCG
advertisement

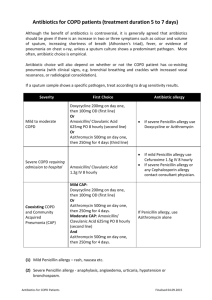
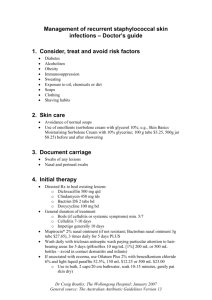
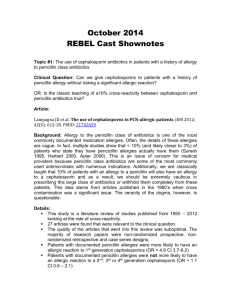
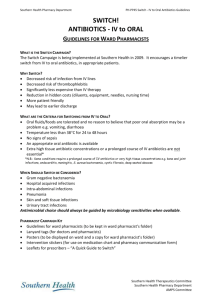
SKIN AND SOFT TISSUE RESPIRATORY TRACT INFECTION 1ST LINE PENICILLIN ALLERGY OR 2ND LINE CHOICE Community acquired pneumonia (CAP) Non–Severe : †CURB65 score 0-1 and NOT previously treated with antibiotics Community acquired pneumonia (CAP) Non–Severe : †CURB65 score 2 OR CURB65 score 0-1 AND previously treated with antibiotics Amoxicillin po 500mg tds Doxycycline po 200mg STAT then 100mg-200mg daily OR Clarithromycin po 500mg bd Community acquired pneumonia (CAP) *Severe: †CURB65 score 3 to 5 (In cases of confirmed legionella discuss with microbiology) COPD exacerbation (use a different class of antibiotic if a recent course of 1st line in the prev 3 months) Early-onset hospital acquired pneumonia (less than 5 days after admission to hospital) including aspiration pneumonia Late-onset hospital acquired pneumonia (more than 5 days after admission to hospital) OR * (Moderate - Severe) OR (if recently prescribed antibiotics or colonised with resistant organisms – speak to Microbiology) Amoxicillin po/iv 500mg – 1g tds plus Clarithromycin po/iv 500mg bd Benzylpenicillin iv 1.2g qds plus Clarithromycin iv 500mg bd OR If known COPD/Chronic lung disease/Recent course of amoxicillin Co-amoxiclav iv 1.2g tds plus Clarithromycin iv 500mg bd Amoxicillin po 500mg tds Treat as in CAP (for aspiration pneumonia add metronidazole iv 500mg tds) Piperacillin/Tazobactam (Tazocin) iv 4.5g tds +/ Amikacin iv 15mg/kg STAT dose for severe infection Doxycycline po 200mg STAT then 100mg-200mg daily OR Clarithromycin iv/po 500mg bd INITIAL DURAT ION 5-7 days 5-7 days Vancomycin iv (as per guideline) plus Clarithromycin iv 500mg bd OR Levofloxacin iv 500mg bd (For intubated or NIV patient) Doxycycline po 200mg STAT then 100mg-200mg daily OR Clarithromycin po 500mg bd Treat as in CAP (for aspiration pneumonia add metronidazole iv 500mg tds) 7-10 days 5 days Vancomycin iv (as per guideline) plus Amikacin iv od (as per guidelines) 5-7 days 5-7 days (for aspiration pneumonia add metronidazole iv 500mg tds) ♦See overleaf for definition of severe and non-severe penicillin allergy † CURB65 is the severity scoring acronym used to determine the management of CAP in patients admitted to hospital. Each risk factor scores one point: Confusion (Abbreviated Mental Test (AMT) score of 8 or less); Urea >7mmol/L; Respiratory rate ≥ 30/min; Blood pressure (SBP< 90mmHg or DBP≤ 60mmHg); Age ≥ 65yrs Please note: CURB65 is a guide and may not be applicable for all patients e.g. young patients presenting with pneumonia. This is also not relevant in patients incapable of mounting an adequate host response to infection. *Severe symptoms = a SIRS score of two or more. SIRS criteria: Temperature >38°C or <36°C; Heart rate >90 beats/min; Respiratory rate >20 breaths/min or PaCO2<4.3 kPa; WBC <4 x 109/L or >12 x 109/L or >10% immature forms. Sepsis = Suspicious or proven infection + Severe symptoms Severe Sepsis = Sepsis + acute organ failure ± hypotension Septic Shock = Severe Sepsis despite adequate fluid resus GASTROINTESTINAL TRACT INFECTION 1ST LINE PENICILLIN ALLERGY OR 2ND LINE CHOICE Cellulitis (mild-moderate) In mild, treat orally & send patient home from A&E Cellulitis moderate with signs of sepsis Cellulitis severe with signs of septic shock) exclude necrotising fasciitis Flucloxacillin po/iv 500mg-1g qds Clarithromycin po/iv 500mg bd Benzylpenicillin iv 1.2g qds plus Flucloxacillin