The Integration of Meditative Techniques Into a Traditional
advertisement

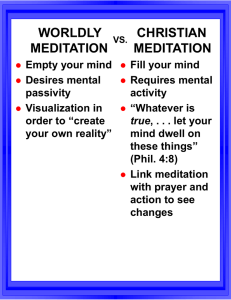
FOCUS: East/West Clinical Practice The Integration of Meditative Techniques into a Traditional Psychotherapy Practice By Helen J. Rosen, Ph.D. Better than if there were thousands of meaningless words is one meaningful word that on hearing brings peace. -Dhammapada, translated by Thanissaro Bikkhu, 1998 Looking back on over 30 years in private practice, I see more clearly than ever my underlying motivation for this work: the strong desire to alleviate suffering, both in myself and in others. As is true for all of us who have dedicated ourselves to this field, that desire surely was (and still is) multidetermined, containing a mixture of both selfish and self-less concerns. Nonetheless, it is what I wanted to do and I devoted myself to developing the professional skills as well as the personal attributes that would make me effective in helping people to feel better. With that in mind, then, I largely pursued what seemed at the time to be the most sophisticated avenue for understanding why we suffer, namely a psychoanalytic or psychodynamic point of view. After completing my doctoral degree, I entered psychoanalytic training as well as the required (and desired) personal analysis. That foundation of theory and understanding became the building blocks for my work and, for the most part, I found that the psychodynamic approach made sense to me and often seemed to help those I treated. Over time, the combination of the therapeutic relationship, insight into the psychodynamics of the individual’s symptoms and some degree of analysis of the transference, brought a measure of relief to many of the individuals who walked through my door. Yet, the results often took a long time to achieve, and were not universal among my clients. Though I understand that we cannot help everyone, the failures I experienced, as well as the patience required for the psychodynamic approach to take hold, were continued factors motivating me to seek, explore and be open to other ways of understanding human suffering. I became interested in exploring alternative ways of understanding human pain. Early in 2000, I began research for a paper that would look at alternate mythologies for understanding female development (eventually published as “Patriarchy, Culture and the Use of Greek Mythology in Psychoanalysis”, Psychoanalysis and Psychotherapy, Spring, 2007). In the course of that research, I was directed by a friend to look at a female deity well-known in Tibetan Buddhist literature, the “dakini”. A dakini is a feisty female deity who can disguise herself as an old hag. If she meets a man who is kind to [1] her even though she is old and ugly, she has the power to convey instant enlightenment upon him. My research led me to other female mythologies as well, though none which would have the same effect on me as learning about dakinis. Shortly after I began familiarizing myself with the literature on dakinis, I also became aware of a local Tibetan Buddhist meditation center. I decided that if I were going to write about dakinis in my paper, I should at least have a bit more experience with Tibetan Buddhism in general. One Sunday morning I went to the center for a meditation session and had a totally unexpected experience of bliss as I sat for the very first time attempting to meditate. That experience convinced me that there was something worth pursuing in meditation and I have been following the “path” ever since. Though my orientation to Buddhism has changed since that time (I now practice “vipassana” or insight meditation rather than Tibetan), I have not wavered in my strong belief that meditation and the Buddhist path have a tremendous amount to offer those of us who are looking for ways to alleviate pain. Meditation and Psychotherapy Along with experiencing a great deal of initial excitement and curiosity regarding meditation as a path to alleviate suffering, I also became aware fairly quickly of internal conflict regarding the integration of meditation and psychodynamic practice. Psychotherapy is about understanding the content of the mind, meditation is about watching the processes in the mind. From a psychoanalytic point of view, the content of the mind holds a high degree of importance (along with other factors, such as the repetition compulsion as played out in the transference, etc.), but in Buddhist psychology, thoughts are, for the most part, “papanca”, or mental proliferation. It doesn’t matter what the thoughts are, all that really matters is knowing that you are thinking. It took me a few years before I could see compatibility in the two approaches and how I could incorporate one without invalidating the other. It was, of course, helpful to read what had already been published by the pioneers in psychotherapy and meditation. Mark Epstein’s Thoughts Without a Thinker (1995) and a collection of essays published as The Couch and the Tree (1998) presented early groundbreaking approaches towards synthesizing western and eastern treatment models, as was Jeffrey Rubin’s Psychotherapy and Buddhism (1996). These books heralded