Anaphylactic Treatment Guidelines
advertisement
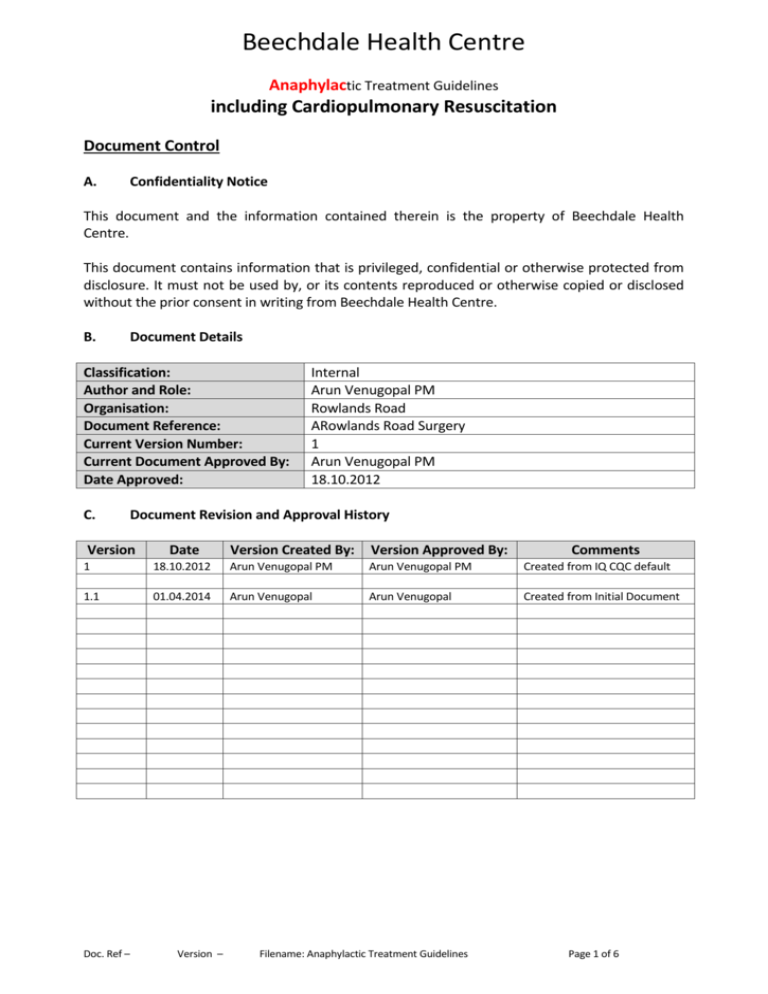
Beechdale Health Centre Anaphylactic Treatment Guidelines including Cardiopulmonary Resuscitation Document Control A. Confidentiality Notice This document and the information contained therein is the property of Beechdale Health Centre. This document contains information that is privileged, confidential or otherwise protected from disclosure. It must not be used by, or its contents reproduced or otherwise copied or disclosed without the prior consent in writing from Beechdale Health Centre. B. Document Details Classification: Author and Role: Organisation: Document Reference: Current Version Number: Current Document Approved By: Date Approved: C. Internal Arun Venugopal PM Rowlands Road ARowlands Road Surgery 1 Arun Venugopal PM 18.10.2012 Document Revision and Approval History Version Created By: Version Approved By: 1 Version 18.10.2012 Arun Venugopal PM Arun Venugopal PM Created from IQ CQC default 1.1 01.04.2014 Arun Venugopal Arun Venugopal Created from Initial Document Doc. Ref – Date Version – Filename: Anaphylactic Treatment Guidelines Comments Page 1 of 6 Objectives That any patient who suffers from an anaphylactic reaction should receive appropriate emergency treatment prior to transfer to hospital; That all staff should receive the appropriate training in order to provide correct and effective treatment. Organisation 1. This is an emergency situation which will be the direct responsibility of the Duty Doctor, with assistance from other available staff as required. When there is no Doctor in the surgery, the Practice Nurse Lead will take responsibility pending the arrival of the emergency services. 2. Personnel • All Doctors and Nurses • Reception staff under the supervision of the Office Manager 3. Resources Information will be in line with Practice procedures, and may be obtained from the following resources: • British National Formulary • Voluntary Services Manual of First Aid • European Resuscitation Council 4. Emergency bag to be kept in the Treatment Room Contents: Resuscitation bag and mask Set of Geudel OP airways Pulse oximeter Oxygen plus trauma masks and tubing Emergency aspirator Nebuliser mask and tubing Scissors and gloves Syringes and needles IV cannulas, saline flushes, tegaderm dressings Drugs: Adrenaline Salbutamol Chlorpheniramine Hydrocortisone (Expiry date of drugs is checked monthly – practice nurse has responsibility for checking the expiry dates) Defibrillator: Kept in treatment room Doc. Ref – Version – Filename: Anaphylactic Treatment Guidelines Page 2 of 6 Administration 1 Record keeping: a) Details of the anaphylactic reaction, treatment provided and outcome to be recorded in the patient’s medical record b) Drugs given – details including time, mode of administration, batch number and expiry date to be recorded. 2 Equipment: Care and maintenance of equipment and ordering of drugs will be the responsibility of the following designated members of staff: a) Equipment and oxygen practice nurses b) Drugs practice nurses c) Defibrillator practice nurses 3 Audit: Information regarding anaphylactic reaction may be audited using the appropriate Emis search facility Training 1 All clinical staff should receive an annual CPR update by an appropriately qualified trainer, and should be familiar with the use of available emergency equipment. 