iv 1g qds Benzylpenicillin iv 1.2g qds plus Flucloxacillin iv 1g qds plus Clindamycin iv 600mg-1.2g qds Meropenem iv 1g tds plus Clindamycin iv 1.2g qds Clindamycin po/iv 450mg qds Vancomycin iv (as per guidelines) Vancomycin iv (as per guidelines) plus Clindamycin iv 600mg-1.2g qds Vancomycin iv (as per guidelines) plus Clindamycin iv 600mg -1.2g qds Cellulitis severe involving groin/scrotal/ labial region Necrotising Fasciitis seek urgent surgery review Surgical wound Mild following clean surgery Flucloxacillin iv/po 1g qds Surgical wound Moderate to Severe following clean surgery with signs of sepsis Benzylpenicillin iv 1.2g qds plus Flucloxacillin iv 1g qds plus Clindamycin iv 1.2g qds Co-amoxiclav po 625mg tds Surgical wound Mild to Moderate following contaminated surgery Surgical wound Moderate to Severe following contaminated surgery with signs of sepsis Human/ Animal bites Diabetic Foot Ulcer TREAT MENT IF M RS A +V E Discuss sensitivities with microbiology Non-severe penicillin Vancomycin iv allergy (as per guidelines) plus (same as 1st line Meropenem iv 1g treatment) ♦Severe penicillin allergy tds plus Vancomycin iv Clindamycin iv (as per guidelines) 1.2g qds plus Clindamycin iv 1.2g qds plus Amikacin iv od (as per guidelines) Doxycycline po 200mg Vancomycin iv daily OR (as per guidelines) Vancomycin iv (as per guidelines) Vancomycin iv (as per guidelines) plus Clindamycin iv 1.2g qds INFECTION 1ST LINE PENICILLIN ALLERGY OR 2ND LINE CHOICE INITIAL DURAT ION Acute Pancreatitis Necrotising Pancreatitis No antibiotics needed No antibiotics needed N/A Meropenem iv 1g tds Non-severe allergy: Meropenem iv 1g tds 7-14 days Community acquired Intraabdominal sepsis: (includingcholecystitis, cholangitis, appendicitis, diverticulitis) Post-surgical intraabdominal infection (deep space) Non-severe: Co-amoxiclav iv 1.2g tds * Severe: Piperacillin/Tazobactam (Tazocin) iv 4.5g tds plus Amikacin iv od (as per guidelines) If no previous treatment course of antibiotics: Co-amoxiclav iv 1.2g tds If previous treatment course of antibiotics: Piperacillin/Tazobactam (Tazocin) iv 4.5g tds If septic plus Amikacin iv od (as per guidelines) Same as second-line treatment Clindamycin po 450mg Same as qds plus second-line Amikacin iv od 2 doses treatment only (as per guidelines) Co-amoxiclav iv 1.2g tds Clindamycin iv 600mgAdd plus Amikacin iv od 1.2g qds plus Vancomycin iv Ciprofloxacin iv 400mg bd (as per guidelines) to regimen plus Amikacin iv od (as per guidelines) (as per guidelines) Co-amoxiclav po Doxycycline po 200mg Same as second625mg tds STAT then 100 daily line treatment – plus Metronidazole po check sensitivity 400mg tds Refer to separate guidelines Spontaneous Bacterial Peritonitis (SBP) Piperacillin/Tazobactam (Tazocin) iv 4.5g tds If septic plus Amikacin iv (as per guidelines) Metronidazole po 400mg tds Clostridium difficile (mild / moderate) ♦Severe penicillin allergy Clindamycin iv 1.2g qds plus Amikacin iv od (as per guidelines) Ciprofloxacin iv 400mg bd plus Metronidazole iv 500mg tds plus Amikacin iv od (as per guidelines) If no previous course of antibiotics in Non-severe penicillin allergy Ceftriaxone iv 2g od plus Metronidazole iv 500mg tds If previous treatment course of antibiotics OR ♦Severe penicillin allergy Ciprofloxacin iv 400mg bd plus Metronidazole iv 500mg tds plus Amikacin iv od (as per guidelines) Non-severe penicillin allergy Ceftriaxone iv 2g od ♦Severe penicillin allergy Discuss with micro Vancomycin po 125mg qds If signs of necrotising fasciitis, immediately seek urgent surgical review MUSCULOSKELETAL