NUR248Clinical Packet Fall 2011 - Suffolk County Community College
advertisement

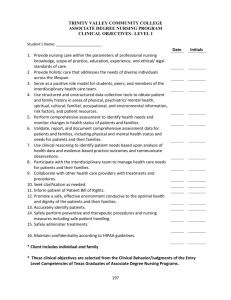
1 SCHOOL OF NURSING CLINICAL PACKET Catalog: NUR248 Course Title: Maternal/Child Health Nursing – Level II Credits: 4 Revised: 5/2011 2 NUR248 CLINICAL PACKET TABLE OF CONTENTS CLINICAL FOCUS 8 POINT POSTPARTUM ASSESSMENT 3 4 DAILY NURSING PROCESS PLAN 6 DRUG EVALUATION GUIDE 10 NEWBORN ASSESSMENT TOOL 11 CLINICAL ASSIGNMENTS COVER PAGE 13 TEACHING PLAN 14 SELF EVALUATION CRITERIA 18 Level II CLINICAL EVALUATION 19 GUIDELINES for FAILED CLINICAL DAY 22 WRITTEN ASSIGNMENT REQUIREMENTS 23 HAND OFF REPORT 24 SUFFOLK COUNTY COMMUNITY COLLEGE SCHOOL OF NURSING NUR248 CLINICAL FOCUS 1. Identify obstacles to parenting, bonding and client learning about self and newborn. 2. Implement client education on one (1) important area of focus identified through assessment. 3. Describe a comparison of Nursing Care for NSD vs C/S delivery. 4. Identify client adaptations to both physiological & psychological changes of pregnancy. 5. Assess complications of pregnancy and nursing interventions required, ie prolonged nausea & vomiting IV therapy (home or hospital). 6. Prioritize nursing interventions addressing postpartal physiological & psychological changes. 7. Identify the impact of NB teaching and response for new parents. 8. Determine consequences of unexpected early deliver to a primipara vs multipara. 9. Discuss the impact of an adolescent pregnancy or substance abuse on Newborn, the family and nursing staff. 10.Share the physical and emotional impact of respiratory stressors of a Newborn on the family. 11. Discuss patient expectations/reactions to the intrapartal & postpartal experience. 12. Identify and present post partum stressors & adaptation for adolescent, Primip and Multip. 13. Identify safety measures implemented to safeguard Mother & newborn in each obstetrical area. SUFFOLK COUNTY COMMUNITY COLLEGE SCHOOL OF NURSING 8 POINT POSTPARTUM ASSESSMENT How carefully do you make routine postpartum checks? Do you follow a logical order of assessment or neglect one or two or maybe three steps now and again? Is your assessment as meaningful for the mother as for the next person who will read her chart? To avoid any such problems on the maternity unit, our students use an 8 point check when assessing postpartum patients. It promotes concise, accurate charting and insures early detection of postpartum abnormalities. It also provides the opportunity to teach self and baby care to the mother during assessment. Here’s how you can use the system, too. Before beginning, be sure that the mother has emptied her bladder and that she is lying in a supine position on a flat bed. Explain each procedure to her and inform her of your findings. 1. B Breasts: Gently palpate each breast. What is the contour? Are the breasts full, firm, tender? Are the veins distended? Is the skin warm? Does the patient complain of sore nipples and are her breast so engorged that she requires pain medication? If you feel nodules (lumps) in the breasts, they may be there because the ducts were not emptied at the last feeding. Take this opportunity to explain the process of milk production. Instruct her on what to do about engorgement; show her how to perform self-breast examinations, and answer any questions she may have about breastfeeding. 2. U Fundus: (Uterine) – Position client with knees flexed and head flat. Palpate the fundus with clean examination gloves on. Stabilize uterus at symphysis with one hand. Below umbilicus, cup hand and press firmly into abdomen. It should be firm and should decrease, approximately one fingerbreadth below the umbilicus each day. Have the patient feel her uterus as you explain the process of involution. If the uterus is not involuting properly, check for infection, fibroids and lack of tone. Unsatisfactory involution may result if there are retained secundines or the bladder is not completely empty. Ex: Day 1 (2 to 24 hours) Fundus at umbilicus or just below, Firm @ U. 3. B Bladder: Inspect and palpate the bladder simultaneously while checking the height of the fundus. Bladder distension should not be present after recent emptying. When it does occur, a suprapubic rounded bulge over the bladder area is observed, dull to percussion while at the same time, the mother usually feels a need to urinate. When bladder is distended, uterus is bogy well above umbilicus, and to client’s right side. Ask client to void, measure amount voided. If unable to void – an order from the physician is necessary so that catheterization may be done. The physician may order a culture and sensitivity test, since definitive treatment may be required. Reassess after voiding (catheterization). Bladder should not be palpable. Infection of the urinary tract must be prevented from occurring. This is why it is imperative that the first three postpartum voidings be measured and should be at least 150 cc. Frequent small voidings, with or without pain and burning, may indicate infection or retention. If voidings are frequent and large, explain the diuresing process to the mother. Talk to the mother about proper perineal care. Explain that she should wipe from front to back after voiding and defecating. This helps prevent urinary tract infection and is a hygienic principle that pertains to females of all ages. Peri bottle with warm water should be used every time she voids or defecates. 