Sample Progress Notes
advertisement

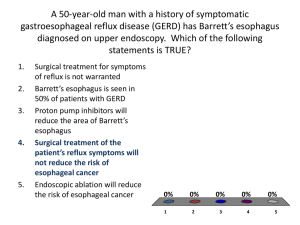
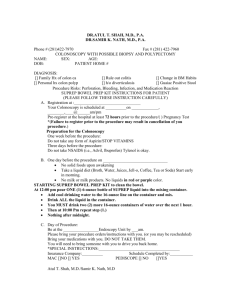
To view each sample’s headings, go to View > Document Map and view individual section headings for each sample down left-hand column of the Word window. Progress Note samples, outpatient setting Progress Note Chart Note Encounter Note Office Note Sample 1 SUBJECTIVE: “I have used the peripheral nerve stimulator in my back for 5 days. While using it I found that I was able to do physical activity without pain. However, afterwards for one day, I would feel pain but then it would go away. I also noticed that I didn’t have to take the Vicodin as much. I took 2 less Vicodin per day and 2 less tramadol everyday. I have not laid in my bed in a year and a half. I sleep in a recliner.” ASSESSMENT: In my medical opinion, the trial was a success in that she was able to decrease her medication intake of narcotics. She was able to perform physical activities with the peripheral nerve stimulator on. While she did experience pain after doing the physical activities, I explained to her that this is due to muscle soreness due to being out of shape and this is to be expected and that is not nerve related. The muscle soreness only had a duration of 24 hours anyway. RECOMMENDATIONS: I will have the trial continue over the weekend and during that time period, I would like for her to lie in her own bed as long as she possibly can with the stimulator on and we will then follow up with her on Monday afternoon, May 10, and then she can have a better idea of how she wants to proceed. Sample 2 PROGRESS NOTE SUBJECTIVE: Mr. Stanford was previously seen on 05/03/10 for a screening colonoscopy. Endoscopic findings revealed evidence of internal hemorrhoids and a sessile polyp size 0.5 cm removed via cold biopsy. The remaining of the inspected colon appeared normal. Pathology findings conclude evidence of segments of hyperplastic polyp but no dysplasia or tubular adenoma. The patient voices after his endoscopy developing two days of nausea and vomiting, which have subsequently resolved. He voices no other GI-related complaints. REVIEW OF SYSTEMS: The patient’s review of systems questionnaire was reviewed and there are no additional pertinent positives. PHYSICAL EXAM: VITAL SIGNS: LUNGS: CARDIO: ABDOMEN: Blood pressure is 143/89. Temperature is 96.2. Current weight is 181 pounds. Clear to auscultation and percussion. S1, S2 within normal limits, without gallops or murmurs. Soft and nontender without organomegaly, mass or ascites. ASSESSMENT: 1. Internal hemorrhoids and benign colon polyp documented via colonoscopy on 05/03/10. 2. Transient nausea and vomiting appears secondary to analgesic administration. Clinically at this time he voices feeling well. PLAN: I recommend a repeat colonoscopy in five years and implementation of a high fiber diet. Otherwise, Mr. Stanford will be seen on an as-needed basis, and I have asked him to return if he develops future GI-related concerns. Sample 3 PROGRESS NOTE PROBLEM: Morbid obesity. SUBJECTIVE: The patient was previously seen on April 21, 2010 for an upper endoscopy prior to proceeding with gastric bypass surgery. Endoscopy of the esophagus revealed low segment Barrett’s esophagus and mild gastritis from which biopsies were obtained. Pathology findings identified evidence consistent with Barrett’s esophagus and H. pylori infection but no dysplasia. The patient has completed appropriate oral antibiotics without difficulty. He presents today voicing no GI-related complaints without nausea, vomiting or abdominal pain. REVIEW OF SYSTEMS: The patient’s review of systems questionnaire was reviewed and there are no additional pertinent positives. PHYSICAL EXAM: VITAL SIGNS: LUNGS: CARDIO: ABDOMEN: Blood pressure is 132/81. Temperature is 97.3. Current weight is 330 pounds. Clear to auscultation and percussion. S1, S2 within normal limits, without gallops or murmurs. Soft and nontender without organomegaly, mass or ascites. ASSESSMENT: 1. Barrett’s esophagus without associated dysplasia. 2. H. pylori gastritis status post Prevpac therapy. 3. Morbid obesity currently undergoing bariatric evaluation for gastric bypass surgery by Dr. Green. PLAN: The patient will be scheduled for a repeat EGD in one year for surveillance purposes of Barrett’s esophagus. From a GI standpoint, we recommend to proceed with bariatric surgery. However, he will need to continue daily PPI administration to maximize acid reduction. there are no additional recommendations. Otherwise, Sample 4 PROGRESS NOTE PROBLEM: 1. Internal hemorrhoids confirmed via colonoscopy on January 28, 2010. 