the beginning of an embrace of eastern psychology, especially that branch of Buddhist psychology that advocated the practice of what is called mindfulness meditation, by growing numbers of western trained mental health professionals. Though still a small percentage of psychotherapists overall, attendance at workshops and conferences on mindfulness meditation for psychotherapists appears to be brisk and the practice of meditation among psychotherapists seems to be growing as well In my own practice I began introducing mindfulness or meditation-based ideas after I had been practicing meditation for a number of years. While I was initially drawn to the concepts of Buddhist psychology and wanted to use them in my work, I subsequently came to see that most clients simply wanted to feel better as quickly as possible. With experience I was able to discern techniques and tools from meditation practice were helpful, and surprisingly to me, it was not necessary for clients to meditate in order to derive benefit from these tools. I have increasingly introduced certain techniques drawn from the practice of mindfulness (also called “insight”) meditation into my work with clients suffering from anxiety and depression. In the remainder of this paper I will summarize some of these treatments and how the use of meditation-based techniques, either alone or in conjunction with traditional psychodynamic psychotherapy, brought about improved well-being in the clients that I worked with in my private practice. [2] Brief Treatment of Anxiety Using “Noting” John D. was 32 years old when he began treatment with me for anxiety. He reported that he had experienced his first anxiety attack approximately 6 months after the attack on the Twin Towers in New York when he was traveling in a foreign (non-European) country with his wife. He stated that he woke up in his hotel room his first day on this vacation and felt dizzy, frightened and weak. He did not leave the hotel room that day. He realized that it was anxiety and was able to gradually leave the hotel room for short periods of time as long as he stayed close to the hotel. He reported that he felt afraid of getting lost, afraid of being attacked, and afraid that something unexpected would happen that he would be unable to handle. He managed to stay for the intended vacation but was immensely relieved when he and his wife returned home. Since that time, he had experienced anxiety on the infrequent trips he took within the States. One weekend he was away in another state with friends from college and he excused himself by telling his friends that he was sick and returned home early. His motivation for starting treatment was that he again had another short trip scheduled to meet these same male friends in another state in approximately 6 months. He wanted to be able to enjoy himself, was embarrassed for his friends to find out he was anxious, and was hoping that treatment would help him overcome his anxiety so that he could travel and enjoy the time away. John stated that though the panic attack that occurred while he was abroad was his first, he felt that he had always been a somewhat anxious man. He felt that he worried too much about the future. Though he had a relatively secure job, he worried that his boss would feel he was inadequate and would fire him. He had some fears that his wife would leave him. When questioned about family history, John stated that he believed his parents were both anxious people however it was never discussed openly in the family. They did not travel and in general led fairly quiet lives. He was an only child. John had been drawn to me for treatment having read online that I was interested in meditation and spirituality. He had meditated briefly in college and thought he might want to try it again. He had avoided therapy in the past because he did not want to spend “years” (as he put it) going back and re-experiencing his past. Before ending the first session, I pointed out to John the obvious relationship between his anxiety attack, the fears he developed on his trip abroad, and the attack on the Twin Towers. Though he could see intellectually that there might have been a connection, he did not particularly resonate with that perception. After further exploration of the circumstances of his anxiety attack(s) in the second session, I explained to John a practice called “noting”, which mindfulness meditators learn to do while sitting on the cushion. In this practice, one notices his/her thoughts (or feelings, or perceptions) and “notes” them to oneself. So while one is meditating, when a thought arises the meditator comments to him/herself “thinking…thinking” and then gently tries to return to the object of meditation, usually the breath. Joseph Goldstein describes the technique of “noting”, when practiced during meditation, this way: Noting should be done very softly, like a whisper in the mind, but with enough precision and accuracy so that it connects directly with the object. For example, you might label each breath, silently saying in, out or rising, falling. In addition, you may also note every other appearance that arises in meditation. When thoughts