SYSTEM Septic arthritis (immunocompetent patients only) Acute osteomyelitis (immunocompetent patients only) Chronic Osteomyelitis/ infected implants Flucloxacillin iv 2g qds plus Sodium fusidate po 500mg tds for initial 2 weeks Clindamycin iv 600mg qds plus Sodium fusidate po 500mg tds for initial 2 weeks Vancomycin iv (as per guidelines) plus Sodium fusidate po 500mg tds (confirm sensitivities for fusidate) Manage with Orthopaedics and Microbiology INTRAVENOUS LINES For peripheral line infections - remove line immediately. -Re-site if still necessary Flucloxacillin iv Vancomycin iv Vancomycin iv Peripheral line Moderate to severe with signs (as per guidelines) plus 1-2g qds (as per guidelines) of sepsis Sodium fusidate po 500mg tds (confirm sensitivities for fusidate) Prompt assessment of line & discussion of risk/benefit line removal with micro Central line See separate guidelines TPN lines Durations for Peripheral line infections: 5-10 days 10-14 days 10 days URINARY TRACT INFECTION 1ST LINE PENICILLIN ALLERGY OR 2ND LINE CHOICE ‡ Nitrofurantoin po 50-100mg qds for 3 days (Treat for 7 days in men) Community acquired Lower UTI (No catheter) Trimethoprim po 200mg bd for 3 days (Treat for 7 days in men) ‡ Caution: Failure may occur with CrCl<45mL per min Avoid if CrCl <30mL per min Cephalexin po 500mg tds for 7 days Community acquired Lower UTI in Pregnant women Trimethoprim 200mg bd for 7 days (avoid 1st trimester) OR ‡ Nitrofuratoin po 50-100mg qds for 7 days (avoid in 3rd trimester) ‡ Caution: Failure may occur with CrCl<45mL per min Avoid if CrCl <30mL per min Ciprofloxacin po 500mg bd plus Amikacin iv 15mg/kg STAT Durations: Septic arthritis and Acute osteomyelitis 4-6wks (min 2wks iv except for sodium fusidate) Caution: Clindamycin is associated with antibiotic-associated colitis –stop if diarrhoea occurs Minimum 7 days (See separate UTI guideline in addition on intranet ) Durations for SSTIs : 7-10 days depending on severity and response Caution: Clindamycin is associated with antibiotic-associated colitis –stop if diarrhoea occurs Review after 5 days Community acquired Pyelonephritis Hospital acquired UTIs Catheter associated UTIs Co-amoxiclav iv 1.2g tds plus Amikacin iv 15mg/kg STAT (switch from IV to oral when clinically appropriate) Treat for 10-14days Treat for 10-14days Firstly check past microbiology results – please refer to separate UTI guideline do not treat unless systemically unwell GENITOURINARY TRACT See separate guidelines CENTRAL NERVOUS SYSTEM INFECTION 1ST LINE Meningitis Ceftriaxone iv 2g bd If pregnant, elderly or immunocompromised add Amoxicillin iv 2g 4hrly Non-severe penicillin allergy Ceftriaxone iv 2g bd If pregnant, elderly or immunocompromised discuss with Microbiology (plus Aciclovir iv 10mg/kg tds if encephalitic) (plus Aciclovir iv 10mg/kg tds if encephalitic) ♦Severe penicillin allergy Chloramphenicol iv 25mg/kg 6hrly (plus Aciclovir iv 10mg/kg tds if encephalitic) Meningitis & Corticosteroid therapy: Consider the use of dexamethasone in adolescents and adults with suspected Streptococcus pneumoniae meningitis. Administer before or with the first dose of antibiotic: IV dexamethasone 0.15mg/kg 6hourly for 4 days (Avoid in septic shock, meningococcal septicaemia, immunocompromised patients and meningitis post surgery. Durations of treatment for meningitis: variable depending on causative organism – please see separate guideline Encephalitis Aciclovir iv 10mg/kg tds o Patient’s allergy status MUST always be checked prior to prescribing and administering antibiotics o The exact