Upper GI endoscopy
advertisement

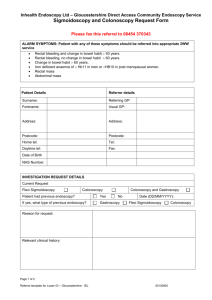
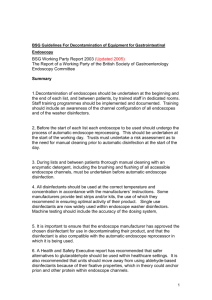
Upper GI endoscopy “Hospital without walls” Your doctor has recommended that you have a procedure called an upper gastrointestinal endoscopy (this procedure can also be called a gastroscopy or just an endoscopy). This leaflet will tell you what to expect. What is an upper gastro-intestinal endoscopy? Gastro-intestinal means “to do with the stomach and intestines”. An endoscopy is the term used when the doctor looks inside you by passing a tiny camera down your throat on the end of a very narrow and flexible tube called an endoscope. So an upper gastro-intestinal endoscopy is when the doctor uses an endoscope to look inside the upper part of your digestive system - that’s your gullet, stomach and small intestine. How can I prepare for my endoscopy? The procedure must be performed on an empty stomach, so you shouldn’t eat or drink anything for at least 6 hours beforehand. Before the procedure, a doctor will explain to you what is going to happen, and you will be asked to sign a consent form to show that you have understood what they are going to do. You should tell a nurse or doctor if you have any allergies or if you have had a bad reaction to other tests or to any drugs, or if you have had an endoscopy before. This is also a good time to mention any worries or questions, so that you can relax before the procedure. You might be asked to undress and put on a hospital gown, and to remove false teeth. What will happen during my operation? You will lie on your left side on a couch. You may have a local anaesthetic sprayed on the back of your throat to numb it, or you might have to suck a tablet which will have the same numbing effect. You might be given a sedative injection, although not all hospitals do this as the endoscope is so small that you can swallow it without difficulty. To hold your mouth slightly open, a plastic mouthpiece will be put between your teeth. The doctor will pass the tip of the endoscope down into your stomach through your mouth. This will not hurt, and it will not affect your breathing. A nurse will stay with you during the operation. The procedure may take up to 15 minutes, and the doctor may have to pass some air through the tube into your stomach to give him a clearer view by creating more space for the endoscope. After the test, this air will be sucked out, and the tube will be removed right away. You might find that lots of saliva collects in your mouth, as you won’t be able to swallow. The nurse will suck this out using the same sort of sucker that you might have seen at the dentist. The doctor might want to take a biopsy, which is a tiny sample of tissue from inside you that can be looked at in a laboratory. The sample is taken through the endoscope; this doesn’t hurt. What will happen after the procedure? You will stay on the couch resting for half an hour, under the care of nursing staff. You will be allowed to have a drink, but if your throat has been numbed for the endoscopy, you won’t be able to swallow right away and will have to wait for the anaesthetic to wear off (this takes 1-2 hours). You can then eat and drink normally, although your throat may feel a bit sore and you might feel a bit bloated if there is still some air in your stomach. Both feelings are normal, and will clear up by themselves. If you are going home on the same day you must arrange for someone to drive you home if you have been given any sedative. The sedative will stay in your system for a while so you should rest for the rest of the day, and you should not drive, operate machinery or drink alcohol. Check with the doctors whether they have given you anything that will affect your ability to do these things. You should be able to resume normal activities on the day after the procedure. When will I get my results? The doctor may be able to tell you the result of your endoscopy straight after it is done. If a biopsy has been taken, however, it will probably be sent away to be examined, so you might have to wait a few days for the results. You should try to have someone with you when you get your results, since if you have had a sedative you will feel quite ‘woozy’ and may not remember everything the doctor tells you. You can discuss your test results in detail with the doctor who recommended that you have the endoscopy. We hope this leaflet has answered your questions. Please ask your doctor or the hospital staff if you feel worried or unsure about anything. Potential complications of colonoscopy There is a very small risk of piercing the wall of the bowel with the endoscope. The risk is slightly higher when a polyp is removed. If this does happen, it can be fixed with an operation. After a polyp has been removed, you might have a bit of bleeding from your back passage. The chance of this is about 1 in 500, and it usually stops without treatment. Occasionally, if this bleeding doesn’t stop by itself, an operation might be necessary. There is also a small risk of bleeding after a biopsy has been taken, and you might see blood in your stools or on the toilet paper the first time you have a bowel movement after the colonoscopy, but this is also unusual and should clear up within 24 hours. Other tests you might have Sometimes the bowel cannot be fully examined with a colonoscope. This is usually either because of previous abdominal surgery, where there is scar tissue or a delicate place in the bowel, or because the patient finds the procedure uncomfortable. You will be given sedatives and painkillers for the procedure (general anaesthetic is not used, however), and most people don’t have any problems with it. If you do feel pain or discomfort, please let the doctor know and they will stop. A different test such as a special CT scan or a barium enema can be used instead. However, colonoscopy is thought to be the best way of examining the bowel because it gives the doctors more information than other test