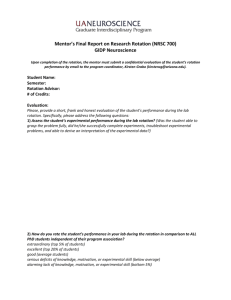
UOMHS Department of Psychiatry/Behavioral Medicine Rotation
advertisement

PsyRotOrientation Rev 6-12-10 David E. Drake, D.O., FACN, DFAPA Clinical Professor of Psychiatry Des Moines University Private Practice, Des Moines Family Psychiatry 1221 Center Street Suite 3 Des Moines, IA 50319-1014 515.288-8000 ddrakedo1@qwestoffice.net Medical Student Psychiatry Rotation “Systems therapy cannot remake what nature has created, but through learning how the organism operates, controlling anxiety, and learning to better adapt to the fortunes and misfortunes of life, it can give nature a better chance” “(Man) does have one ability beyond other protoplasmic life, and that is his ability to observe, think abstract, and see the natural order, to understand the secrets of nature and to govern himself a bit differently. …Even the most objective of all thinking is done with brain cells that are protoplasmic outgrowths of all protoplasm. It is impossible for man to ever become completely objective and the future of the brain will ultimately be determined by the natural order.” Murray Bowen, M.D. If you are considering a psychiatry rotation with me, please read the following to get an idea of what these four weeks will entail. If you have already signed up to spend time with me either in a shadowing capacity or for the full rotation, welcome to this practice! Some pearls and what I want you to focus on during this rotation or shadowing: When a person presents with symptoms (and we all have symptoms!), I’d like you to be thinking about “What has you stirred? What are you reacting to? Where are you stuck? Where are you trying to get to? And what’s getting in your way?” These are also questions I would like you to be asking the folks in my practice who you will be meeting with – either with me or by yourself in the Education Room of my office. I want to encourage you to allow folks to tell their story – what they have been through and what has helped them along the way. ***Note: this rotation is demanding, challenging, and gratifying. I expect much and will treat you well in return. This rotation requires a good deal of emotional maturity and stability. As a solo practitioner in private practice, my time also focuses on building and maintaining a practice – marketing/PR – and students will be involved in that activity as well. How to find my office (depending on highway construction!) : from I-235 going east (the exit on I-235 is closed at this time and you’ll have to make your way around off of the highway – call for directions if you need them), take Keo South to 12th Street, Go right on 12th Street to the yield sign to the right onto Center Street. Go to the driveway on the west side of the first building on your right. Enter the driveway and go to end of first building to Suite 3 of 1221 Center Street. It says my David E. Drake, D.O. on the door. From Ingersoll, go north on 15th Street past Methodist Hospital on your right – passing Pleasant Street, the Ronald McDonald House, to Center Street. Take a right (east) on Center Street. You will pass the Oakridge housing complex on your left and then the Eyerly-Ball Mental Health Center. The next building on your left is my building complex. Follow the directions above to Suite 3. _____________________________________________________________________ **Note: the office is “Japanese-style” – we leave our shoes just inside the door and go without our shoes – I wear clean crocks just for the office that I leave here – please bring slippers or Crocs or something similar that are not worn outdoors. _____________________________________________________________________ This is a rotation with an emphasis on understanding the family as a system. And while I use medications, the primary focus is on psychotherapy. You will be exposed primarily to Bowen Family Systems Theory as devised by Murray Bowen, M.D., who was a psychiatrist and Director of the Bowen Family Center in Washington, D.C. Bowen Theory is based on the individual as part of a family system and emphasizes evolution as central to understanding life in our world and our part in nature. You can access the website for the Bowen Center for the Family to learn more at: www.thebowencenter.org Much of the focus of this rotation will be on you and your own family life. You will watch videos, write about yourself and your family, read articles and book chapters, see patients from my practice – sometimes while sitting in on psychotherapy sessions in my office, sometimes seeing patients by yourself in the Education Room in this office, and when we have inpatient admissions or consultations in the hospital. When you sit in on sessions in my office, I ask students to blend in with the woodwork – to not make sounds or react to what the patients are saying. I will generally not introduce the patients to you, but if they talk to you during the session, feel free to respond back. After you get the hang of it, I will generally ask you to ask a question of the patient at the end of the session. Please take notes while you are listening. Many students find the rotation emotionally intense and draining. You will listen to stories of incest, rape, domestic violence, drug use, prison terms, mental illness, chronic physical illness, marital conflict, divorce, etc. Please let me know if you have any special needs that might hinder your ability to talk with people about these topics. Note: This is a talking rotation – if you are shy or quiet, this could be a struggle for you, not that you shouldn’t do it or can’t do it. When I give