nature, severity and time of onset of any reported allergy should be ascertained. A distinction should be made between intolerance, e.g. diarrhoea, nausea and vomiting, and ‘true’ immune-mediated allergy. o For all true antibiotic allergy, it is important to differentiate between immediate (type I) and delayed hypersensitivity reactions – please see table below. o Nursing staff must contact the medical team immediately if the patient develops any signs or symptoms of an allergic reaction. o Penicillins (coded red) are contra-indicated in all patients with a true penicillin allergy – mild or severe reaction. o Non-penicillin beta-lactams (coded orange) should be avoided in patients with severe reactions to penicillins (immediate or delayed). o Non-penicillin non-beta-lactams (coded green) are safe to use in all forms of penicillin allergy. o See full penicillin policy for further details. Characteristics of Immediate (Type I) Delayed antibiotic allergy Time interval after drug administration Clinical signs: Severe SEPTICAEMIA of unknown origin Severe Sepsis Piperacillin/Tazobactam (Tazocin) iv 4.5g tds plus Amikacin iv od (as per guidelines) Non-severe allergy: Meropenem iv 1g tds ♦Severe penicillin allergy: Vancomycin iv (as per guidelines) plus Amikacin iv od (as per guidelines) plus Metronidazole Clinical signs: Mild < 4hrs (rarely up to 72hrs) Anaphylaxis(Airway obstruction and/or Hypotension) Angioedema (swelling) Generalised urticaria (hives) Diffuse erythema (redness) Minor rash CARDIOVASCULAR See separate guidelines for endocarditis OTHER INFECTION Conjunctivitis Oral Candidiasis Postsplenectomy prophylaxis 1ST LINE Chloramphenicol eye ointment qds Fluconazole po 50mg od Amoxicillin po 500mg od plus Vaccines (see intranet) PENICILLIN ALLERGY OR 2ND LINE CHOICE DURAT ION Chloramphenicol eye drops 2-6 hrly dependant on severity Nystatin liquid po 1ml qds 48 hrs after resolution Clarithromycin po 500mg od plus Vaccines (see intranet) Life-long 7 days GENERAL ANTIMICROBIAL RULES 1. Intravenous v Oral Antibiotics 3. 14 days 28 days 7 days 14 days CrCl (ml/min) >110 90 – 110 75- 89 51 – 74 40-50 30-39 20-29 10-20 Restricted Antimicrobial List These are only to be prescribed under the direction of Medical Microbiology unless they are used as part of a Trust agreed protocol/guideline. Antibiotics & Antifungals Aztreonam, Colistin, Ertapenem, Imipenem, Linezolid, Meropenem, Synercid, Teicoplanin, Temocillin, Tigecycline, Tobramycin, Caspofungin, Lipid based amphotericin (Ambisome®), Posaconazole, Micafungin, Voriconazole ~~~Clostridium difficile and Antibiotics~~ To reduce the risk factors for Clostridium difficile disease ALL antibiotics should be avoided wherever possible, especially those in the classes of cephalosporins and fluoroquinolones Minor rash Contact dermatitis Maculopapular rash Morbilliform rash Drug fever Vancomycin IV dosing (see full fileshare guidelines) Duration of Antibiotics for Bacteraemia Staphylococcus aureus bacteraemia (no endocarditis) Source removed : Source unknown or non-removable: Enterobacteriaceae bacteraemia (e.g. E.coli, Klebsiella) Source removed: Source unknown or non-removable: Steven Johnson Syndrome Toxic Epidermal Necrolysis Give a loading dose followed by a maintenance dose Loading dose based on weight only. No adjustment for age or renal function. Check age and renal function to calculate maintenance dose. Elderly patients (>65yrs old) should be dosed with a maximum starting maintenance dose of 500mg BD despite normal serum creatinine. Take vancomycin level twice a week if normal