RegionalRSIProgramElements012006
advertisement
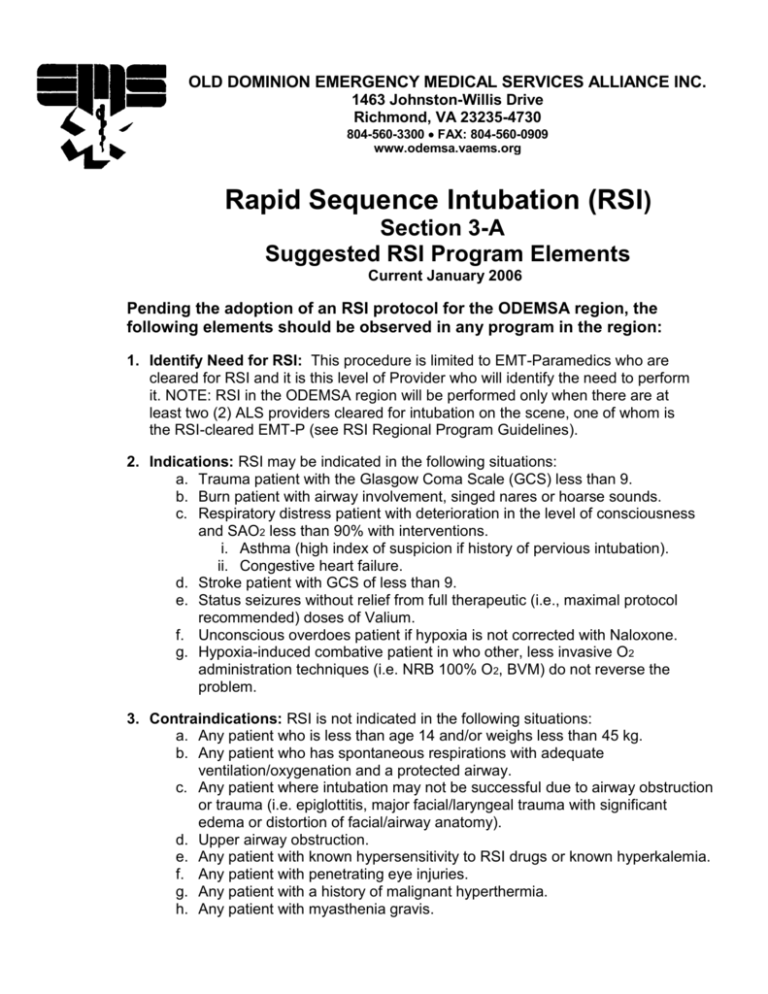
OLD DOMINION EMERGENCY MEDICAL SERVICES ALLIANCE INC. 1463 Johnston-Willis Drive Richmond, VA 23235-4730 804-560-3300 FAX: 804-560-0909 www.odemsa.vaems.org Rapid Sequence Intubation (RSI) Section 3-A Suggested RSI Program Elements Current January 2006 Pending the adoption of an RSI protocol for the ODEMSA region, the following elements should be observed in any program in the region: 1. Identify Need for RSI: This procedure is limited to EMT-Paramedics who are cleared for RSI and it is this level of Provider who will identify the need to perform it. NOTE: RSI in the ODEMSA region will be performed only when there are at least two (2) ALS providers cleared for intubation on the scene, one of whom is the RSI-cleared EMT-P (see RSI Regional Program Guidelines). 2. Indications: RSI may be indicated in the following situations: a. Trauma patient with the Glasgow Coma Scale (GCS) less than 9. b. Burn patient with airway involvement, singed nares or hoarse sounds. c. Respiratory distress patient with deterioration in the level of consciousness and SAO2 less than 90% with interventions. i. Asthma (high index of suspicion if history of pervious intubation). ii. Congestive heart failure. d. Stroke patient with GCS of less than 9. e. Status seizures without relief from full therapeutic (i.e., maximal protocol recommended) doses of Valium. f. Unconscious overdoes patient if hypoxia is not corrected with Naloxone. g. Hypoxia-induced combative patient in who other, less invasive O2 administration techniques (i.e. NRB 100% O2, BVM) do not reverse the problem. 3. Contraindications: RSI is not indicated in the following situations: a. Any patient who is less than age 14 and/or weighs less than 45 kg. b. Any patient who has spontaneous respirations with adequate ventilation/oxygenation and a protected airway. c. Any patient where intubation may not be successful due to airway obstruction or trauma (i.e. epiglottitis, major facial/laryngeal trauma with significant edema or distortion of facial/airway anatomy). d. Upper airway obstruction. e. Any patient with known hypersensitivity to RSI drugs or known hyperkalemia. f. Any patient with penetrating eye injuries. g. Any patient with a history of malignant hyperthermia. h. Any patient with myasthenia gravis. 4. Prepare the Patient: a. Pre-oxygenate by BVM and/or NRB 100% O2. b. C-spine control as needed. c. Place adjunct airway if possible. d. Place patient on ECG and pulse oximeter. e. Establish patient IV access. 5. Prepare Equipment: a. Attach BVM to O2 source. b. Prepare suction. c. Check intubation kit (ETT with syringe and stylette, laryngoscope and blade). d. Check capnography (EasyCap and cardiac monitor). 6. Pre-medications: a. Make sure that all required drugs that are expected to be used are easily accessible and in premixed condition so that they are immediately available upon demand during RSI. b. Administer at minus-three (3) minutes: i. Lidocaine 1.0-2.0mg/kg IV 2-5 minutes before laryngoscopy unless contraindicated. ii. Atropine 0.01mg/kg IV unless contraindicated. iii. Defasiculating dose of Vecuronium 0.01mg/kg if needed. 7. Sedation: (zero point) a. Administer Etomidate 0.3mg/kg (draw up appropriate amount from 40mg vial) IV push. b. Administer Versed 2.0-5.0mgs IV push (based on dosing of .05 mg/kg). Versed should be administered two (2) full minutes before intubation is attempted. c. Paralytics are not indicated if a patient may be adequately and safely intubated after the sole administration of Versed. 