2 All staff who are AED trained must undertake an annual update with an authorised training provider – Sandwell PCT. 3 Reception / office staff should be aware of the action to take in the event of an emergency occurring, and be able to assist where required. Such assistance may include: • Requesting emergency services via the 999 system; • Assisting in resuscitation where CPR / Defibrillator trained; • Providing privacy by screening the area if in a public part of the building; • Caring for relatives. Treatment Refer to Appendices 1, 2 and 3 Review These guidelines are to be reviewed annually Reporting the Death of a Patient to the CQC The death of a patient during an active period of care provision (e.g. if a patient dies at home whilst under the ongoing care of the Practice) requires the Practice to inform the CQC immediately if this should occur. There is a dedicated notification form to report such deaths – it is contained in the Outcome 18 document “Notification of Death - Outcome 18 Composite Statement and Form”. The practice nurse or practice manager at the Practice is responsible for notifying the CQC immediately upon the death of a person who uses the Practice’s services. Where the Registered Persons are unavailable, for any reason, the practice secretary will be responsible for reporting the death to the CQC. Doc. Ref – Version – Filename: Anaphylactic Treatment Guidelines Page 3 of 6 Appendix 1 Treatment of the Conscious Patient Designate team leader 1. Assess the patient • Primary survey • History / signs / symptoms 2. Obtain assistance if not already present and send for an ambulance via 999. Defibrillator trained staff to obtain defibrillator and emergency bag if not already collected from Treatment Room 3. Commence Oxygen via non re-breathing mask 15 litres per minute. 4. Administer Adrenaline 1:1000 by intramuscular injection in accordance with the age related dose chart (Appendix 3). 5. Record and continue to monitor vital signs (P, B/P, R, SaO2). 6. Obtain venous access. 7. Observe for any developing signs of airway obstruction. 8. Be prepared to resuscitate. Any other treatment is given at the discretion of the Doctor(s) attending. The patient must be transferred to hospital for further assessment. Doc. Ref – Version – Filename: Anaphylactic Treatment Guidelines Page 4 of 6 Appendix 2 Treatment of the Unconscious Patient Designate team leader 1. 2. Assess the patient – Primary survey. Assess response to external stimuli. • If the patient is not responding, send for assistance if not already present, and send for an ambulance via 999. • Obtain the emergency bag from the treatment room and the AED from the front office. Team leader to designate the AED team 3. 4. Secure an open airway with a head tilt / chin lift. Check the breathing; • If there is no, or ineffective breathing, commence CPR 30 compressions / 2 inflations with 100% O2 via BVM. NB – CARE WITH ORO-PHARYNGEAL AIRWAYS, MAY EXACERBATE DEVELOPMENT OF AIRWAY OBSTRUCTION AED team to apply electrode pads and follow AED protocol Adrenaline 1:1000 should be administered intramuscularly in accordance with the age related dose chart (Appendix 3) as soon as assistance is available and CPR is established 5. If both breathing and pulse are present, maintain an open airway and administer Oxygen 15L per minute via a non re-breathing mask. Record and continue to monitor vital signs (P, R, B/P, SaO2). 6. Obtain venous access if practicable. 7. Observe for any signs of airway obstruction. 8. Any other treatment is given at the discretion of the Doctor(s) attending. Doc. Ref – Version – Filename: Anaphylactic Treatment Guidelines Page 5 of 6 Appendix 3 Emergency Drugs ADRENALINE 1:1000 by intramuscular injection which may be repeated every FIVE minutes until improvement occurs. Under 6 months 0.05 mg 6 months to 6 years 0.12 mg 6 – 12 years 0.25 mg Adolescent and adult 0.5 mg CHLORPHENIRAMINE 10 – 20 mg given intravenously SALBUTAMOL 5mg, nebulised through Oxygen 6 - 9 L per minute HYDROCORTISONE 100 – 300 mg intravenously OXYGEN 100% (15L per minute) via a non re-breathing mask Doc. Ref – Version – Filename: Anaphylactic Treatment Guidelines Page 6 of 6