4. B Bowel function: Question the patient daily about bowel movements. She must NOT become constipated. If her bowels have not functioned by the second postpartum day, you may want to start her on a stool softener. Encourage her to drink extra fluids and to select fruits and vegetables from her menu (avoid sweets, etc.). Notify the doctor if the lochia looks abnormal in color or quantity, if it has an unusual odor or contains clots other than small shiny ones. Inform the mother about what changes she should expect in the lochia and when it should cease. Instruct her on when her next menstrual period will probably begin and when she can resume sexual relations. You m ay also want to discuss family planning at this time. 5. L Lochia: Assess the amount and color of lochia on the perineal pads in relation to the number of postpartum days. Teach client that for the first 3 days, she should find a very red lochia, similar to the menstrual flow. During the next few days it should become watery or serous, and on the tenth day, it should become thin and colorless (yellow or white). Check linen under mother’s buttocks for additional drainage. . 6. E Episiotomy/Perineum: Ask or assist client to turn on her side and flex upper leg on hip. Although episiotomies are routine, don’t overlook the importance of inspecting them thoroughly. Use a flashlight if necessary for better visibility. To determine if the wound is healing properly, check for infection, inflammation and suture sloughing. Is the surrounding skin warm to the touch and does the patient complain of discomfort? You should notify the doctor if any occur. Also check the rectal area. If hemorrhoids are present, the doctor may want to start the patient on a sitz bath and local analgesic medications. Most postpartum patients – especially those who are mothers for the first time will have questions about stitches. “When will they be removed?” “Will they pull out during bowel movement?” Reassure her as you answer these and other questions she may have regarding her pain, cleanliness, and coitus. 7. H Homan’s sign – assess lower extremities for: swelling and/or pain in calf; Assess full ROJM, no muscle weakness skin warm, dry and intact. Dorsalis pedis and pedal pulses present. 8. E Emotional status: Throughout the physical assessment, notice and evaluate the mother’s emotional status. Does she appear dependent or independent? Is she elated or despondent? What does she say about family support? Are there other nonverbal clues? ck Revised 5/10 DAILY NURSING PROCESS PLAN NUR 248 Date of Care ________ Pt. Initials_____ Age ____ Room #_____EDC_____ Date/Time of Delivery______ Gestation________ Pre-Delivery: G:_____ P:_____ (T:____P_____A_____L_____); Post-Delivery: G:____P:____(T:____P:_____A:____L:_____) Pregnancy History: _____________________________________________Type of Birth _____________Reason____________ Wt._______ Ht. _______ Diet _____________ Appetite ______________ Formula/Breast/Frequency____________________ Admitting Diagnosis:_____________________________________Allergies:_________________________________________ Surgical Procedure (C/S, Episiotomy, Laceration, Anesthesia,)_____________________________________________________ PMH/PSH/Social/Family (include birth health history, maternal (pregnancy) health history, childhood medical hx: ______________________________________________________________________________________________________ _______________________________________________________________________________________________________ Labor Hx: _____________________________________________________________________________________________ Planned/Unplanned Pregnancy: _________________Pre/Post Delivery weight:_________/________ Weight gain:___________ Immunization Profile _________________________________________________________________Activity _____________ Vital Signs: T:_______ Pulse: _______ Apical: _______ RR: _______ B/P: _______ SaO 2 _______ Pain Scale:___________ IV __________________________________________________________________ ( Solution, Site, Gauge, Date, Time) Intake _________ Output _________ Foley Catheter ____________ Drains _______________________________________ SUBJECTIVE/OBJECTIVE ASSESSMENT: Circle and describe Client’s Stressors Include positive and significant negative findings. (GIVE DETAILED DATA) BUBBLE HE Domain #5, 11: Neurological B S: O: Domain # 5, 6: Mood/Affect/Emotions U S: O: Domain # 4: Thorax and Lungs B S: O: Domain # 4:Cardiovascular B S: O: Domain # 4: Peripheral Vascular L S: O: Domain # 2,3: Gastrointestinal E/I (epiosiotomy, laceration, incision) S: O: Domain # 3,8: Genitourinary H S: O: Domain # 4, 11: Musculo-Skeletal E S: O: Domain # 2, 3, 11, 13: Skin, Hair, Nails S: O: DAILY NURSING PROCESS PLAN MEDICATIONS: [Include 5 Meds] * Complete Page 10 for each medication. Add additional pages as necessary with interpretation of abnormal labs. ** Post Del Labs Pregnan Expected Labs Pregnancy Values cy Values Values Values RBC GBS Status Hgb Rubella Titer Hct Hep BsAg Platelets HIV WBC U/A Type & Rh Drug Level RPR Other Explain Abnormal Labs: Post Del Values Expected Values Diagnostic Tests, Procedures, Treatments, Dressings: Client/Parent Teaching Topics: (Include health education/prevention & areas of knowledge deficit). ____________________________________________________________________________________________ ____________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ Write SHORT TERM GOALS for ALL Nursing Diagnoses: Nsg.Dx 1:_______________________________________________________________________________________________ Nsg.Dx 2:_______________________________________________________________________________________________ Nsg.Dx 3:_______________________________________________________________________________________________ Nsg.Dx 4: _______________________________________________________________________________________________ Nsg.Dx 5: _______________________________________________________________________________________________ 5 Nursing Diagnoses MUST be listed in priority order and at least 3 Nursing Diagnoses MUST be worked up. PRE/POST-CONFERENCE DIAGNOSES/COLLABORATIVE PROBLEMS Add additional pages as necessary ** Tentative Nursing Diagnosis 1. 2. 3. Actual Nursing Diagnosis [Includes “Actual” & “Risk For”] Place in priority order in PES format. 1. 5 Interventions for 3 Nursing Dx ________________________________ 2. 3. 4. 5. NURSES NOTE: Write Evaluations for Interventions/Goals Newborn Date of Care _________ Pt. Initials ______ Age ______ Room # ______Date/Time of Delivery ___________Gender:____________ Apgar _________ Birthweight: _________gms. _______lbs._______ oz _______ Length: _______cms_______ inches____________ T: ________ AP: ___________ RR:_________ Skin color: ___________Gest Age__________Stooling Pattern: ________________ Voiding Pattern: _______________Umbilical Site: ______________ Circumcision Site: ______________Voided after Circ________ Blood Type: _____Rh____ Coombs _______ Glucose Monitoring: AC#1 _____ mg/dL. AC#2______ mg/dL. AC#3 ______mg/dL Feeding: Breastfeeding/Formula (circle one or both) Amount of Time on each breast per feeding __________________________ Formula: __________Amount taken and tolerated __________Frequency of feeding: __________Time of last feeding ___________ Sleeping: # of hours during day ________________# of hours during night___________________ Abnormal Findings: _________________________________________________________________________________________ MEDICATIONS: Complete Page 10 for each medication. Include: Hep B vaccine; Erythromycin Ointment; Vitamin K. Client Values Labs Expected Values Interpretation of Abnormal Values Glucose Type & Rh Total Bilirubin Direct/Indirect Bilirubin PRE/POST CONFERENCE DIAGNOSES/COLLABORATIVE PROBLEMS Tentative Nursing Diagnoses 1. 2. 3. Actual Nursing Diagnoses [Includes “Actual and Risk For”] Place in Priority Order in PES format. 5 Interventions for 3 Nsg Dx 1. 2. 3. 4. 5. Write SHORT TERM GOALS for All Nursing Dx: 1. 2. 3. 4. 5. Write Evaluations for Interventions/Goals NUR 248 - DRUG EVALUATION GUIDE Name: ___________________________________ Pt. Initials: __________________________ Date: ___________________________________ Clinical Assignment #: _________________ DRUG NAME: ______________________________________ Pregnancy Category:___________ Generic Name: ___________________________________________________________________ Classification: ____________________________________________________________________ Action: __________________________________________________________________________ Indications for use: _________________________________________________________________ Pt. Dose: _________________________________ Usual Dose: _________________________ Route Prescribed: ___________________________Alternate