NON r-TPA/Alteplase
advertisement

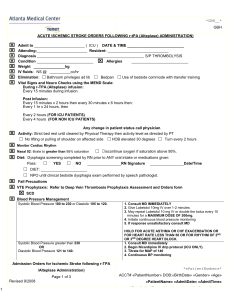
*GBH__* GBH ADMISSION ORDERS FOR TIA OR ISCHEMIC STROKE (NON r-tPA/Alteplase) Admit to ________________________ ( ICU / CVU) DATE & TIME ___________________________ Attending:________________________ Resident: _____________________________ Diagnosis ___________________________________________________ Condition ___________________________ Allergies ___________________________ Weight _______________kg IV fluids: NS @ __________ml/hr Elimination: □ Bathroom privileges ad lib □Bedpan □ Use of bedside commode with transfer training Vital Signs and Neuro Checks using the MEND Scale: Every 1 hr x 24 hours, then Every 2 hours (FOR ICU PATIENTS) Every 4 hours (FOR NON ICU PATIENTS) Any change in patient status call physician. Activity: Strict bed rest until cleared by Physical Therapy then activity level as directed by PT □ No lifting or pulling of shoulder on affected side Nasal 02: titrate to greater than 95% saturation □ Discontinue oxygen if saturation above 95% Diet: Dysphagia screening completed by RN prior to ANY oral intake or medications given: □ □ □ YES □ NO __________________RN Signature _______________Date/Time DIET: ______________________ NPO until clinical bedside dysphagia exam performed by speech pathologist. Fall Precautions VTE Prophylaxis: Refer to Deep Vein Thrombosis Prophylaxis Assessment and Orders Form Turn every 2 hours Monitor Cardiac Rhythm Pass: □ HOB elevated 30 degrees □ SCD Blood Pressure Management Systolic Blood Pressure greater than or equal to 220 OR Diastolic Blood Pressure greater than 120 on 2 or more consecutive BP checks at least 10 minutes apart contact House Officer IMMEDIATELY Initial Diastolic Blood Pressure greater than 140 1. Consult MD IMMEDIATELY 2. Give Labetolol 10mg IV over 1-2 minutes. 3. May repeat Labetolol 10 mg IV or double the bolus every 10 minutes for a MAXIMUM DOSE OF 300mg. 4. OR begin Nicardipine IV drip protocol (ICU only) 5. Initiate continuous blood pressure monitoring 6. If response unsatisfactory consult MD HOLD LABETOLOL FOR ACUTE ASTHMA OR CHF EXACERBATION OR FOR HEART RATE LESS THAN 50 OR FOR RHYTHM OF 2ND OR 3RD DEGREE HEART BLOCK. 1. Consult MD immediately 2. Begin Nicardipine IV drip protocol 3. Titrate for MAP of 140 4. Continuous Blood Pressure Monitoring Admission Orders for TIA or Ischemic Stroke (NON r-TPA/Alteplase) Page 1 of 3 Revised 9/2008 1 *«PatientNumber»* ACCT# «PatientNumber» DOB:«BirthDate» «Gender» «Age» «PatientName» «AdmitDate» «AdmitTime» MR#«MedicalRecordNumber» «AttendingDoctorName» *GBH__* GBH ADMISSION ORDERS FOR TIA OR ISCHEMIC STROKE (NON r-tPA/Alteplase) For Diabetic patients: Check blood glucose before each meal and at HS. If blood glucose is greater than 140 on two consecutive readings call House Officer for instructions. Notify physician of ALL admission blood glucose greater than 140. Consult PT, OT, ST for evaluation and treatment upon admission. Consult Nutrition Services for evaluation and dietary education. Consult Case Management for discharge planning. Notify Stroke Coordinator (5-4243). Consult Stroke Educator for Stroke Education (5-4613). Provide Stroke Education: Types of Stroke, Complications, Personal Modifiable Stroke Risk Factors, Stroke Warning Signs and Symptoms; FAST; How to Activate EMS:911; Need for Follow up after Discharge; Prescribed Medications; Smoking Cessation; Heart Healthy Diet Diagnostics to be performed in AM: □ □ □ □ □ □ MRI Brain & MRA Brain and Neck without contrast: Stroke protocol MRI Brain without contrast, without MRA Dx: Stroke CT of Brain without contrast for stroke, (patient cannot have MRI) Carotid Duplex Ultrasound for Dx: Stroke Echocardiogram for Dx: Stroke: Dr. ____________________ to read. CTA brain and neck for Dx: Stroke Medications □ □ r-tPA (Alteplase) not indicated due to __________________________________ ANTIPLATELET THERAPY □ NOT INDICATED DUE TO ____________________________________________________ □ □ □ Aspirin 81 mg po daily □ Lorazepam 1 mg IV every 20- 30 minutes prior to imaging procedure for agitation. May repeat X ______ □ STATIN: _______________________________________________ Aggrenox 1 capsule po BID □ □ Coumadin ______mg po Daily Aspirin 325 mg po daily Plavix 75 mg po daily □ PT/INR daily □coumadin Education (Consider Statin for LDL greater than or equal to 100mg/dL; For Diabetic patients LDL greater than 70) □ □ □ ACE Inhibitor: _____________________________________________________ Thiazide Diuretic: _________________________________________________ Laxative: _________________________________________________________ Admission Orders for TIA or Ischemic Stroke (NON r-tPA/Alteplase) Page 2 of 3 Revised 9/2008 2 *«PatientNumber»* ACCT# «PatientNumber» DOB:«BirthDate» «Gender» «Age» «PatientName» «AdmitDate» «AdmitTime» MR#«MedicalRecordNumber» «AttendingDoctorName» 3 *GBH__* GBH ADMISSION ORDERS FOR TIA OR ISCHEMIC STROKE (NON r-tPA/Alteplase) □ □ □ Phenergan 12.5 mg PO/IV (diluted in 50 ml normal saline) every 4 hours PRN nausea Acetaminophen 1000 mg PO/PR every 4-6 hours PRN temp greater than 101.5 or for headache NOT TO EXCEED 4 GRAMS DAILY Other Medications: ________________________________ ________________________________ _________________________________ _________________________________ __________________________________ □ □ □ □ □ □ □ □ Labs: CBC w/diff, Platelets, PT/PTT/INR Basic Metabolic Profile □ □ □ Daily Daily Daily CKMB, Troponin every 8 hrs x 3 Fasting Lipid Profile (if not already done) Hgb A1C (if not already done) □ Urine C&S _____________ UA □ □ 2 Hour Glucose Tolerance Test ____________ □ _______________ Pneumovax Vaccination Protocol Consult: ______________________________________________________ Consult: _______________________________________________________ □ Verbal orders read back x 1 and verified. □ Telephone orders, read back x 2, and verified. MD SIGNATURE:___________________________________________________________ _________________ DATE & TIME Admission Orders for TIA or Ischemic Stroke (NON r-TPA/Atleplase) Page 3 of 3 Revised 9/2008 4 *«PatientNumber»* ACCT# «PatientNumber» DOB:«BirthDate» «Gender» «Age» «PatientName» «AdmitDate» «AdmitTime» MR#«MedicalRecordNumber» «AttendingDoctorName»