2. Chronic GE reflux disease. 3. History of intermittent diarrhea of unclear etiology. SUBJECTIVE: The patient was previously seen on February 25, 2010 for evaluation of chronic GE reflux disease. Subsequently, an EGD was performed on March 1, 2010 concluding a small hiatal hernia and gastritis from which biopsies were obtained. There is no evidence of peptic ulcer disease or neoplasm. Pathology findings document no evidence of Barrett’s esophagus or H. pylori infection. The patient returns today voicing that heartburn is well controlled with Nexium PPI therapy. However, he has developed recurrent intermittent loose stools, which is occurring sporadically. Recently he has developed right lower quadrant pain and nausea but no vomiting, fevers, chills or significant weight loss. He voices a very limited intake of dairy and caffeine products and denies administration of laxatives. A previous colonoscopy in January of 2010 revealed no evidence of colitis. REVIEW OF SYSTEMS: The patient’s review of systems questionnaire was reviewed and there are no additional pertinent positives. PHYSICAL EXAM: VITAL SIGNS: LUNGS: CARDIO: ABDOMEN: Blood pressure is 124/75. Temperature is 98.3. Current weight is 182 pounds. Clear to auscultation and percussion. S1, S2 within normal limits, without gallops or murmurs. Soft and nontender without organomegaly, mass or ascites. ASSESSMENT: 3. GE reflux disease, currently well controlled with PPI therapy. Upper endoscopy concluded no evidence of Barrett’s esophagus. 4. Intermittent loose stools of unclear etiology. Clinical features favor probable irritable bowel syndrome with diarrhea predominance versus increased stool frequency from dietary factors. PLAN: The patient will avoid dairy, caffeine and sorbitol. A trial of Bentyl antispasmodic therapy will be added for suspected irritable bowel syndrome. In addition, laboratory data to include celiac panel will be ordered. If clinical symptoms fail to improve, then a CT scan of the abdomen may be considered. Follow up in two weeks. Additional recommendations to follow. Sample 5 PROGRESS NOTE PROBLEM: 1. Rectal bleeding. 2. Anemia. SUBJECTIVE: The patient was previously seen for GI consultation on January 5, 2009 for evaluation of rectal bleeding and anemia. The patient was scheduled for a colonoscopy, but due to personal reasons the study has not yet been performed. She returns today with ongoing anemia but the most recent lab data is not available for review. In addition, less than a week ago she began having loose stools, but this appears to be improving. She voices no other GI-related complaints, without nausea, vomiting and/or evidence of active blood loss. She has no other comments or medical complaints. REVIEW OF SYSTEMS: The patient’s review of systems questionnaire was reviewed and there are no additional pertinent positives. PHYSICAL EXAM: VITAL SIGNS: LUNGS: CARDIO: ABDOMEN: Blood pressure is 100/58. Temperature is 96.1. Current weight is 187 pounds. Clear to auscultation and percussion. S1, S2 within normal limits, without gallops or murmurs. Soft and nontender without organomegaly, mass or ascites. ASSESSMENT: Microcytic anemia of unclear etiology with history of blood in the stools. This raises the suspicion for possible primary bowel source. Other possibilities include low H&H indices related to menorrhagia. PLAN: The patient will be scheduled for a colonoscopy. If endoscopic inspection of the lower GI tract is inconclusive, then a subsequent upper endoscopy and/or small bowel capsule study may be necessary. recommendations will follow. Further Sample 6 OUTPATIENT CLINIC NOTE VITALS BP 122/74, weight 239, pulse 84, temperature 98.6. PROBLEM 1. Recurrence of depression. 2. Med refills. SUBJECTIVE 1. Over the past year his orthopedic group had to cut back staff. He is now part-time, leading to quite a bit of financial stress. He called about six weeks ago to ask about restarting bupropion along with his fluoxetine. The reason for the addition was because he was having a hard time getting motivated, a harder time concentrating, decreased mood. On the bupropion he did definitely have more alertness, better concentration; however, he was also more irritable and having a harder time sleeping. When he is anxious it is more intense. Overall, it has not been that helpful this time around. He has currently been on fluoxetine for four years. Prior to that he had been on citalopram for eight years, which did well. We have decided to move him back to citalopram and drop the bupropion. 