Headaches
advertisement

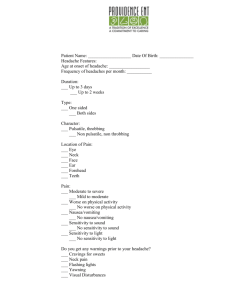
Headaches Headaches are a very common complaint in our patient population. Occurs in up to 90% of school-aged children by 18 years old. 20% of children 4-18 y/o report having had frequent or severe headaches in the past 12 months. Case: a 15 y/o female presents for WCC today. The only concern from mother is that her daughter is complaining of frequent headaches. What questions do you have for her? What physical exam maneuvers will you perform? Important aspects of the History: Current symptoms: o Age of onset o Mode of onset: sudden? o Pattern o Frequency o Aura or prodrome o Quality o Location o What makes it better/worse o Wake up in the night (early Am is more specific for mass) Associated symptoms: photophobia, phonophobia, nausea, emesis, dizziness, flushing Symptoms between headaches Headache burden (missing activities, school, etc) Change in vision, weight, sleep Past head injuries Meds tried, frequency PMHx including medications & mental health Family hx- don’t just ask if there is a family hx of migraines o Headaches o Neurological disorders (Fibromyalgia) o Mental health disorders (depression, anxiety) o IBS? Important Aspects of Physical: Vitals signs including BP & HR Complete neurological exam including optic fundi, vision & visual fields CV- murmurs Skin- neurocutaneous disorders Spine- evaluation for occult dysraphism, palpation along spinous processes for tenderness, turtle move (evals c1/2 & c3-7) 1 Red Flags: Progressive pattern of headache: becoming more severe and/or more frequent New or different severe headache, change in clinical features Increased headache with straining, coughing, or sneezing Explosive or sudden onset of severe headache (< 6 months duration) Sleep-related headache: headache waking the patient from sleep (especially just before sunrise) or headache always present in the morning Systemic symptoms: fever, weight loss, rash, joint pain Secondary risk factors: immunosuppression, hypercoagulable state, neurocutaneous disorder, cancer, genetic disorder, rheumatologic disorder Neurological symptoms/signs: altered mental status, papilledema, abnormal eye movements, or other neurological abnormalities Etiology: Common Causes: 1. 2. 3. 4. 5. 6. 7. Infection: Virus or upper respiratory infection, sinusitis, strep throat, meningitis Stress related or worsened Head injury Migraine Cluster Tension Medication overuse (Reported in 20-36% of adolescents with daily headaches) Less frequent causes: 1. 2. 3. 4. 5. 6. 7. Space occupying lesion Medications- SSRI’s, SNRI’s, OCP’s, glucocorticoids HTN Idiopathic intracranial HTN Hydrocephalus Intracranial hemorrhage Chronic Meningitis Chronic headache Evaluations: See American Academy of Neurology recommendations & American College of Radiology Appropriateness Criteria attached. Routine laboratory & imaging studies are not indicated o Neuroimaging of children with headaches in the absence of neurological abnormalities on exam and/or symptoms of neurologic abnormalities on history has a low yield of clinically significant findings = 0.0-1.2%2. Neuroimaging should be considered in the following situations (AAN recommendations): 1. Abnormal neurological examination or other findings that suggest CNS disease 2. Other factors predictive of space occupying lesion: 2 a. b. c. d. Headache <1 month Absence of family history of migraines Gait abnormalities Seizures Chronic Daily Headache: Present for >15 days/month for at least 3 months in the absence of detectable organic pathology Prevalence: 1.5% 4 subtypes of daily headaches based on International Headache Society: o Chronic Migraine o Chronic Tension-type o New Daily persistent o Hemicrania Continua Migraines: Most common acute & recurrent headache syndrome in children. Prevalence increases from 3% (age 3 to 7 years) to 4-11% (7-11 years) to 8-23% (11-15+) More common in females 3 4 Types of Migraines: Migraine with Aura (formerly know as classic migraine): o Aura is present before headache- neurological deficit or disturbance, can be: Ophthalmic Hemiparesthetic Hemiparetic Hemiplegic Aphasic o Familial Hemiplegic Migraine: Migraine with aura that includes motor weakness in a patient that has at least one first or second degree relative who has migraine with aura that includes motor weakness o Sporadic Hemiplegic Migraine: Migraine with aura that includes motor weakness in a patient without relative with same migraine Migraine without Aura (formerly known as common migraine): o Patients typically have a prodrome consisting of pallor, alteration in personality, or change in appetite or thirst o Prodrome may proceed headache by several hours Retinal Migraine: rare o Sudden loss of vision or the perception of bright light or scintillations in one eye followed within one hour by a migrainous headache. o Can occur without the headache o Vision usually returns, but permanent visual loss can occur. Basilar Type Migraine: o More common in adolescents than younger children, but can starts young Average age of onset = 7 y/o One study found children as young as 12-18 months o Affects 3-19% of children with migraines o Occipital headaches, combination of: Dysarthria Vertigo Diplopia Tinnitis Decreased hearing Ataxia Altered consciousness Simultaneous visual disturbances in both nasal/temporal fields Simultaneous bilateral paresthesias Migraine Variants: o Alice in Wonderland syndrome: headaches preceded or accompanied by visual hallucinations, bizarre perceptual distortions, or impairment of time sense o Confusional Migraine: Migraine associated with agitation, disorientation, and aphasia that last longer than the headache o Hemisyndrome Migraine: hemiparesis associated with migraine, but can be other hemisensory symptoms. 