Routes available: _______________ Schedule of Administration: __________________________________________________________ Major Side Effects and Toxicity: Nursing Implications (include patient assessments and pertinent lab data): Contraindications and Precautions: Patient Education: Reason Why This Patient Is Taking Medication: NEWBORN ASSESSMENT TOOL (Due once during the course) Student Name:_____________________ Date & Time of Exam:_____________ Baby’s Initials:_____________________ Date & Time of Delivery:_____________ Sex: Male_________ Female________ Weeks Gestation_________ Breast/Bottle/Both___________ TYPE OF DELIVERY Normal Vaginal Delivery___________ Forcep____________ Vacuum___________ Primary C/S___________ (Reason) Repeat C/S________ CLASSIFICATION Pre-Term_______________ Post-Term____________ Term________________ SGA________AGA______LGA_______ VITAL SIGNS: Temp__________ Apical HR____________ Respirations__________ ACTIVITY: Active/Alert______________ Lethargic____________ MEASUREMENTS: Weight ____________ Length ____________ Head Circum ____________ Chest Circum ____________ Gms Cms Cms Cms ____________ ____________ ____________ ____________ Lbs/ozs Inches Inches Inches COLOR: Pink: _____________________ Pallor: ____________________ Ruddy: ____________________ Jaundice: __________________ Phototherapy _______________ Skin: Acrocyanosis Cyanosis Dryness Rash Desquamation Meconium stained Petechiae Lanugo Other ________________ Head: Normocephalic Fontanels soft (Circle One) Fontanels: level depressed bulging Molding Cephalhematoma Caput succedaneum Forcep marks Bruising Overriding Sutures Other_______________ Mouth: □ Lips intact □ Soft Palate intact □ Hard Palate intact □ Symmetry □ Pink mucosa Other_____________ Thorax: □ Symmetry □ Clavicles intact □ Breath sounds (bilateral) □ HR rhythm regular □ Arrythmia □ Murmur □ Tachypnea □ Grunting □ Retractions Other_______________ Eyes: □ Conjunctiva pink □ Cornea clear □ Scleral hemorrhage Other_______________ Abdomen: □ Symmetry □ 3 vessel cord □ Bowel sounds □ Femoral pulses (bilateral) Other______________ Ears: Normal placement Normal shape Other_______________ Back: □ Vertebral Column intact □ Sacral Dimple Other______________ Nose: Neuro: □ □ □ □ □ □ □ □ □ □ □ Nares Bilateral & Patent Nasal Flaring Milia Other_______________ Genitalia: Male □ Testes descended □ Epispadias □ Hypospadias □ Hydrocele Other ___________ Female □ Vaginal Tag □ Pseudomenstruation Other___________ Extremities: □ Peripheral Pulses □ Full hip rotation □ Gluteal Folds □ Symmetry of movement Symmetry of limbs □ Hip click Other______________ Anus patent Passed stool Lusty Cry Tonus Normal Stepping Babinski Suck Swallow Moro Palmar Plantar Grasp Rooting Other______________ Voided Date/Time Intake Breast or bottle (amt per feeding) Void Stool (color) **PLEASE SUBMIT A SEPARATE SHEET WITH THE DEFINITIONS OF ALL THE BOLDED TERMS AND HOW THE REFLEXES ARE PERFORMED (separate sheet of paper –typed) Revised 12/10 SUFFOLK COUNTY COMMUNITY COLLEGE NURSING DEPARTMENT NUR 248 CLINICAL ASSIGNMENTS STUDENT’S NAME________________________________________________ Online Community Perinatal Assignment: ________________ 4 page Daily Nursing Process Plan on Mother & Infant: (Mother & NB Meds) #1___________________________________________________________ #2___________________________________________________________ #3___________________________________________________________ One Evidence-based journal article with summary R/T your Patient:____________ Newborn Assessment Tool with Definitions: ______________________________ Case Study: _________________________________________________________ Student Self-Evaluation: _______________________________________________ Evidenced-Based Teaching Plan with Reference Page: ______________________ 2 to 3 Professional Evidenced Based Journals _____________________________ Please tape this sheet to a brown manila envelope. Complete information on specific area with appropriate data. Place assignment in envelope. Refer to page 4 (course outline) for details. Submit to instructor. Rev 5/11 Suffolk County Community College NUR248 Teaching Plan: Write topic here Target Group: Who are you going to teach this to? For example: new mothers, new fathers, adolescents, staff nurses. Expected Outcomes: List at least 3 objectives. For example: At the end of the session _____ will: 1. 2. 3. Teaching Tools/ Methods: List tools/methods that you will be using. For example: handouts, 1:1 demonstration, a pre/post test, a poster board presentation Interventions: List at least three nursing interventions. 1. 2. 