arise, note thinking. If physical sensations become predominant, note pressure, vibration, tension, tingling, or whatever it might be. If sounds or images come into the foreground, note hearing or seeing. (p. 35) [3] After briefly describing the practice of “noting” to John, I asked John to observe himself throughout the week, and if he found himself worrying, or having any kind of anxious thought, to “note” it, giving it any label he preferred. The instructions were not to try and change the thoughts, or get rid of the thoughts, but simply to “note” the thoughts and if possible move on. I stressed the importance of trying not to criticize himself for having the anxious thoughts. As I always do when I give these instructions, I demonstrated to him the tone of voice (which obviously can’t be demonstrated in writing here) I wanted him to try and achieve – a kind of “Oh, isn’t that interesting…I’m having another one of those thoughts!”, rather than the usual way we react to those kinds of thoughts – “What’s wrong with me? Why do I worry so much? I have to stop this. Why can’t I stop this? Etc. etc.” As part of the preparation and support that I give in the beginning of treatment for anxiety, I explain the difference between fear (when there is something actual to be afraid of) and anxiety (where there is not). I might talk about anxiety as a “mis-firing” of the fear response in the brain. And I tell patients that they cannot stop their brains from producing anxious thoughts, but they can stop themselves from taking the anxious thoughts “seriously”. Most anxious individuals resonate very quickly with that idea, because they have been trying for years to stop having the thoughts and they have been unsuccessful. I might even say to them “Well, if all it took was stopping having the anxious thoughts you would already have done that, right? You’ve been trying to do that and it hasn’t worked.” They universally agree. Sometimes I suggest the idea that the thought is like a bus going by you on the street. You can see the bus, and notice the bus, but you don’t have to get on the bus. The main elements are to recognize and label the thoughts and to begin to develop a different relationship to the anxiety symptoms. In this approach to treating anxiety, these elements are built upon in each of the succeeding sessions. Depending on how quickly the patient responds and how interested he or she is, I might talk about the impermanence of all feelings and thoughts, being in the present moment vs. mental “time travel”, i.e. thinking endlessly about the future or returning endlessly to the past. We might talk about how feelings and thoughts change, and therefore don’t really define who we are. In the third session, the first following his instructions to note his anxious thoughts, John reported two very common reactions to the task: first, he said he was surprised to notice how many anxious thoughts he had throughout the day, and second, he reported that he was feeling better. John reported walking down the street in Philadelphia in front of a hotel that had an awning held by metal rods to the front of the building. He said that whenever he found himself walking under that particular awning he had worried that the rods would break and the awning would fall on him. Having noted to himself the worried thought, he reported that it didn’t seem to bother him as much. At this point, John stated that he was interested in trying to meditate again. I encouraged him to start with only 5 minutes a day, as it has been my experience that individuals who try to start meditating for longer periods of time quickly become discouraged and quit. I also instructed him briefly in mindfulness meditation, i.e., rather than trying to clear his mind of thoughts, he would try to do exactly what he had already being doing in his daily life, that is, notice and “note” when he was thinking and then return to focusing on the “breath”. I try to point out to patients that it is exactly the same thing in either situation. His mind will produce thoughts and his job is to notice that he is thinking. That’s all. In the fourth session, John continued to report progress in noticing his thoughts and now we spoke about “letting them go”. He had been able to meditate a few times during the week and found it calming. He was beginning to feel more confident that he could “control” his anxiety better. He had a weekend [4] coming up where he was not going far – to a bed and breakfast in the state with his wife – but he thought it might help give him a measure of how well the “noting” would work in a stressful situation. We practiced the meditation and “noting” for a few minutes in the session, and he made an appointment for another session in a few weeks, after the weekend away with his wife. When we met for the last time, he reported that he had only had brief moments of anxiety on the weekend and had been able to note them and they seemed to diminish. His enjoyment of the weekend had not been impaired. John now reported that he felt prepared to tackle more extensive travel and that he was no longer fearful about his trip in the fall. At that session, he terminated