you articles or books to read, DVD’s or videos to view, opportunities to meet with patients in the office, hospital, and nursing home setting, I will expect you to approach me with your feedback and comments. Silence comes across as disinterest and/or a lack of engagement in the rotation. **Please refer to the Student Orientation folder that will be given to you by Dr. Drake on your first day. During some months, I will have two students on rotation. I request that one student remain in the office when I have two students with me, while the other is on out-rotations with this practice. ----------------------------------------------------------------------------------- You are about to begin a rotation with me in my role as a general (family) psychiatrist in a solo private practice. Students are not to have part-time work in addition to this rotation. This rotation will require your full attention and time. The rotation ends at the end of the day of your last Friday. Numbers you will need: our office: 288-8000 My home: 279-0670 My cell phone: 229-5085. My e-mail at work: ddrakedo1@qwestoffice.net **Needed Equipment: 1) cell phone or pager 2) Bring your laptop computer to the office for writing assignments and for accessing the Internet. The office is hooked up for wireless connection. (look through the student folder on the student desk for instructions on how to access the wireless computer network in my office). Jan Burns is the part-time office assistant who generally works from 8 a.m. to 1 p.m. Monday through Thursday. She is, now semi-retired, having previously worked as office manager for an 8 physician clinic with Iowa Health Systems, and later doing the same with a group of nurse midwives. The rotation is generally family friendly. If you have special needs regarding care for your children or your marriage/partnership, let me know. Also let me know if you have special times that you set aside for meeting religious obligations, services, activities, meetings, etc. My expectation is that a student’s time will be flexible as the schedule can change throughout the day – e.g. late patient hours I will give you assignments with regard to reading material and videos. Please assume that your written notes about patients will be read by the patient themselves – probably a good thing to keep in mind on other rotations and in your future practice as patients do have a legal right to review their charts and to have copies of their notes. I will often read your own notes that you wrote to the patient at the next session. Here is a partial list of my expectations of you for your days on this rotation. On the first day or your rotation Receive and review a copy of the initial consultation/interview protocol by Dr. Drake for seeing patients in the office. Make sure you make a copy to keep at home or in your car in case you are called at home to see a patient in a nursing care center. I start in the office at 7:15 a.m. or 8 a.m Monday through Friday and am usually finished in the office by 6 p.m. Infrequently, I may have a later appointment and may need to have you stay for that as well. If you have meetings or appointments you need to attend, let me know and we’ll see what we can work out together. Always keep my office informed of your whereabouts if you are going to be delayed. .Keep confidentiality at all times. When you discuss what you hear and see with friends and family, as well as with other students, be sure to disguise the particulars so as not to identify that person. This is, obviously, especially important in psychiatry. *** Don’t make phone calls to third parties or release information to someone who is calling you or this office without the written permission of the patient to do so, and unless I have directed you to do so. Students are not to socialize with or date patients from this practice. Should you know someone in my practice on a social basis, prior to this rotation, let me know and I will not have you sit in their sessions or be involved in their care. Students are not to enter into any business transactions with patients from this practice, including the buying or selling of any goods. Students are not to socialize with any patients or their family members/significant others from this practice. If you have any questions or concerns about questions of ethics, including boundaries with patients, please let me know and we’ll discuss it. Unlike other rotations and practices, it is highly private even that someone sees a psychiatrist. Should you run into folks from my practice in public or social settings, please do not approach the other person but let them approach you if they want to say hello and keep it private from others how you met this person. The below ‘mini’ rotations are part of a ‘cafeteria’ assortment of options. You will do a few of them but certainly not all. Don’t fret at all about them during the first week. I will talk to you about which ones to call and set up after the first week. I try to make the rotation especially pertinent to your particular interests and specialty or primary care career path. **(Please note where one student at a time is designated or two, during months where I have two students with me on this rotation). For the most part when two students are on the rotation, one student will remain in the office to work with me and so they will take turns with the out rotations. When I have only one student, the primary focus will be on the office. Week One: 1. Write a 8-10 page autobiography (typed and double-spaced) about you and your family – from birth to how you got where you are now – include information about your relationships with your parents, your siblings, your friends, significant others, etc. If you have been in any form of counseling or psychotherapy now or in the past, include what this experience was like for you – did you then or now see it as a positive or negative experience? Include your religious/spiritual and political beliefs/persuasion and how you came to these. Write about how you came to enter the medical profession. Please have this completed by Tuesday, the second morning of the first week. I will give you most of your first day after noon to write this. I will have you read your autobiography out loud to me so I can comment and ask questions. This autobiography will be held in confidence. I will review the basics of breath-focused meditation your first day. This is from Tricycle's Daily Dharma: February 26, 2007 Completely Missing the Moment ”It is often the case that whatever we are doing, be it sitting, walking, standing, or lying, the mind is frequently disengaged from the immediate reality and is instead absorbed in compulsive conceptualization about the future or past. While we are walking, we think about arriving, and when we arrive, we think about leaving. When we are eating, we think about the dishes and as we do the dishes, we think about watching television. This is a weird way to run a mind. We are not connected with the present situation, but we are always thinking about something else. Too often we are consumed with anxiety and cravings, regrets about the past and anticipation for the future, completely missing the crisp simplicity of the moment.” --B. Alan Wallace, Tibetan Buddhism from the Ground Up Optional (after getting an introduction to breath-focused meditation from me your first day): Attend a Mindfulness Meditation Group (2 students ok) – on Tuesdays from 7:30 p.m. till 9 p.m. at the Friends Meeting House at 4211 Grand Avenue in Des Moines. The group is led by Charlie Day, PhD and/or Paul Lambakis, MSW. You can attend the first sitting (40 minutes) at 7:30 p.m. where instruction for beginners is given and then stay for the 20 minute talk and you can stay for the 2nd sitting (30 minutes) which is from 8:30 till 9 p.m. 2. (Optional – but I hope you take advantage of this! – You are given the time off to pursue this – but at your own expense. Please clarify the cost with the massage therapist prior to going to your appointment and let them know you will be paying them at the time of the appointment. Experience an educational massage with one of three local massage. The three and their contact information include: Diane Goodson at 277.0790 (cell phone is 988.9978) and at diart@gronkulator.com on 4730 Ingersoll (just ½ block west of Polk Blvd in Des Moines); Michael Thompson at 284.5777 or 975.7931 in Sherman Hill (just a few blocks from this office) at 1700 ½ Woodlawn Avenue, and Melissa Van Kooten at 4400 E. university Avenue in Pleasant Hill at 229-8423. If you are more relaxed yourself you are of greater benefit to your patients and this is to inform you about resources available to you and your patients for stress management. The therapist will give you a full massage and will also talk with you about the emotional and physical benefits of massage. When you call for the appt remind them that you are seeing them for an educational massage. 3. Read about ethics in psychiatry from the American Psychiatric Association’s website at: http://www.psych.org/MainMenu/PsychiatricPractice/Ethics/ResourcesStandards/Prin ciplesofMedicalEthics.aspx Pay special attention to boundary issues in psychiatry and medical practice in general. Week Two: Due the second Monday is a family diagram of your family – going back to your grandparents on both sides – include dates and causes of deaths, who’s in jail, on drugs, drinks too much, divorces, professions/jobs/unemployed, ages, etc. The student folder gives descriptions of how to make this. Do this in pencil so changes can be made. Tanner Nissly, 3rd year DMU D.O. student with me in June, 2006 found this website and I pass it on to you as possible assistance in the making of your family diagram. It does a very neat job of it. Tanner wrote: http://www.genopro.com/ “This is the website from which you can get the program to aid in making a genogram. Getting the program is relatively self-explanatory from the website. It is a shareware program...and you have a 30 day free trial. You have to give the site an email address for activation of the program. As far as using the program, I found it very helpful in organizing my family tree. They have several tutorials and help sessions on the program to aid you in getting started. The only thing that I really had trouble with right from the start, was finding out how to change a marriage to divorce. To do this simply double click on the marriage line. From there a pop-up menu entitled "Family Properties." Under the "relations" pull down menu, you can have several options to define the relationships between two people.” At the end of Week Two (Friday): write several paragraphs on how you see your performance so far on this rotation. Where do you need improvement and what do you plan to do about it? Regarding Lifestyle changes: please familiarize yourself with all the current methods of smoking cessation available – lozenges, gum, Zyban (Wellbutrin is another trade name – buproprion is the generic), Nicotrol Inhalers, Chantix. Be prepared to talk with patients in my practice about what they can do to stop smoking. Also be prepared to talk with folks in my practice about weight loss, nutrition, and