3. Evaluation of Outcomes: Document the client’s response to the teaching provided. (3 sentence minimum) Reference Sheet: Include references utilizing APA format and submit 2-3 hard copies from professional nursing journals in support of your topic and teaching plan. Grade: Pass/Fail Revised 5/10 SUFFOLK COUNTY COMMUNITY COLLEGE SCHOOL OF NURSING NUR248 APA Bibliographic and Parenthetical (in-text) Citations Publication Manual of the American Psychological Association,(2010) 6 thed. For APA Online Electronic References go to. http://www.apastyle.org/elecref.html You can access information on APA format from the College web site. Follow the directions below to access this information: 1. Go to http://www3.sunysuffolk.edu/index.asp 2. Click on Academics 3. Click on Library 4. In the upper right hand corner of the library web page, scroll on Hours, Directions, Services, etc until you get to Library Handouts 5. Click on Library Handouts 6. Look under Ammerman campus and you will find various guidelines to APA format 7. Click on each of the following: Guide to APA format, APA Reference List: Basic Rules, APA Citations for Nursing and APA Sample References. 8. In the upper right hand corner there is a Print Friendly Version link for each of the above guidelines. Print this information. 9. Refer to this information when writing your EB Teaching Plan Reference Page SUFFOLK COUNTY COMMUNITY COLLEGE Suggested Topics – Early Start Sections 1. A mother who is breast feeding 2. The pregnant adolescent and available support services 3. The various methods of contraception 4. The sexually active adolescent, focusing on providing information about sexually transmitted diseases 5. The “Brand New Dads” 6. Car seat safety for newborn/toddler/child and child proofing home 7. Sudden Infant Death Syndrome (SIDS) 8. Cord blood/stem cell banking 9. Sibling rivalry toward a newborn 10. Bereavement support services. 11. Effects of smoking during pregnancy 12. Effects of alcohol during pregnancy 13. Effects of drug use in pregnancy SUFFOLK COUNTY COMMUNITY COLLEGE Suggested Topics - Late Start Sections 1. Prepare teaching plan for childbirth education. 2. Prepare teaching plan for a client who is scheduled for amniocentesis, stress test, or chorionic villus sampling. 3. Prepare teaching plan for a client from a low income family, including how to obtain available community resources for mother and infant. 4. Prepare teaching plan to assist the woman in labor determining when to go to the hospital. 5. Develop care plan for non-pharmacological pain management. 6. Prepare teaching plan for a client having induction of labor. 7. Develop exercise plan for the postpartum woman. 8. Develop a teaching plan describing newborn care. 9. Develop teaching plan for a mother who is breast feeding. 10. Develop teaching plan for a mother who is formula feeding. 11. Develop teaching plan for the pregnant adolescent and available support services. 12. Develop teaching plan on the various methods of contraception. 13. Prepare teaching plan discussing Shaken Baby Syndrome. SCHOOL OF NURSING NUR248 – Maternal Child Nursing SELF EVALUATION CRITERIA NUR248 students are expected to become more actively involved in the clinical evaluation process by writing a self reflective commentary on their learning at the end of the course. Students will be rotated to specialty areas at the respective agency, with independent learning occurring in each area. Hence, it is helpful for students to identify their implementation of knowledge and skills as well as personal growth in new learning arenas. To evaluate oneself is a valuable life skill which will be an asset to you long after you graduate and leave SCCC. There is no single way to write a good self-evaluation. It is suggested that you address most of the points below. Give time and thought to what you write. It may be helpful to image being in an interview setting and asked to explain your strengths and reasons why you should be hired. Weaknesses should also be addressed and should include ways to improve and change them into strengths. The following is provided to assist in the writing of a Self Evaluation. Student self evaluation comments should address: Ability to correlate theory with clinical practice. New knowledge, skills and understanding; what did you learn that you’ll remember in a year? In five years? What things were difficult or frustrating? Which were easy? Critical Thinking; clinical decision making. Collaborating with others; Organizational skills; Managing care effectively & efficiently. Holistic Assessment; Delivery of caring interventions in a variety of settings. Time Management skills; Ability to complete assignments on time. Professional Behavior; accountability for own actions. Prioritization, Delegation abilities. Effective Communication (teaching, health promotion, documentation, etc.). Personal Insights: