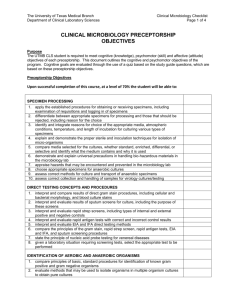
CLINICAL MICROBIOLOGY PRECEPTORSHIP
advertisement

CLINICAL MICROBIOLOGY OBJECTIVES Purpose The student is required to meet cognitive (knowledge), psychomotor (skill) and affective (attitude) objectives of each preceptorship. This document outlines the cognitive and psychomotor objectives for microbiology. AFFECTIVE OBJECTIVES: 1. Demonstrate initiative by reviewing objectives, theory and procedures prior to and regularly through out the rotation. 2. Demonstrate professionalism by: a. Report to clinical time on all scheduled days at assigned times b. Notify clinical preceptor as soon as possible of anticipated tardy. c. Notify clinical preceptor and MLT faculty of absence at least 30 minutes prior to scheduled arrival time. d. Use cell phones and MP3 only during designated break times, NEVER in the clinical laboratory. e. Ask permission to use the phone for personal reasons. Limit personal phone calls to once per shift and less than 3 minutes. 3. Demonstrate enthusiasm and interest in the profession of clinical laboratory science. 4. Demonstrate an understanding of the concepts underlying clinical laboratory tests. 5. Use time in the clinical laboratory effectively to maximize productivity and learning. 6. Offer to help with the work load of the clinical laboratory when appropriate. 7. Use instructional guidance and constructive criticism to correct deficiencies and improve performance. 8. Work cooperatively with clinical preceptors, other laboratory personnel and other health care professionals. 9. Demonstrate the ability to concentrate and avoid distractions while performing laboratory work. 10. Perform laboratory work independently and without distractions. 11. Follow written and verbal instructions. 12. Perform laboratory work with accuracy, efficiency and precision. 13. Communicate in a clear and concise manner and record data accurately and legibly. 14. Recognize report and resolve problems that may arise and take appropriate corrective action. 15. Demonstrate diligence in working through and resolving problems. 16. Assure that the laboratory work area is clean and well stocked. 17. After appropriate time and training, perform laboratory work with organization, accuracy, efficiency, precision and confidence. 18. Complete work on time and meet deadlines for assignments. 19. Maintain the confidentiality of patient information. 20. Follow all safety guidelines of the MLT program and clinical site. 21. Conform to the clinical dress code. 22. Conform to the ASCLS Code of Ethics. Objectives The student shall demonstrate the ability to: Safety 1. Use appropriate personal protective equipment at all times when working with patient samples. 2. Locate all fire extinguishers, eye wash stations and safety showers. Austin Community College Revised 5/2012 3. Locate Materials Safety Data Sheets, chemicals carcinogens list, and hazardous chemicals list. SPECIMEN PROCESSING 1. Apply the established procedures for obtaining or receiving specimens, including examination of requisitions and logging in of specimens. 2. Differentiate between appropriate specimens for processing and those that should be rejected, including reason for the choice. 3. Identify and integrate reasons for choice of the appropriate media, atmospheric conditions, temperature, and length of incubation for culturing various types of specimens. 4. Explain and demonstrate the proper sterile and inoculation techniques for isolation of microorganisms. 5. Compare media selected for the cultures, whether standard, enriched, differential, or selective and identify what the medium contains and why it is used. 6. Demonstrate and explain standard precautions in handling bio-hazardous materials in the microbiology lab. 7. Review hazards that may be encountered and prevented in the microbiology lab. 8. Choose appropriate specimens for anaerobic cultures. 9. Evaluate correct methods for culture and transport of anaerobic specimens. 10. Evaluate correct collection and handling of samples for virology cultures/testing, if applicable. QUALITY CONTROL AND QUALITY ASSURANCE 1. Perform and report results of quality control. 2. Use CLSI guidelines for quality control in microbiology to determine compliance. 3. Apply quality assessment programs to ensure the validity of tests. 4. Perform, report, and evaluate preventive maintenance of instruments. 5. Detect instrument malfunctions and take appropriate action. TESTING CONCEPTS AND PROCEDURES 23. Interpret and compare results of direct gram stain procedures, including cellular and bacterial morphology, and blood culture stains. 24. Interpret and evaluate results of sputum screens for culture, including the purpose of these screens. 25. Interpret and evaluate rapid strep screens, including types of internal and external positive and negative controls. 26. Interpret and evaluate rapid antigen tests with correct and incorrect control results. 27. Interpret and evaluate EIA and IFA direct testing methods, if applicable. 28. Compare and contrast the principles of the gram stain, rapid strep screen, rapid antigen tests, EIA and IFA, and sputum screening procedures. 29. Given a laboratory situation requiring screening tests, select the appropriate test to be performed. IDENTIFICATION OF AEROBIC AND ANAEROBIC ORGANISMS 1. Compare and contrast principles of basic, standard procedures for identification of known gram positive and gram negative organisms. 