8.) Paralysis: (zero point) a. Administer Succinylcholine 1-1.5mg/kg. i. 30- to 40-second onset that lasts four (4) to six (6) minutes. ii. Monitor for fasiculations. b. Administer Vecuronium 0.1 mg/kg IV push (maximum initial does 10mg). i. Produces clinical effects in approximately 30 seconds and intubation paralysis in 1-4 minutes. ii. Reconstitute vial with 10ml of normal saline and shake thoroughly. iii. Re-dosing is ½ initial dose IVP 20 minutes after initial dose as indicated. 9.) Intubation: c. This initially is handled by the second ALS provider. RSI-cleared EMT-P handles medications. d. Approximately 30 seconds after administration of the paralytic, the patient’s muscles will relax and respirations will cease. e. Do not attempt laryngoscopy until the mandible is flaccid. f. RSI-cleared EMT-P applies cricoid pressure. 2 g. If trauma patient, maintain manual in-line c-spine stabilization. h. Perform first intubation within one minute. i. The position of the endotracheal tube in the trachea must be confirmed by three (3) different methods and those three methods must be documented in the medical record. j. If intubation is successful, do not administer any additional sedation or paralytics. k. If the FIRST attempt is unsuccessful, the RSI-cleared EMT-P MUST perform all subsequent attempts l. If the RSI-cleared EMT-P is unsuccessful, maintain BVM with an adjunct airway. m. If three (3) intubations fail, place Combitube. Verify oxygenation and ventilation as below. n. If BVM measures fail and Combitube does not provide adequate ventilation and oxygenation, perform immediate surgical cricothyroidotomy. 10.) Verification: a. Acceptable documentation of tube placement may include: i. Presence of bilateral breath sounds and absence of breath sounds over the epigastrium. ii. Presence of condensation on the inside of the ET tube. iii. End tidal CO2 monitoring on three consecutive breaths. iv. Esophageal detection device. v. Visualize tube passing chords. 11.) Secure Endotracheal Tube: a. Secure endotrachael tube with holder. b. Place C-collar to stabilize patient’s neck. c. Use extreme caution when moving patient to prevent tube from becoming dislodged during movement. Re-verification is mandatory after a movement and must be documented. 12.) Long-term Paralysis and Continued Sedation: a. Once the ETT has been verified and secured: i. Administer Vecuronium 0.1mg/kg for paralysis. ii. Administer ??. iii. Consider Morphine 4.0mg for analgesia (head injury or multiple trauma) with BP maintaining. 1. Blood pressure> 100mmHG. 2. Repeat after 20 minutes of transport time and if BP tolerates. 13.) Considerations: a. Once a neuromuscular blocking agent is given, the provider assumes complete responsibility for maintaining an adequate airway and ventilations. b. The provider must be prepared to perform a surgical airway if intubation cannot be executed and ventilation with a Combitube or BVM is not possible. c. The provider can maintain sedation/paralysis per re-dosing schedule. 3 d. e. The provider must monitor oxygen saturations and end-tidal carbon dioxide continuously. On-line medical control always is an option. 14.) Chemical Restraint Policy: a. Patients who are sedated for procedures and then maintained in a chemically induced state of “control” following that procedure should be managed according to the EMS agency’s restraint guidelines. 15.) Notification, Documentation and QA: a. Documentation will be completed on the Prehospital Patient Care Report (PPCR) and any agency reporting document b. Each agency must set up a notification process that includes appropriate agency leadership and the agency Operational medical Director (OMD) as soon as possible by pager, phone or e-mail. c. Each agency must establish a documentation and quality assurance process d. The ODEMSA Medical Control Committee has adopted a policy that all incidents where RSI is performed on a patient will be reviewed by the agency OMD and the agency’s QA/QI committee. ##### January 2006 4