renal function. Take level and give dose unless suspicion of toxicity. For renal impairment see full guideline. Target level = 10-15mg/L or 15-20mg/L for serious, deep-seated infections, MRSA pneumonia or infections with less sensitive strains of MRSA If levels are out of range, please adjust dose accordingly – see full guidelines Weight (actual body weight) Loading dose Vancomycin Loading dose (LD) calculator Less than 60kg 60 to 90kg More than 90kg 1g 1.5g Vancomycin maintenance dose (MD) Vancomycin Start time Maintenance after LD Dose (MD) 1.5g BD 12hrs 1.25g BD 12hrs 1g BD 12hrs 750mg BD 12hrs 500mg BD 12hrs 750mg OD 24hrs 500mg OD 24hrs 500mg every 48 hrs 48hrs 2g Timing of 1st vancomycin level (based on CrCl) Before 3rd MD Before 2nd MD Before 1st MD Amikacin IV dosing (see full fileshare guidelines) P Poocckkeett ssuum mm maarryy vveerrssiioonn ooff A Adduulltt E Em mppiirriicc A Annttiibbiioottiicc TTrreeaattm meenntt G Guuiiddeelliinnee JJaannuuaarryy 22001144 > 72hrs 1. IV antibiotics should only be initiated in patients with severe symptoms or where no equivalent oral antibiotics are available or where the oral administration is contraindicated/compromised. 2. IV to oral switch should be considered in a patient who has shown clear evidence of improvement with the following features: a) Resolution of fever for >24hrs b) Pulse rate <100 beats/min c) Absence of hypoxia d) Improving white cell count e) Resolution of tachypnoea f) Resolution of hypotension g) Taking oral fluids h) Non-bacteraemic infection i) Gastrointestinal absorption 2. ALLERGY INFORMATION PENICILLIN ALLERGY OR 2ND LINE CHOICE Check age, weight and renal function to calculate dose Use IBW if patient if >20% obese, if >40% obese see full guidelines If <65yrs AND CrCl >50ml/min, dose=15mg/kg every 24hrs (max 1.5g/day) If > 65yrs or renal impairment, refer to full guidelines. Give the first dose when clinically indicated. Give second dose and subsequent doses 24hrs apart. Take trough level before the THIRD dose if no renal impairment. Do not delay the third dose while waiting for level, unless suspicion of amikacin toxicity. Target level = <5mg/L If levels are out of range, please adjust dose accordingly – see full guidelines Prescribing Standards 1. 2. Follow prescribing guidelines Specify clinical Indication for antibiotics in medical notes and drug chart (unless clinically inappropriate) Specify duration in medical notes and on drug chart Only use IV antibiotics where clinically indicated or oral route compromised 3. 4. Date 01/09 Drug Amoxicillin Route PO 1 09:00 500mg 14:00 500mg 22:00 500mg Indication COPD exacerbation Duration 5 days 2 3 4 5 IMPORTANT: Always review treatment in light of microbiology results if available. Consider the possibility of resistant organisms, e.g. MRSA and ESBL, especially if recurrent admissions/recent antibiotic therapy. For Outpatient Parenteral Antibiotic Treatment (OPAT) Contact: 07507-894-927 (for Tower Hamlets pts only) For further antimicrobial guidance please contact: Medical Microbiology SpR via switchboard Antimicrobial Pharmacists: RLH on 14-60135 or bleep 0893 NGH Bleep 026 (via switchboard 0207-476-4000) WXH Bleep: 528 (via switchboard 0208-539-5522) For antibiotic allergy testing, where appropriate, please fax referral to: Consultant Allergists on 16-2279 or, if urgent, call Allergy CNS on 07720 948385 Leaflet produced by Ms Lisa Boateng (Antimicrobial Pharmacist) Updated January 2014 with the Barts Health Antimicrobial Review Group Allergy information produced with Dr Runa Ali, Consultant Allergist