exercise. I will assist you in setting some ‘field trip’ mini-rotations. The main focus, however, will be time spent in my office. one 1. I want you to attend meeting each of A.A. (Alcoholics Anonymous), N.A. (Narcotics Anonymous), and Al-Anon during this month. (2 students ok) You can call each these groups to find out where and when an open meeting is available (‘open’ means available for non-members to attend) Call AA at 282-8550; NA at 244-2277; and Al-anon at 277-5059. Please make a notation of where and when you attended each meeting for your record. You can attend these meetings over the lunch hour, in the evenings, or on the weekends. When you meet people at the meetings, you can tell them you are a medical/P.A. student who was assigned to attend the meeting to learn more about alcoholism/drug abuse. These meetings have been most welcome to our students. 2. You will also call a local business man and experienced A.A. member, Mr. Jim Baker (2 students ok) at one of the following numbers: office: 327.8731 cell: 556.1936 home: 277.0790 Mr. Baker and you can set up a time to meet him over coffee to discuss his own experience with this valuable organization. He will have much to teach you. 3. Contact Ms. Sarah Evans, BA, CADC, Substance Abuse Counselor, of Mecca Substance Abuse Services, at 262.0349, to spend 1-2 days with her staff at 3451 Easton Blvd is the outpatient program and the residential program is at 3806 Easton blvd in Des Moines (50317). Mecca has both outpatient and inpatient facilities. 4. Contact Passageway at 243.6929 (305 15th Street in Des Moines) to take a tour of this club house for mental health consumers. The director is Ms. Linda Oleson-King. 4. Spend part or all of one day with the Churches United Shelter at 205 15th Street. Contact whoever is the current director and let them know that we use to do this with Ms. Jean Brown – call 284.5719 to set this up. This facility provides shelter, food, and other resources for homeless folks. Mental illness is common among many of the folks who stay there. 5. Contact the office of Steven Zorn, M.D., to spend one-half day with him or Steve Grant, MD (Dr. Grant is an internist and psychiatrist) at the Iowa Sleep Disorders Center at 4080 Westtown Parkway in West Des Moines. (The half-day is because he does internal medicine with the other half.)Tell him you want to be present for the time of day when he evaluates folks for possible sleep disorders. His office number is 225.0188. 6. Contact Ms. Christina Smith with Community Support Advocates (CSA) at 883.1776 x 264 to arrange 1-2 days to spend time with their case managers and other staff. You will attend staff briefings and go with case managers to clients’ homes to meet with them in their own element. 7. Contact Jacqueline Stoken, D.O., at 327.0046. regarding the possibility of spending one day in her physiatry (rehab medicine) practice. She sometimes has a student with her already, in which case it will not be possible. Dr. Stoken is an osteopathic physician who incorporates principles of holistic medicine into her practice. This will also be a good review of OMT for D.O. students on the rotation and a good introduction to physiatry or rehab medicine for both D.O. and P.A. students. Her practice is located at 1454 30th St. Suite 109, in West Des Moines. Or contact Ed Steinman, DC, DO – to spend a day with him on a day when he is scheduled to do a lot of OMT – his office is just below mine on the other side of the building at 1221 Center Street, Suite 15 – at 243.2888. 8. For students who would like to learn more about psychoanalysis and psychoanalytic psychotherapy: Meet with Ms. Deana Schuplin, a local psychotherapist in private practice who is training in psychoanalysis at the training institute in Kansas City (see the video on the life of Freud prior to this meeting). The two of you can arrange where to meet – this office or?? You can reach her at 515.418.7735 or Deana@Schuplin.org – 2 students 11. For those students interested in chronic pain – contact Dan Baldi, D.O. who practices anesthesiology at Broadlawn’s Medical Center with United Anesthesia and Pain Control. His practice refers me a number of folks with chronic pain for psychotherapy and stress management training. He has a student with him from my practice on a Wednesday or Thursday. The main office number is 282.5710. His cell phone is 229.6128 13. Spend one half day with the Family Violence Center. Contact Ms. Marlene Wozniczka at 471.8699 x 114 to set up time to do so. Two students are ok at one time. In addition to a half day at the Center, contact Ms. Amra Viso, the Outreach Advocate at the Domestic Violence Shelter at 471.8699 ext. 116, to attend an open support group 14. Spend 1 or 2 days with Wes Richardson, DO, psychiatrist with the PACT (Program on Assertive Community Treatment) or Ara Robinson, D.O. – seeing patients in their office and in the homes of patients. Please call PACT at 282.9972 and set up times with Molly Mertens (married to class of 2010- DO, Ryan Mertens) to spend time with Drs. Richardson or Robinson or with Molly on her rounds with folks in the program. The PACT office is at 401 E. Court Avenue, next to AJ’s in the back of the building. . 