CHAPTER 1 Infection
advertisement

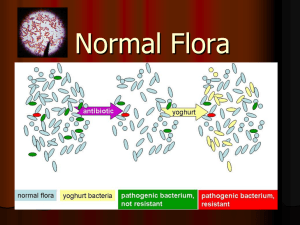
CHAPTER 1 Infection The science of medical microbiology dates back to the pioneering studies of Pasteur and Koch, who isolated specific agents and proved that they could cause disease by introducing the experimental method. These efforts, combined with work begun by Semmelweis and Lister, which showed how these diseases spread, led to the great advances in public health that initiated the decline in disease and death. In the first half of the 20th century, scientists studied the structure, physiology, and genetics of microbes in detail and began to answer questions relating to the links between specific microbial properties and disease. By the end of the 20th century, the sciences of molecular biology, genetics, genomics, and proteomics extended these insights to the molecular level. These gradually extended from bacterial diseases to fungal, parasitic, and finally viral infections. Almost as quickly, virtually all categories of infectious agents developed resistance to all categories of antimicrobics to counter these chemotherapeutic agents. THE INFECTIOUS AGENTS: THE MICROBIAL WORLD 1. Microbes are small 2. Most play benign roles in the environment 3. Products of microbes contribute to the atmosphere 4. Increasing complexity: viruses → bacteria → fungi → parasites I. Viruses 1. 2. 3. 4. 5. 6. Viruses are strict intracellular parasites of other living cells Contain little more than DNA or RNA Most have a protein coat over their nucleic acid Sometimes a lipid surface membrane is derived from the cell they infect. Replication is by control of the host cell metabolic machinery Some integrate into the genome II. Bacteria 1. 2. 3. 4. The smallest living cells Cytoplasmic membrane surrounded by a cell wall Interwoven polymer called peptidoglycan makes the wall rigid. Cytoplasm contains only ribosomes and a single, double-stranded DNA chromosome 5. 6. 7. All the chemical elements of nucleic acid and protein synthesis are present Divide by binary fission and can be grown in artificial culture Prokaryotic cell plan lacks nucleus and organelles like mitochondria III. Fungi 1. 2. 3. 4. 5. Fungi exist in either yeast or mold forms. Similar in size to bacteria, but most are larger Grow as yeasts or molds and multiply by budding. Molds form tubular extensions called hyphae Eukaryotic and have a rigid external cell wall composed of polymers, called glucan, mannan, and chitin. 6. Replicate by meiosis or mitosis. 7. Most are free-living and widely distributed in nature IV. Parasites 1. Range from unicellular amoebas to multicellular tapeworms 2. Individual cell plan is eukaryotic 3. Worms have their own organ systems and microscopic egg or larval stages 4. Life cycles may involve multiple vertebrate and invertebrate hosts The Normal Microbial Flora 1. Flora may stay for short or extended periods 2. If pathogens are involved the relationship is called the carrier state 3. Balance is the desired state I. Origin and Nature 1. 2. 3. 4. Initial flora is acquired during and immediately after birth Physiologic conditions such as local pH influence colonization Adherence factors counteract mechanical flushing Ability to compete for nutrients is an advantage II. Normal Flora at Different Sites A. Blood, Body Fluids, and Tissues 1. Tissues and body fluids such as blood are sterile in health 2. Transient bacteremia can result from trauma B. Skin 1. Propionibacteria and staphylococci are dominant bacteria 2. Skin flora is not easily removed 3. Conjunctiva resembles skin C. Intestinal Tract 1. 2. 3. 4. Oropharynx has streptococci and Neisseria Stomach and small bowel have few residents Small intestinal flora is scanty but increases toward lower ileum Adult colonic flora is abundant and predominantly anaerobic predominantly members of the genera Bacteroides, Fusobacterium, Eubacterium, and Clostridium 5. Other colonic flora is composed of facultative organisms such as Escherichia coli, enterococci and yeasts 6. Diet affects species composition D. Respiratory Tract 1. Nasopharynx is often the site of potentially pathogenic organisms such as pneumococci, meningococci, and Haemophilus species. 2. S. aureus is carried in anterior nares 3. Lower tract is protected by mucociliary action E. Genitourinary Tract 1. Bladder and upper urinary tract are sterile 2. Hormonal changes affect the vaginal flora 3. Use of epithelial glycogen by lactobacilli produces low vaginal pH III. Roles in Health and Disease A. Opportunistic Infection 1. Flora that reach sterile sites may cause disease 2. Compromised defense systems increase the opportunity for invasion 3. Mouth flora plays a major role in dental caries B. Exclusionary Effect 1. Competing with pathogens has a protective effect 2. Antibiotic therapy may provide a competitive advantage for pathogens C. Priming the Immune System 1. Organisms of the normal flora play an important role in the development of immunologic competence 2. Sterile animals have little immunity to microbial infection 3. Low microbial exposure correlates with asthma risk D. Promoting “Good” Flora 1. Probiotics promote colonization with "good" flora such as lactobacilli in the intestinal tract. 2. Certain intestinal lactobacilli may protect against diarrheal agents INFECTIOUS DISEASE 1. Pathogens are just a tiny part of the microbial world 2. Degrees and mechanisms of virulence vary greatly I. EPIDEMIOLOGY 1. 2. 3. 4. Each agent has its own reservoir, mode of spread, and target population Poor socioeconomic conditions foster infection Elements of modern society may facilitate spread Anthrax and smallpox are new bioterrorism threats II. PATHOGENESIS 1. Pathogenicity is multifactorial involving sequential steps 2. Pathogens have surface molecules that bind to host cells 3. Invasion is specialized and requires adaptation to new environments 4. The inflammatory response to the pathogen can itself cause injury 5. Toxins may destroy cells or alter their function III. IMMUNITY 1. For each pathogen, the primary interest is whether there is natural immunity and, if so, whether it is based on cell-mediated or humoral (antibody) mechanisms 2. Evading the immune response is a major feature of virulence 3. Knowing the molecule against which the protective immune response is directed is particularly important for devising preventive vaccines IV. CLINICAL ASPECTS OF INFECTIOUS DISEASE A. MANIFESTATIONS 1. Fever, pain, and swelling are the universal signs of infection 2. Body system(s) involved dictate clinical findings 3. Cough, diarrhea, and mental confusion represent disruption of three different body systems B. DIAGNOSIS 1. Growing disease-causing microbes in culture is preferred when possible 2. Many agents can be seen and identified by microscopy 3. Specific antibodies directed against the pathogen may be diagnostic 4. Molecular methods detect toxins or virulence genes C. TREATMENT 1. Antibiotics are directed at structures or metabolic processes of bacteria not present in host 2. Antivirals target viral entry and unique virus-coded enzymes 3. Resistance to antimicrobial agents complicates therapy 4. Resistance mechanisms include mutation of the target, inactivation of the antimicrobial, and development of alternate metabolic pathways 5. Genetic mechanisms allow spread of resistance D. PREVENTION 1. Public health measures and immunization are primary preventive measures 2. Live vaccines use attenuated organisms that do not produce disease but still stimulate a protective immune response. 3. Rarely live vaccines can cause disease 4. Purified components of killed pathogens produce safe vaccines 5. Vaccines can be genetically engineered