include things you are proud of; my strongest and weakest points; what did I do to improve the weak points. Include what you want others to know. You will come across strongest if you come across like a real person. SUFFOLK COUNTY COMMUNITY COLLEGE SCHOOL OF NURSING CLINICAL EVALUATION LEVEL II Name: ___________________________________ Final Mid Semester NUR240 _____ Clinical Agency: ___________________________ NUR246 _____ NUR248 _____ # Of Absences: ______ Date: From: _____________To: _____________ Per # Of Clinical Experiences _____ EVALUATION CRITERIA All areas are critical. In Part I, a minimum rating of 2 or better in each category must be achieved on the final evaluation to receive a passing grade. I. PROFESSIONAL BEHAVIOR A. Adheres to standards of professional practice. B. Demonstrates accountability for personal actions and delegated actions. C. Practices nursing within legal, ethical and regulatory frameworks. D. Utilizes and incorporates resources for life long learning. E. Demonstrates leadership in the nursing role. F. Initiates actions that facilitate empowerment for the nursing profession. G. Utilizes constructive criticism, evaluates own nursing competencies and changes behavior accordingly. H. Reports to clinical facility on time. I. Submits written assignments on time. J. Clinical absences do not exceed policy limit. K. Presents a professional appearance. L. Identifies appropriate alternatives when unable to meet a course obligation. M. Reports errors of omission/commission in a timely manner. II. COMMUNICATION A. Identifies similarities and differences on a position and supports their position with current nursing literature. B. Applies advanced techniques of therapeutic communication with clients, significant others and members of the health care team. C. Employs group dynamic strategies when communicating with team members. D. Demonstrates increasing ability to communicate relevant, accurate and complete information for groups of clients verbally and in written documentation. III. ASSESSMENT A. Analyzes health status of clients with multiple health problems. B. Demonstrates advanced skill in completing a health history. C. Integrates prior knowledge in assessing the effects of stressors on clients, families and communities. D. Prioritizes responses to actual or potential health problems and to nursing interventions for individuals/groups of clients in a timely manner. IV. CLINICAL DECISION MAKING A. Analyzes data pertaining to dysfunctional health patterns and stressors of the individual, family and the community. B. Utilizes evidence-based practice in order to formulate clinical decisions. C. Maintains accurate and safe care and an awareness of current National Patient Safety Goals. D. Develops diagnoses and plans care that focuses on actual or potential health problems, promotion, wellness and restoration. E. Modifies client care as indicated by evaluation of outcomes. V. VI. CARING INTERVENTIONS A. Initiates and performs effective and preventative nursing measures to facilitate health promotion and maintenance in clients and groups. B. Acts as an advocate and synthesizes understanding of cultural, spiritual, and developmental needs when caring for individuals/families in order to provide sensitive, holistic nursing care. C. Demonstrates aseptic techniques correctly. D. Administers medications accurately and in accordance with agency protocol. TEACHING AND LEARNING 1 2 3 NA /NO 1 2 3 NA /NO A. Develops teaching/discharge plans to assist individuals and groups to promote health and manage acute and chronic health problems. B. Identifies learning needs of the individual and family and modifies interventions according to developmental level. C. Utilizes teaching and learning concepts in leadership/management in assigned setting. D. Informs patient and family about appropriate community resources. VII. COLLABORATION A. Collaborates with peers and multidisciplinary team members to deliver cost effective, quality care to individuals, families and communities. B. Conveys mutual respect, trust, support and utilization of each discipline’s role and contributions to health care. VIII. MANAGING CARE A. Applies principles of effective motivation. B. Utilizes key concepts underlying effective delegation. C. Demonstrates leadership management skills when working with the multidisciplinary health team members to deliver care to groups of clients. D. Applies strategies of change theory with the health care team. E. Employs techniques that can be used in evaluating the work of others. F. Utilizes conflict resolution skills. G. Assesses visionary skills and identifies a plan to become more innovative. ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ KEY TO PERFORMANCE APPRAISAL 3 = Performance meets clinical objectives and exceeds requirements 2 = Performance meets clinical objectives 1 = Performance does not meet clinical objectives N/A = Not applicable N/O = Not observed Revised 2/02/09 5/2010 DC INSTRUCTOR'S COMMENTS: Daily Nursing Process/Newborn Tool P/F__________Other _________ Instructor's Signature _______________________________________ Date ______ STUDENT'S COMMENTS: Student's Signature ____________________________________ Date __________________ Revised 2/02/09, 5/10 DC SUFFOLK COUNT COMMUNITY COLLEGE SCHOOL OF NURSING Guidelines for Student Written Report of Clinical Incident Resulting in clinical warning or Failed Clinical Day Explanation This is an additional assignment that is given when the faculty identifies student decisions and/or actions that fail to meet the course objectives or standards of nursing practice during a given clinical class. The assignment is made in the spirit of student-centered learning and continued professional development. It provides a framework that assists the student to analyze clinical events, to consult the nursing literature, and to plan future nursing goals for themselves that are in keeping with professional standards. Instructions to Faculty The student’s written report should be submitted on the clinical day following the critical incident. The faculty must discuss the critical incident with the student before making this assignment. The completion of the written assignment provides tangible evidence of the student’s perspective regarding the incident. Further discussion with the student or further action may/may not be necessary depending upon the insight demonstrated in the written report as well as the student’s subsequent clinical practice. Instructions to Students 1. 2. 3. 4. Provide a written report of the critical incident to the clinical instructor. The report is due on the next clinical day following the critical incident. The report should consist of your answers to three basic questions. A. What happened? Describe the details of the incident. What were your nursing actions? What was the patient’s response? What were the actual and the potential consequences for the patient? Include any and all details you deem pertinent. B. What should have happened? Based upon your meeting with your clinical instructor after the incident, and based upon the research you have done since the incident, what should have happened in this clinical circumstance? C. What Nursing Practices will you implement in the future to prevent the recurrence of similar incidents? The report should include a bibliography of at least one pertinent nursing reference. NUR248 Written Assignment Requirements 1. Assignments are due one week after the clinical/community experiences. 2. Maternal/Child Assignments: 2 Daily Nursing Process Plans [3rd is required if #1 and/or #2 is unsatisfactory] 1 Newborn Assessment Tool 1 Evidenced Based Teaching Plan 1 Case Study Presentation 1 Online Community Perinatal Assignment (See Course Outline for specific instructions) Each assignment has specific criteria delineated which must be followed. Students must satisfy every one of the criterion in order to pass the required assignments. Clinical instructor will deem paperwork acceptable or not. Need for revisions will be determined by the clinical instructor. 3. All assignments must be received by the clinical instructor one week before the final day of clinical. 4. PLEASE NOTE: One of your clinical objectives is to hand assignments in on TIME. You MUST meet ALL clinical objectives in order to pass the NUR248 course. Suffolk Community College Nursing Department Hand Off Report All Nursing students should be prepared to give a concise “hand off” report to the RN. It should include the following: 1. Name of patient/s: __________________________________________ Room Number: _______ 2. Diagnosis or Obstetrical Date (DD, PP1, CS1) 3. B B Breast (nipples) Soft, Full, Engorged U Sore/blistered/cracked/erect Uterus (fundus) Palpate height, consistency, position B Bowel B Bladder L Lochia E Episiotomy/Laceration U B B L Bowel sounds, abdomen soft or Distended. BM; passing flatus E H E Voiding: color, amount (measure), odor 4. VS 5. Diet (Tolerance vs NPO) H Homan’s sign 7. IV status; LIB / Meds 8. Pain data (medication given and evaluation of effectiveness) E 9. Infant report: T – P – R; voiding, stooling. Feeding – Formula – Amount taken and tolerated Breast – Time on each breast, frequency, time of last feeding. 11. Anything significant “REEDA” Redness, ecchymosis; edema; drainage; approximation 6. Activity 10. Client Teaching: Rubra, serosa, Small, moderate, large; Odor Emotional Status Pain in calf when foot is dorsiflexed. Verbal and non-verbal communication