2. We reviewed his prescriptions. He needs a refill of Cialis, otherwise doing well. PHYSICAL EXAMINATION Alert, oriented, good eye contact, overweight. PHQ-9 is 11. PLAN 1. DC bupropion. 2. DC fluoxetine after a one-week overlap. 3. Citalopram 20 mg 1/2 daily, four days, then one daily. 4. Follow up in late June. Prior to that he will get his labs and we will make that visit a physical. Sample 7 OUTPATIENT CLINIC NOTE PROBLEM Follow up cold hands. SUBJECTIVE He saw a vascular surgeon who felt this was a variation of Raynaud's. No underlying vascular problems noted. He recommended considering a calcium channel blocker which might help this and also treat his blood pressure. Patient is overall doing well with the lisinopril, however, we both agree, this is certainly worth a try. PHYSICAL EXAMINATION VITAL SIGNS: BP 134/80. Weight 192. Height 5'11". GENERAL: Smiling, alert and oriented. EXTREMITIES: His hands are very warm today, warmer than mine. PLAN DC lisinopril. Start amlodipine 10 mg one daily. Start checking blood pressure every day and let us know if not in range. Otherwise follow up in a month and if this is working, will go with a mail order prescription. Sample 8 PROBLEM Acute gout, left great toe. SUBJECTIVE Patient has gone many years without gout. In the past it was episodic. He used indomethacin without any side effects. He is on indapamide but as noted, he goes many years between bouts. This was probably triggered by garden work which has done it in the past. Hiking is never a problem. Other problems are stable, continues being treated for blood pressure. He has had a prostatectomy for prostate cancer. PHYSICAL EXAMINATION VITAL SIGNS: BP 124/80. Weight 225. Temp 98.6. EXTREMITIES: Warmth, redness, tenderness left great toe primarily over the DIP. There is some warmth and redness along the instep of the foot as well. No sign of cellulitis, no entry wound to suggest spider bite, etc. PLAN 1. Indomethacin 50 mg t.id. with food, 30 prescribed which should last him for the next few episodes. 2. Set up labs for July which will include BMF, lipids, LDL, uric acid and because he was a bit anemic, postop prostatectomy will get CBC. He will also set a physical up for mid summer. Sample 9 OUTPATIENT CLINIC NOTE PROBLEM 1. Thoracic back strain. 2. Left forearm and elbow contusion and strain. 3. Changing psychiatric diagnosis, now PTSD and not bipolar. SUBJECTIVE 1. 1-1/2 weeks ago she was going too fast on her new hardwood floors in stockings and fell with both feet coming out. At the time no back pain but two days ago she developed a diffuse pain through the entire thoracic spine up to the upper scapular level, right and left, perhaps a bit more on the right but mainly in the midline. This is making it hard to move, hard to sleep. She is using ibuprofen 200 mg three t.id. Previously she used acetaminophen but it just did not help that much. No radicular symptoms with this. No change in bowel or bladder control. 2. On the same fall, she ended up catching herself on the couch and then landing on the left forearm. She is still sore diffusely from the elbow down to the radial side of the hand. No redness, swelling, deformity, numbness. Just an achy pain. 3. She has a new psychiatrist who based on her symptoms, past history, etc, decided she did not have bipolar but has PTSD. The lithium was stopped and her tremor is virtually gone. She is now just on fluoxetine 40 mg daily and working on cognitive therapy as well. PHYSICAL EXAMINATION VITAL SIGNS: BP 116/78. Weight 178 with shoes. Pulse 76. Temp 98.1. GENERAL: Patient is heavier, likely from the Lyrica. Alert and oriented, good eye contact. EXTREMITIES: The left hand, forearm and elbow are normal to inspection, slightly tender to palpation but nothing localizes. She still has supination, pronation, flexion and extension at the elbow. BACK: Normal to inspection except for some superficial acne. She is tender from about T-12 to about T-8 to palpate. No one vertebra, however, seems to be worse than the others. There is moderate tenderness in the soft tissue of the thoracic spine as well. Pain is aggravated by right rotation, not so much by left. No visible stepoff. IMPRESSION Most likely sprain from the fall although a little bit delayed. PLAN 1. Continue ibuprofen. GI warnings. 