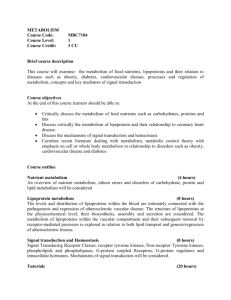
Alcohol Metabolism
advertisement

Alcohol Metabolism Week 30 LO’s 1. Outline the biochemical pathways by which alcohol is absorbed and metabolised in the body. 3. Explain the pharmacokinetics of alcohol, including why alcohol has simple kinetics with a constant rate of metabolism per hour. Absorption rapidly absorbed primarily from duodenum peak blood alcohol concentration (BAC) depends on: o amount and [alcohol] of beverage o rate of drinking o food consumption and composition e.g. high lipid content → ↓EtOH absorption o gastric emptying and gastric metabolism carbonation ↓ gastric emptying time (more rapid absorption e.g. champagne) o hepatic first pass metabolism Metabolism ethanol metabolism occurs almost entirely in the liver (90-98%) mainly by a pathway involving successive oxidations to produce acetaldehyde and then acetic acid 1st step – oxidation by alcohol dehydrogenase – rate-limiting and zero-order (constant amount/unit time) EtOH oxidation requires NAD+ and its availability: o is rate-limiting factor (limits EtOH metabolism to about 8g/h) o leads to competition between EtOH and other metabolic substrates for available NAD+, which may be factor in EtOH-induced liver damage accumulation of acetaldehyde (intermediate metabolite) contributes to hepatotoxicity and is associated with headache, gastritis, nausea, dizziness (hangover) alcohol dehydrogenase: o oxidizes EtOH → acetaldehyde o reduces NAD+ → NADH mixed function oxidase system also metabolises EtOH → acetaldehyde (see slide 26 of lecture) usually this pathway only accounts for a small proportion of EtOH metabolism but it is up regulated in alcoholics EtOH can affect the metabolism of other drugs that are metabolized by the mixed function oxidase system (e.g. phenobarbitone, warfarin and steroids) nearly all acetaldehyde produced → acetate by acetaldehyde dehdrogenase Excretion Kidney – since most Etoh is metabolized, very little is excreted by kidney (can’t hasten exctretion with diuretucs) Lungs – constant % of blood alcohol levels are excreted – tiny amount but basis of breathalyzer test Ethanol Metabolism shows saturation or zero-order kinetics: disappearance of the drug from the plasma is linear i.e. EtOh is removed at a constant rate independent of [Plasma] the reason for this is that the rate of oxidation by alcohol dehydrogenase reaches a maximum at low EtOH concentrations due to the limited availability of NAD+ 2. Describe the effects of alcohol on other biochemical pathways, including fat, carbohydrate and energy metabolism. o o >70g of alcohol places a large load upon liver leading to metabolic abnormalities Some biochemical effects of alcohol are attributed to cofactors used in its metabolism, which limit the availability for other pathways. Glucose metabolism: Gluconeogenesis is decreased due to the decrease in NAD+ levels as a result of alcohol metabolism o pyruvate is converted to lactate to increase the availability of TCA intermediates (Pryuvate + NADH → lactate + NAD+) o results in hyperlacticacidaemia and lactic acidosis acute intoxication can lead to severe hypoglycaemia and sudden death due to ↓ in TCA intermediates (e.g. OOA) ↑ Synthesis and ↑ lactate utilization leads to acidosis which leads to ↓ renal excretion of uric acid (from purine degradation) – hyperuricaemia Protein metabolism: Protein synthesis is decreased due to an unknown mechanism. Fat metabolism: decrease in TCA activity → Fatty acid oxidation inhibited metabolic purpose of FA oxidation – produce NADH for ATP synthesis by oxidative phosphorylation BUT in alcohol metabolism – NADH is produced – thus FA oxidation is ↓ excess NADH signals for Fatty acid synthesis to ↑ impaired assembly and secretion of lipoproteins All of these lead to steatosis or fatty liver . Anaerobic metabolism: ↑lactate production from pyruvate due to an ↑ in NADH:NAD+. Utilisation of lactate decreases leading to hyperlactacidemia, acidosis, and hyperuricaemia. Other: Inhibition of oxidation steps involved in testosterone synthesis gynecomastia and testicular atrophy.