treatment, with the understanding that should his weekend with his friends not go well, or should he feel uncomfortable anxiety again, he would return for more sessions. Combined Treatment of Depression Carol T. was a 47 year old single woman who began therapy following her layoff from an administrative job that she had held for many years. Carol knew that she had been laid off as part of a general downsizing at her company; however she felt that she was suffering nonetheless from low selfesteem as a result of losing her job. Through a combination of inheritance and careful real estate investments, Carol found herself able to take a year or more off from work during which time she hoped to figure out where she wanted to go in terms of future employment. She also felt that she was unable to apply for jobs and go on job interviews in her current state of mind. Carol had been raised in a middle-class suburb, the only girl of three siblings, both neglected and over-protected by her mother. She reported that she never heard her mother say “I love you”, however, her mother would not let her ride a bicycle for fear of Carol hurting herself. Carol had been an excellent student, and had been accepted into a philosophy doctoral program following receiving her bachelor’s degree. However, her parents were unwilling to help her financially so that she could attend the program, and Carol lacked the confidence to try and do it on her own. Instead, she gave up her dream of pursuing her interest in philosophy and became an administrative assistant. In the intervening years, Carol had been successful in her work and had received promotions and raises. At the time of her first consultation with me, she no longer had an interest in philosophy or in furthering her education. The main symptoms that Carol reported initially were that she had difficulty getting out of bed in the morning, and that she was very self-critical. She also reported feeling very insecure and frightened when she had to deal with contractors, repairmen and others connected with maintaining her properties. In fact, Carol owned one property that was in considerable disrepair, and she was finding it very difficult to arrange for the repairs, while at the same time she worried about the neighbors anger at her for the state of the property. Carol began therapy while already on a course of anti-depressants. Initially, Carol was most concerned about her inability (as she expressed it) to get out of bed promptly in the morning. Her hypercritical attitude came out in full force as she talked about how she wasted a good part of each day sleeping late or at least lolling about in bed. When questioned, however, she did state that if she had somewhere to go, she never missed an appointment to stay in bed. The problem occurred mostly when she had no plans for that day. At the time I first saw Carol, she had been out of work for about 2 months. My first “mindfulness”-based intervention with Carol, therefore, focused on her so-called inability to get out of bed in the morning. There is an often-quoted saying in Buddhism: “Pain is inevitable, but suffering is optional.” This statement refers to the fact that there will always be unwanted, undesirable [5] and painful aspects in life – they are inevitable. But the stories that we weave around those events, and which compound the suffering enormously, are optional. Frequently those stories are what we, with regard to psychodynamic theory, would call aspects of a harsh superego – self-criticism, self-blame, and a sense of failing to live up to one’s own expectations for oneself. For Carol, it was second nature for her to beat herself up emotionally for failing to be more productive. As I had with John, I pointed out to Carol that her self-criticism had not been particularly helpful in getting her to change her behavior, so I suggested that she notice and “note” whenever self-critical thoughts arose concerning whatever time it was that she got up in the morning. She was instructed to note the thoughts, label them however she chose, and then try and move on. Contained in the saying “Pain is inevitable but suffering is optional” is also the idea that fighting the experience of pain does not help us cope with it. In a counter-intuitive way, we are better able to work with painful situations when we are able to be attentive and stay “with” the pain, seeing it for what it is, not what we fearfully expect it to be. Carol had built a highly negative story around her “morning” problem. Her staying in bed was depression, yes, but it was also laziness and lack of motivation. What she really needed was someone to give her a good kick in the butt! I suggested to Carol that we didn’t really know what her morning behavior meant, and that perhaps it wasn’t exactly what she thought it was. I gave Carol the assignment of trying to explore what the experience of staying in bed in the morning was really like, in a moment-to-moment way. Perhaps it was pleasurable sometimes… perhaps she felt bored… maybe there was anxiety at other moments… I asked her to try and set aside her judgments to really closely examine what she was feeling when she languished in