2. For more severe pain, especially at night, she can use hydrocodone/APAP 5/500, 30 prescribed. GI warnings given. She will use prune juice. 3. I reassured her this should all get better. 4. We discussed potentially getting an x-ray to look for compression fracture but I think the odds are low and we can do that later if she is not coming around. Keep her next month's follow up. Sample 10 Chart Note: Mary visited with this patient about his hip arthritis. He has been under the care of Dr. Muller. He has tried intraarticular injection downstairs under fluoroscopy and it apparently was not very successful. I am going to have him come and see me and we will try an intraarticular injection in the office upstairs. I will use a marker film with a paperclip over the hip, and then do the injection myself upstairs. At that point, we can visit some about what type of hip arthroplasty he might consider. Mary will work on setting this up. Sample 11 Chart Note: The patient showed up to clinic on Thursday 05/20/10. He was upset because he showed up an hour early and had to wait to be seen, and therefore left without being seen. I have called and tried to talk to him. I will continue to try and contact him and discuss how he is doing. Sample 12 Present Illness: The patient is status post two weeks from a left shoulder arthroscopy with capsular release and manipulation under anesthesia. Overall she has done well postoperatively. She presents today with no complications. She did have an allergic reaction to the prep that we did preoperatively in the operating room. She sustained a mild rash, but it is resolved since taking Benadryl and using hydrocortisone cream. There are no pustules or redness, and she has well healing portal sites on her left shoulder. Past Medical History: The patient’s past medical history was reviewed, updated, and filed in the Medical History tab in the chart. Examination: On physical exam, the patient is alert and oriented x 3. She is here today with her husband. Her sutures were removed. She has well healing portal sites on her left shoulder. There is no sign of erythema, drainage, or infection noted postoperatively. She has good range of motion. She has about 90 o of forward elevation on the left shoulder. She can externally rotate to approximately 15 o, and she can internally rotate to 15o on her left shoulder. Diagnosis: Status post left shoulder adhesive capsulitis and subacromial bursitis two weeks status post left shoulder arthroscopy and manipulation under anesthesia. Plan: The patient is here for re-evaluation of her left shoulder. She is two weeks out from a left shoulder arthroscopy with capsular release and manipulation under anesthesia. Overall she continues to do well postoperatively. She has well healing portal sites. There is no sign of any erythema, drainage, or postoperative infection. She did have a mild reaction to the prep preoperatively in the operating room. She is taking Benadryl and using hydrocortisone cream on that which is helping it to resolve. She was given a note in the office today to return to half days on May 20 through May 28, 2010, and then she can return to full duty on May 31, 2010, back to work. Overall if she continues to do well, I will see her back in four to six weeks for a follow-up or sooner if she is having problems. Sample 13 Present Illness: Beverly presents today as a 71-year-old woman with bilateral knee arthritis. Her problem is mainly patellofemoral in nature. She has difficulty going up and down stairs and getting up and down out of chairs. She has noticed some dramatic activity decrease secondary to this. The problem has been with her for 40 years. She does yoga which helps some. She has never had a lubricant shot or a steroid shot to treat this. Examination: Her physical exam is noted in the chart. Of note is that she is alert and oriented x 3. General skin exam is normal. No evidence of rashes, purpura, ecchymosis, etc. She has very slight valgus deformity of both knees. She does correct to neutral alignment with varus stress. Her range of motion is 0 to 135˚ in both knees. She has significant crepitus in her anterior compartment of her knee throughout her arc of motion. X-rays: Previous x-rays show significant patellofemoral arthritis and patellofemoral joint narrowing. Diagnosis: Bilateral patellofemoral arthritis. Plan: The plan is for conservative care. We are going to go with straight leg raising with weights, exercise bike, aquatics, etc., to try to increase her quad strength and then we will see her back as needed