2. Evaluate methods that may be used to isolate organisms in multiple organism cultures to obtain pure cultures. 3. Evaluate aerobic cultures and determine what constitute normal flora and potential pathogens from various sources and types of specimens. 4. Examine and compare the significance of bacterial colonies on primary plating media and describe appearance and hemolytic patterns on blood agar and appearance on MacConkey agar. 5. Select, perform, and give the principle of tests needed for identification of isolated organisms, based upon colonies observed on primary plating media. Austin Community College Revised 5/2012 6. Perform and evaluate methods of colony counts and identification procedures on urine cultures and explain the significance of results obtained. 7. Discuss the importance of reporting the isolation and identification of clinically significant organisms to the proper professional(s), such as TDH or Infection control. 8. Compare and contrast different systems for achieving anaerobic conditions. 9. Evaluate the appearance of colonies growing anaerobically on media used for primary isolation of anaerobes, and select appropriate identification testing. 10. Compare and contrast methods used for the identification of anaerobes. 11. Identify anaerobes that are considered endogenous and/or pathogenic by body site. 12. Discuss appropriate identification techniques for Clostridium difficile. ANTIMICROBIAL SUSCEPTIBILITY 1. Use CLSI guidelines on susceptibility testing to ensure compliance. 2. Compare and contrast disk diffusion, MIC, and MBC methods for susceptibility testing, where applicable. 3. Select the appropriate method for susceptibility testing considering the type and origin of the organism. 4. Observe, perform, and evaluate results of automated methods for susceptibility testing. 5. Evaluate causes of development of antibiotic resistance. 6. Evaluate mechanisms of antibiotic action on the bacteria. 7. Evaluate antibiotic susceptibility and appropriate reporting of susceptibility testing for infections caused by specific types of organisms. Reference Laboratory Send-Out 1. Using reference laboratory procedure manuals, process specimens for transport, where applicable. OPTIONAL PROCEDURES (as available at the clinical site) MYCOBACTERIOLOGY 1. Describe the principle of and perform the concentration-digestion and decontamination methods for acid-fast organisms. 2. Choose appropriate media, incubation conditions, and length of time for growth of the commonly occurring mycobacteria. 3. Compare and contrast acid-fast (such as Kinyoun) and fluorescent staining techniques. 4. Perform and interpret acid-fast and/or fluorescent staining for Mycobacteria. 5. Compare grouping of Mycobacteria other than tuberculosis (MOTT) and tuberculosis to determine relationships. PARASITOLOGY 1. State the principle of the formalin/ethyl acetate concentration method for specimen processing and explain the sources of error and limitations. 2. Design a proper collection technique for pinworms to optimize recovery of the organism. 3. Demonstrate calibration of the ocular micrometer for production of a conversion chart for sizing parasites. 4. Perform a concentration procedure to prepare a specimen for ova and parasite examination. 5. Prepare and examine wet preps for Ova and Parasites. 6. Prepare and examine smears for blood and tissue parasites. 7. Prepare and examine special stains for Cryptosporidium and Cyclospora. 8. Compare and contrast staining procedures for malaria and other parasites found in blood or body fluids. Austin Community College Revised 5/2012 9. Select quality control, quality assurance and preventive maintenance procedures to ensure the validity of tests. 10. Given pictures, slides, or other representations of trophozoites, cysts and/or ova, correctly identify the organism. 11. Differentiate and identify specific nematode infections based on clinical symptoms and laboratory findings. 12. Differentiate and identify specific cestode infections based on clinical symptoms and laboratory findings. 13. Differentiate and identify specific trematode infections based on clinical symptoms and laboratory findings. 14. Differentiate and identify protozoan infections based on clinical symptoms and laboratory findings. MYCOLOGY 1. Differentiate between contaminant and pathogenic fungi by examining fungal cultures. 2. Identify fungi in slide culture, wet preps, LPCB preparations or from pictures, slides or other representations. 3. Compare and contrast commercial yeast identification methods. 4. Identify and state the principle of basic tests used to identify fungi and yeasts. VIROLOGY 1. Apply established procedures for obtaining or receiving specimens, including examination of requisitions and logging in of specimens. 2. Differentiate between appropriate specimens for processing and those that should be rejected, including reason for the choice. 3. Identify and integrate reasons for choice of the appropriate media, atmospheric conditions, temperature, and length of incubation for culturing various types of specimens. 4. Compare and contrast principles of basic, standard procedures for identification of common viruses. 5. Differentiate and identify specific viruses based on cytopathic effects. Austin Community College Revised 5/2012