bed for hours. Carol agreed to try the assignment and came to her next appointment and spoke about her experiences with less judgment and significantly more interest. In fact, she had noticed that on some mornings she really enjoyed being able to stay in bed, especially after all the years of working and getting up early each morning. She also noticed that on those days that she had nothing planned to do, she experienced some dread of how she would fill the long day ahead. She also noticed, contrary to her first description of the problem, that on some mornings she did feel like getting up and did so without too much hesitation. Carol’s self-criticism of this behavior did not disappear immediately, however. She continued to berate herself for those mornings that she lingered rather than immediately getting up and starting her day. This then led to a more general assignment for her, which was to begin to notice and take note of her self-criticism, regardless of the content. Once again, the instructions included encouragement to observe these thoughts, almost like an objective scientist watching what her mind produced. She was to notice as often as she could when she was criticizing herself and “note” it without attempting to change the thought in any way. I told her that we would talk about it further in the next session. When Carol came in the following week, she laughingly talked about a constant, steady stream of self-criticism that, while on the one hand she could see with some objectivity, on the other hand felt very real to her. The therapy at this point began to look more closely at her childhood and at long-held beliefs Carol had about why her mother had not appeared to love her. Carol continued to practice noting the self-criticism while I helped her look with “new” eyes (adult eyes) at her mother’s inability to express love and Carol’s striving to get her approval. As Carol was able to remove herself from the cause of her mothers’ behavior (it wasn’t who I was, it was how my mother was), she was also able to dis-identify with the self-criticism. At this point, her depression started to lift and she began to be able to manage her life more easily. With her doctor’s [6] approval, she gradually weaned herself off of the antidepressant she had been taking and after a few shaky weeks felt she was managing as well as she had while taking the medication. Discussion There are many ways of understanding the progress made by these clients in therapy, utilizing mindfulness techniques alone or with psychodynamic psychotherapy. One aspect of the treatment is to help the client develop greater affect tolerance. In anxiety, the highly unpleasant experience of anxiety leads many individuals to try and avoid any situation, external or internal (thinking about the problem) that they feel might lead to anxious feelings. In phobic patients, avoidance as a pattern of coping results in less and less freedom of movement in one’s life. At the same time, since there is no experience of success in coping with the anxious feelings, the fear of becoming anxious starts to motivate much of the individual’s behavior. A spiral of increasing anxiety and decreasing coping often results. The practice of “noting” allows for a dis-identification with the experience of anxiety that creates distance from the experience without denial or conscious suppression of the experience. It is, in a sense, making the “preconscious” conscious. “It is awareness of, rather than thinking about, mental events” (Germer, p. 154). While similar in some ways to cognitive-behavioral therapy for anxiety, an approach using mindfulness meditation techniques differs in that it tends to be more flexible and it is not based on a disease model (Germer, p. 156). This last point needs explanation. In Buddhist psychology, problems are not viewed as examples of individual pathology, but rather as universal problems that all sentient beings experience. We all at times either grasp at or push away thoughts, feelings and perceptions. We all wish to avoid pain and increase pleasure in our lives, yet not one of us is capable of controlling our lives so that unpleasantness doesn’t arise. A technique such as “noting” has application for each of us, no matter whether or not we experience anxiety. It can be helpful to us in situations that demand patience (“watching” our reaction rather than reacting when we are sitting in traffic) or when we are angry at someone else’s behavior, i.e. being aware of, and tolerating, undesirable behavior from a friend, colleague or boss, especially when reacting to that behavior is not in our own best interests. “Noting” is therefore a tool that both therapist and patient can share, rather than a “treatment” for someone with a “symptom”. The attitude of understanding that comes from a shared experience goes a long way towards mitigating the client’s feeling that something is wrong with him or her. As might be anticipated, I have found that in general this approach works best with people struggling with mild to moderate anxiety, although I have recently begun working with a 32 year old man with severe anxiety for many years and he has experienced