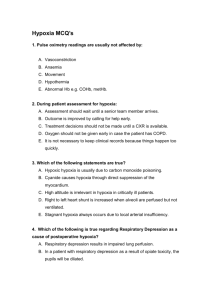
Pulmonary embolus
advertisement

Protocol for the management of pulmonary embolus Department of Internal Medicine, PMHC Pulmonary embolus is caused by a blood clot that passes from the peripheral venous circulation to the pulmonary aterial ciculation causing impaired gas exchange as well as increased pulomnary vascular and airways resistance. Right ventricular dysfunction may result and right sided heart faliure may be the ultimate cause of death in patients with either massive pulmonary embolous or repeated smaller emboli. Diagnosis can be difficult and requires a high index of suspicion as well as careful diagnostic evaluation. The Geneva scoring system presented below can help identify patients where further evaluation should be carried out where the diagnosis is uncertain. Presentation – The most common symptoms are dyspnoea, chest pain, cough and less commonly haemoptysis. Examination maybe normal, or there may be tachycardia and tachypnoea. The legs should be checked for DVT. In massive pulmonary embolus patients may have cyanosis, hypotension and signs of right heart faliure such as a raised JVP. Chronic recurrent pulmonary emboli may present as pulmonary hypertension / heart faliure. Remember to ask about risk factors such as recent immobalisation (such as a recent operation or hospital stay), hormonal contraception, smoking, obesity, cancer, pregnancy, hypertension, COPD and inherited thrombophilia. Pulmonary emboli often occur in hospitalised patients – such as those who are around one week post surgery or in medical patients that are relatively immobile due to their underlying illness such as TB patients. Management 1. 2. 3. 4. 5. 6. In patients presenting with dyspnoea consider pulmonary embolus in the differantial diagnosis – look for associated signs, symptoms and risk factors as outlined above. Try to rule out other diagnoses such as pneumonia, tuberculosis, acute coronary syndrome, pleurisy, rib trauma and pneumothorax. If the patient is unstable (tachycardia, hypotension, cyanosis) get senior advice and help – the patient may need urgent CT angiography / HRCT chest and possible thrombolysis via a central vein. Give oxygen and analgesia, such as morphine. Insert a large cannula, give IV fluids if the patient is hypotensive. In stable patients take a full history and do an examination looking for the signs and symptoms mentioned above. Take a chest x-ray. This will help exclude other diagnoses. It maybe normal in pulmonary embolus or may show a wedge shaped infarct. Record an ECG to exclude a cardiac cause of chest pain. This maybe normal in pulmonary embolus or may show tachycardia, right bundle branch block, right axis deviation, non specific ST changes, right venticular strain shown by T wave inversion in V1 to V4 and rhythm changes such as atrial fibrillation (S1 Q3 T3 is very unusual). If the patient has an oxygen saturation less then 93% do a blood gas to assess the degree of hypoxia. Take blood for a clotting profile, full blood count and renal function. If pulmonary embolus is felt to be the diagnosis start heparin either unfractionated heparin or low molecular weight heparin. Unfractionated heparin should be initiated as a 5000iu bolus dose then given by continous infusion at the rate of 18iu/kg per hour. The rate should be adjusted to achieve an APTT of over twice normal. At Ngwelezane we have enoxaparin (Clexane) which is not licensed for use in pulmonary embolus but has been used at the dose of 1mg/kg 12 hourly for treatment. Futher diagnostic evaluation should include CT angiography (high resolution CT chest is an alternative especially if there is a contraindication to intravenous contrast such as renal impairment) – if this is unhelpful carryout doppler ultrasound on the legs if a DVT is present consider pulmonary embolus likely and treat as such – if there is no DVT – consider sending the patient for a pulmonary angiogram or V/Q scan in Durban. If the diagnosis of pulmonary embolus is confirmed start warfarin aim for an INR or 2.0 to 3.0. Try to establish the underlying cause of the pulmonary embolus. If the cause or risk factor has gone stop warfarin after 6 months. If the cause continues to be present take expert advise before stopping warfarin. Geneva Clinical prediction rule points Age > 65 Previous PE or DVT Surgery or fracture within 1 month Active malignancy Unilateral leg pain Haemoptysis Heart rate 75-94 Heart rate >= 95 Pain on leg palpation and unilateral oedema 1 3 2 2 3 2 3 5 4 Clinical probabilty Low Intermediate High 0-3 4-11 >=11