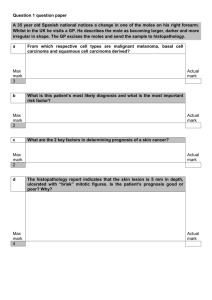
eprint_1_4118_1366
advertisement
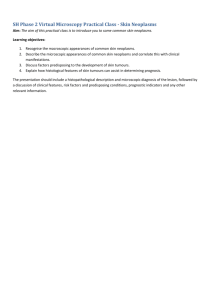
Squamous Cell Carcinoma Squamous cell carcinoma is a common tumor arising on sun-exposed sites in older people. Except for lesions on the lower legs, these tumors have a higher incidence in men than in women. In addition to sunlight, predisposing factors include industrial carcinogens (tars and oils), chronic ulcers, old burn scars, ingestion of arsenicals, and ionizing radiation. Pathogenesis. The most common exogenous cause of cutaneous squamous cell carcinoma is UV light exposure, with subsequent unrepaired DNA damage. Individuals who are immunosuppressed as a result of chemotherapy or organ transplantation, or who have xeroderma pigmentosum, are at increased risk. In addition to inducing mutations, UV light (UVB in particular) may have a transient immunosuppressive effect on skin by impairing antigen presentation by Langerhans cells.This may contribute to tumorigenesis by weakening immunosurveillance. Immunosuppressed patients, particularly organ transplant recipients, are likely to be associated with high-risk HPV types. p53 mutations with associated UV mutation signatures are common, as are activating mutations in RAS. As with squamous cell carcinomas at other sites, those in the skin may be precedeby in situ lesions. Morphology Squamous cell carcinoma in situ is characterized by highly atypical cells at all levels of the epidermis, with nuclearc crowding and disorganization. The squamous dyplasia is broad and occupies the full thickness of the epithelium.When these cells break through the basement membrane, the process has become invasive . lnvasive squamous cell carcinomas exhibit variabled differentiationr. ranging from tumors formed by atypical squamous cells arranged in orderly lobules showing large zones of keratinization to neoplasms formed by highly anaplastic, rounded cells with foci of necrosis and only abortive, single.cell keratinization(dyskeratosis) 1 Clinical Features. Squamous cell carcinomas in situ appear as sharply defined, red, scaling plaques; many arise from prior actinic keratoses. More advanced, invasive lesions are nodular, show variable scale, and may ulcerate . The likelihood of metastasis is related to the thickness of the lesion and degree of invasion into the subcutis Invasive souamous cell carcinomas of the skin are often discoveied while small and resectable; less than 5%o have metastases to regional nodes at diagnosis Basal Cell Carcinoma Basal cell carcinoma, the most common human cancer, is a slow-growing tumor that rarely metastasizes. It tend to occur at sites subject to chronic sun exposure and in lightly pigmented people. As with squamous cell carcinoma, the incidence of basal cell carcinoma increases with immunosuppression (though not as dramatically as that of squamous cell carcinoma) and in individuals with inherited defects in DNA repair. Pathogenesis Basal cell carcinoma has been associated with dysregulation of the sonic hedgehog, or PTCH, pathway. Inherited defects in the PTCH gene with subsequent loss of heterozygosity in the numerous individual tumor foci cause the familial basal cell carcinoma syndrome, Gorlin syndrome. Thus, PTCH functions as a classic tumor suppressor Morphology Tumor cells resemble the normal epidermal basal cell layer from which they are derived. Because they arise from the epidermis or sometimes follicular epithelium, they are not encountered on mucosal surfaces. Two common patterns are seen: either multifocal growths originating from the epidermis (superficial type), or nodular lesions growing downward into the dermis as cords and islands of variably basophilic cells with hyperchromatic nuclei, embedded in a fibrotic to mucinous matrix . Peripheral tumor cell nuclei align in the outermost layer (palisading) with separation from the stroma, creating a cleft or separation artifact 2 Clinical Features. Clinically, these tumors present as pearly papules, often containing prominent, dilated subepidermal blood vessels (telangiectasia) . Some tumors contain melanin pigment and thus appear similar to melanocytic nevi or melanomas. Advanced lesions may ulcerate, and extensive local invasion of bone or facial sinuses may occur after many years if neglected Melanoma is less common but much more deadly than basal or squamous cell carcinoma. Today, as a result of increased public awareness of the earliest signs of skin melanomas, most melanomas arc cured surgically Pathogenesis As with other cutaneous malignancies,sunlight plays an important role in the development of melanoma. The incidence is highest in sun-exposed skin and in geographic locales such as New Zealand and Australia where sun exposure is high and the protective mantle of melanin is sparse. Intense intermittent exposure at an early age is particularly harmful. Sunlight, however, does not seem to be the only predisposing factor; the presence of preexisting nevi and hereditary predisposition also play a role. Morphology Individual melanoma cells are usually considerably larger than nevus cells. They contain large nuclei with irregular contours having chromatin characteristically clumped at the periphery of the nuclear membrane and prominent eosinophilic nucleoli often described as "cherry red" Malignant cells grow as poorly formed nests or individual cells at all levels of the epidermis and as dermal expansile, balloon-like nodules Clinical Features. Although most of these lesionsClinically, melanoma of the skin is usually asymptomatic, although itching may be an early manifestation.The most important clinical sign of the disease is a change in the color or size of a 3 pigmented lesion. Unlike benign nevi, melanomas exhibit striking variations in pigmentation, appearing in shades of black, brown, red, dark blue, and gray . The borders of melanomas are irregular and often "notched." The main clinical warning signs of melanoma are (1) enlargement of a preexisting mole, (2) itching or pain in a preexisting pigmented lesion, and (5) variegation of color within a pigmented lesion. These principles are expressed in the so-called ABCs of ,melanoma: asymmetry, border, color, diameter, and evolution (change of an existing nevus). It is vitally important to recognize and intervene in melanoma as rapidly as possible. The vast majority of superficial lesions are,cured surgically while melanomas that become metastatic have a virtually uniformly poor prognosis, with no effective therapy in most cases. 4