5 o Non-headache symptoms precede headache by 30-60 min & may persist after the headache resolves for hours Migraine Evaluation: Consider CBC, CMP, TSH/T4, ANA if indicated to evaluate for underlying medical conditions (See AAN recommendations above) Refer to headache specialist for: o Abnormal neuro exam o Transformation to chronic daily headache (>15days/month) o Not responding to care o Child being home schooled secondary to headaches o Uncertain diagnosis Migraine Treatment: SMART headache management: acronym to remember behavioral changes o S: sleep- same schedule, 8-10hrs at night o M: meals- don’t skip meals Limit caffeine (max 12oz/day, goal is 0) Drink water (40-60oz/day) o A: activity-regular exercise (3x/wk) o R: relaxation o T: trigger avoidance Food: cheeses, chocolate, lunchmeats, citrus, food additives etc Stress Limit medications (no more than 2x/wk- can cause overuse headache) Abortive Medications: o Ibuprofen: 10mg/kg is safe & effective, better relief of headaches as compared to placebo & Tylenol o Tylenol: 10-15mg/kg o Naproxen: 5-10mg/kg or max 500mg BID o Triptans: off label Contraindications: hx of stroke or TIA’s in family or patient, ischemic heart disease, peripheral vascular disease, uncontrolled HTN, use within 24hrs of ergotamine, concurrent administration with another 5-hT1 agonist or MAO, management of hemiplegic or basilar migraine Sumatriptan + naproxen: recent study in Pediatrics showed combination was statistically improved outcome as compared to placebo in adolescents Most effective are: nasal sumatriptan & nasal zolmitriptan, but not as well tolerated o Antiemetics: may relieve nausea & emesis Preventative treatments: 6 o Initiate at lowest effective dose, increase slowly until clinical benefits without side effects o Give adequate trial 2-3 months o Avoid interfering medications o Provide plenty of patient education, use of diaries o Re-evaluations- consider tapering when stable for 6 months o Medications: B-Blockers: Propanolol, nadolol, atenolol, metoprolol Clonidine (contraindicated in Asthma) Antidepressants: Amitriptyline, nortripyline, fluoxetine, imipramine (less common) Anticonvulstants: Depakote (Valproic acid), Keppra (Levetiracetam), Neurontin (Gabapentin), Topamax (Topiramate) Others: Riboflavin 50-400mg, Magnessium oxide (9mg/kg divided TID) 250mg BID, Coenzyme Q 100mg, Cyproheptadine (.251.5mg/kg/day) Complications of Migraines: o o o o o Chronic migraine Status migrainosus Persistent aura without infarction Migrainous infarction Migraine triggered seizure Cluster Headaches: Deep, continuous, explosive Severe, debilitating headaches of short duration (15 min-3 hrs) Commonly cause eye redness & tear production on side of headache, rhinorrhea or nasal congestions, sweating, pale appearance, drooping of the eyelid Appear repeatedly for weeks to months at a time Rare <10 y/o (0.1% of headaches in 10-18 year olds) Tension Headache: Pressing tightness, located over the forehead (or band around head). Mild to moderate, no throbbing Lasts 30 minutes to several days Not made worse with daily activities Medication Overuse Headache: AKA: Analgesic rebound headache, drug-induced headache, medication-misuse headache 7 Causative agents: Opiates > butalbital containing combination analgesics > aspirin/acetaminophen/caffeine combinations > NSAIDS Often preceded by another episodic headache disorder that has been treated with excessive amounts of acute symptomatic medications Most often daily, more often upon awakening, improved with medication use Use of analgesic > 2-3x/week in association with chronic daily headache (>15 days/month) Criteria for diagnosis: o Headache x 15 days o Regular overuse for more than 3 months of one of the more acute/symptomatic treatment drugs Ergotamine, triptans, or combination analgesic medications >10 days a month x 3 months Simple analgesic or combination of ergotamine, triptans, analgesic opioids >15 days a month x 3 months without overuse of any single class alone o Headache has developed or worsened during medication use Apps: Headache Diary App: iHeadache (Free) Med helper pill reminder (Free) Special thanks to Dr. Gerhart for providing me with additional information about migraines Resources: • The American Committee for Headache Education (www.achenet.org/) provides information and resources for patients and providers. • The American Headache Society (www.americanheadachesociety.org/) provides resources for clinicians. • The National Headache Foundation (www.headaches.org) provides information and resources for patients and providers. References: 1. Blume, HK. Pediatric Headache: A Review. Pediatrics in Review 2012; 33 (12): 562-576. 2. Bonthius, DJ. Approach to the child with headache. In: UpToDate, Drutz, JE (Ed), UpToDate, Waltham, MA, 2012. 3. Cruse, RP. Classification of Migraine in Children. In: UpToDate, Patterson MC (Ed), UpToDate, Waltham, MA, 2012. 4. Cruse, RP. Management of Migraine headache in Children. In: UpToDate, Patterson MC (Ed), UpToDate, Waltham, MA, 2013. 8 5. Derosier FJ, Lewis D, Hershey AD, Winner PK, Pearlman E, Rothner AD, et al. Randomized Trial of Sumatriptan and Naproxen Sodium Combination in Adolescent Migraine. Pediatrics 2012; 129 (6): e1411-e1420. 6. Garza, I. Medication Overuse headache: etiology, clinical features, and diagnosis. In: UpToDate, Swanson JW (Ed), UpToDate, Waltham, MA, 2013. 9