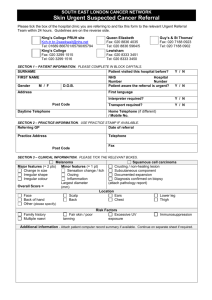
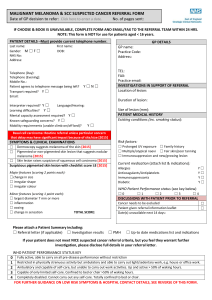
Skin Urgent Suspected Cancer Referral

SOUTH EAST LONDON CANCER NETWORK
Skin Urgent Suspected Cancer Referral
Please tick the box of the hospital clinic you are referring to and fax this form to the relevant Urgent Referral
Team within 24 hours. Guidelines are on the reverse side.
Princess Royal
Fax: 01689 863187
Tel: 01689 865676
King’s College
Fax: 020 3299 1515
Tel: 020 3299 1516
Queen Elizabeth
Fax: 020 8836 4035
Tel: 020 8836 5964/5
Lewisham
Fax: 020 8333 3451
Tel: 020 8333 3450
SECTION 1
– PATIENT INFORMATION. PLEASE COMPLETE IN BLOCK CAPITALS.
Guy’s & St Thomas’
Fax: 020 7188 0923
Tel: 020 7188 0902
SURNAME Patient visited this hospital before? Y / N
FIRST NAME
Gender M / F D.O.B.
NHS
Number
Hospital
Number
Patient aware the referral is urgent? Y / N
Address First language
Interpreter required? Y / N
Post Code Transport required? Y / N
Daytime Telephone Home Telephone (if different)
/ Mobile No.
SECTION 2
– PRACTICE INFORMATION. USE PRACTICE STAMP IF AVAILABLE.
Date of referral Referring GP
Practice Address Telephone
Fax
Post Code
SECTION 3
– CLINICAL INFORMATION. PLEASE TICK THE RELEVANT BOXES.
Major features (= 2 pts)
Change in size
Irregular shape
Irregular colour
Overall Score =
Face
Melanoma
Back of hand
Other (please specify)
Minor features (= 1 pt)
Sensation change / itch
Oozing
Inflammation
Largest diameter
(mm)
Scalp
Back
Location
Ears
Chest
Squamous cell carcinoma
Crusting / non-healing lesion
Subcutaneous component
Documented expansion
Diagnosis confirmed on biopsy
(attach pathology report)
Lower leg
Thigh
Family history
Multiple naevi
Fair skin / poor tanning
Risk Factors
Excessive UV exposure
Immunosuppression
Additional information - Attach patient computer record summary if available. Continue on separate sheet if required.
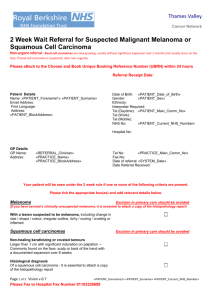
SOUTH EAST LONDON CANCER NETWORK
Information to support Skin referrals
Refer urgently patients:
With a lesion suspected to be melanoma (excision in primary care should be avoided).
Where squamous cell carcinoma is suspected – they are non-healing keratinizing or crusted tumours larger than 1cm with significant induration on palpation. They are commonly found on the face, scalp or back of the hand, with a documented expansion over 8 weeks.
Who have had an organ transplant and develop new or growing cutaneous lesions as squamous cell carcinoma is common with immunosuppression but may be atypical and aggressive.
With histological diagnosis of squamous cell carcinoma.
Use this proforma to refer urgently (2 Week Wait)
Refer non-urgently patients:
Where basal cell carcinoma is suspected – they are slow growing, usually without significant expansion over 2 months, and usually occur on the face.
Use Choose & Book or a letter to refer non-urgently
Investigations in Primary Care:
Melanoma assessment:
Change is a key element in diagnosing malignant melanoma. For low-suspicion lesions, undertake careful monitoring for change using the 7-point checklist (see below) for 8 weeks. Make measurements with photographs and a marker scale and/or rule.
Be aware of and use the 7-point weighted checklist for assessment of pigmented skin lesions o Major features: change in size; irregular shape; irregular colour o Minor features: largest diameter 7mm or more; inflammation; oozing; change in sensation
Lesions scoring 3 points or more (based on major features scoring 2 points each and minor features scoring 1 point each) in the 7-point checklist above are suspicious. (If you strongly suspect cancer any one feature is adequate to prompt urgent referral.)
Investigations:
All pigmented lesions that are not viewed as suspicious of melanoma but are excised should have a lateral excision margin of 2mm of clinically normal skin and cut to include subcutaneous fat in depth.
Send all excised skin specimens for pathological examination.
When referring a patient in whom an excised lesion has been diagnosed as malignant, send a copy of the pathology report with the referral correspondence.
Primary Care physicians undertaking minor surgery should have received appropriate accredited training in relevant aspects of skin surgery, and should undertake appropriate continuing professional development.
Approved by the South East London Cancer Network in November 2006.
For comments, additional copies, or patient information resources for GPs to use contact the Network on Tel 020 7188 7090 /
Fax 020 7188 7120, or visit our website: www.selcn.nhs.uk
.