some immediate moderation in his level of anxiety. In situations of severe anxiety, therapy in conjunction with medication is usually indicated. Recent advances in the application of mindfulness meditation to working with depressed clients have built upon earlier developments of Aaron T. Beck and others on the relationship between thoughts and depression. While it had been observed clinically that depressed clients evidenced negative thoughts, Beck proposed that perhaps negative thoughts were themselves a cause of depression (Segal, et al, p.22). That idea became the rationale for a cognitive approach to depression, in which clients would look directly at their thoughts as a way of confronting their depressed moods. Mindfulness meditation was a natural concomitant to that approach as it also works directly with thoughts, though with a slight variation [7] of emphasis. Mindfulness meditation does not attempt to counter or oppose thoughts, but rather proposes that awareness of thoughts alone is sufficient to change their influence on the (depressed) individual. Carol fit the standard profile of the depressed individual in that she tended to get caught up in negative self-representations which had a strong influence on her mood. In the case of her staying in bed in the morning, while a number of factors came into play, her negative self-judgments about the behavior were largely responsible for generating depression and dissatisfaction about herself. When she began noticing and isolating the self-judgments, she became appreciably less depressed. In psychodynamic terms, we worked to moderate a harsh superego. In terms of Buddhist psychology, Carol began to look less judgmentally at all aspects of her experience, negative and positive, and became more accepting of all sides of her personality. Summary While programs such as Mindfulness-based Stress Reduction (MBSR) are helping introduce meditation to a more general audience (including both mental health professionals and non-professionals), it still remains a largely neglected and often misunderstood approach. For example, a common response of clients to my suggestion that they might want to try meditation is “Oh, I tried that but I can’t do it. I can’t make my mind a blank!” Other general notions that Westerners often have is that Buddhism is depressing (only focusing on suffering) and that it is entirely a spiritual practice, with little to offer western psychology, which is a “science”. In fact, the emphasis (if there is one) on suffering in Buddhism comes about in relation to the belief that it is only through the understanding of the causes of suffering that we can find freedom from suffering. With regard to the question of spirituality versus science, the Buddhist model repeatedly exhorts individuals to not accept any ideas just because someone says they are true, but rather to test them out in life. It is a very practical approach to life and does not require blind faith. Those arguments aside, however, there is a much more serious limitation to a more widespread use of these ideas in general mental health practice. When Zindel Segal et al decided to develop what they called “attentional control training” for the prevention of relapse among depressed clients, they discovered that it was not enough to teach “mindfulness” as a “skills training exercise”. In observing the staff at Umass Medical Center where MBSR was being used, they became aware that it was not simply a set of skills that was needed, but that the therapist working in this way also needed to embody the ability to relate differently to negative affect or the program wouldn’t work. They discovered that: “Participants in the MBSR program learn about mindfulness in two ways: Through their own practice, and when the instructor him- or herself is able to embody it in the way issues are dealt with in class…If the therapists themselves are not mindful as they teach, the extent to which class members can learn mindfulness will be limited…” (56). It has been my experience that this is true of psychotherapy practice as well. Having taught numerous classes to clinicians who are interested in learning to use meditation-based techniques in their practice, it has been demonstrated repeatedly that unless the clinician has a strong practice of his or her own, there is not sufficient conviction or actual experience with the method to be able to help clients learn it. At the same time, however, developing a meditation practice to the degree that one experiences the power of the practice and its potential to alleviate suffering, takes considerable time and commitment. Most therapists [8] are not prepared to make that commitment, so that the information remains an interesting topic but not a usable tool in treatment. It is the purpose of this paper to inform mental health practitioners about the potential efficacy of incorporating mindfulness-based meditation practices into their lives and professional practices. It is my hope that as more clinicians experience the power and usefulness of these practices, they will take the time and make the effort to try the “path” and enjoy the benefits of wherever it leads. [9]