15. Spend 1 or 2 days at the Vet Center – contact Ms. Katina Mach, director at 284.4929 to set up a time to go there. Vets returning for current or past wars are counseled there. The Vet Center is located at: 2600 Martin Luther King Parkway in Des Moines. Week 4: Due the Wednesday of your last week: is an 8-10 page original personal paper (typed and double-spaced) – I would like you to reflect on what you have learned over the past month on this rotation – about yourself, your personal relationships, your family, and our human species. I will have you read this paper to me also so I can comment and ask questions. Do not give me a review of Bowen Theory unless you plan to relate aspects of it to you and your family and other relationships. End your paper with a narrative evaluation of your performance over this last four weeks – the positives, where you excelled, as well as your weaknesses and where you need further development. __________________________________________________________ _ Required Readings: (all available in this office) Articles: “Chronic Anxiety and Defining A Self” by Michael Kerr, M.D. – both should be in your packet. Pamphlet: “One Family’s Story: A Primer on Bowen Theory by Michael E. Kerr, M.D. – find in the office or on-line at www.thebowencenter.org – this website has other material on Bowen Family Systems Theory as well. Books: Extraordinary Relationships and Connecting with our Children: Guiding Principles for Parents in a Troubled World by Roberta Gilbert, M.D. Peruse and see what is useful to you from the more extensive, in-depth, Family Evaluation: The role of the family as an emotional unit that governs individual behavior and development by Michael Kerr, M.D. We have numerous resource books – psychiatry texts, etc., available in the office. For you history buffs in psychiatry – watch this video American Experience | The Lobotomist | PBS http://www.pbs.org/wgbh/amex/lobotomist/program/ A video to watch: re the controversy of the diagnosis of bipolar disorder and the use of psychiatric medications in children: a provocative and important film Check out http://www.pbs.org/wgbh/pages/frontline/medicatedchild/ An important film on prisons as the ‘new asylums’: http://www.pbs.org/wgbh/pages/frontline/shows/asylums/view/ A video on health care around the world: see what you think of the different systems of care now in operation around the world. http://www.pbs.org/wgbh/pages/frontline/sickaroundtheworld/ I encourage you to watch this video – Doctors Diaries – on the experience of becoming a physician: 2hrs total: http://www.pbs.org/wgbh/nova/doctors/program.html Some Admonitions: a. Do not remove any video/audio tapes, books/magazines/journals from the office without permission from Dr. Drake. b. No need to wear white coats. Please do wear your ID badge for consultations and admissions, but not needed in this office. c.Never suggest or recommend changes in a patient’s treatment without first getting your idea approved by Dr. Drake. Do not give advice about how the person should live their lives regarding their relationships. Do share information regarding healthy lifestyles – smoking, drinking, diet, exercise, stress management, etc. Do not see patients in the office without Dr. Drake being present in the building, unless he gives you permission to do . ***If you ever have doubts about what you are doing or are concerned for your own safety or the safety of others, contact me at once. e. please do not hang out in the office assistant’s area unless you are directed to do so. My office assistants have much work to do. You can study in the chart room where you have a desk or the Education Room. You are certain to find this rotation challenging and you will learn a great deal - about yourself and about the struggles of our fellow human beings. I will give you feedback throughout this rotation, so that the final evaluation is not a surprise. I look forward to hearing your feedback as to how we can improve this learning experience for you. Let me know, along the way, of any problems you might be experiencing. My goal is to make this time personally as well as professionally rewarding. I am glad to have you with this office for the next month. Don’t be afraid to ask for an hour or so off from seeing/observing patients in my office. Most students find the work intense and even overwhelming at times. Your evaluation for the rotation: is dependent on a number of factors: your participation – asking a question of the patient at the end of most sessions in my office; your questions to me; the quality of your personal paper and family diagram, reports back from other sites where you spend time while on this rotation; your professional demeanor; your willingness to learn; attitude and enthusiasm; as well as the other factors outlined in the rotation evaluation sheet. **Preparation for the D.O./M.D. Boards – Our D.O. students do well on the psychiatry section of the Boards. My advice to you is to re-read your psychiatry notes – especially with regard to medications and DSM-IV diagnoses. **Preparation for the DMU Dept. of Psychiatry end of rotation exam: review your class notes. You can also watch pertinent videos in this office. In the past the exam was heavy on DSM-IV diagnoses and psychiatric medications. This exam is administered by the Dept. of Psychiatry at a place and time to be determined by the respective parties. I would recommend taking it during your last week. I am aware that you have other required texts to read. Whenever you have questions, concerns, problems relating to this rotation, let me know. I want this to be a valuable rotation for you – personally and professionally. **If you have an especially good experience, please write a thank you note at the end of your rotation to each person you spend time with while on this rotation. Running a small office: Each of us, my office assistants and I, and each student with me, help out with the daily ‘chores’ of keeping things going. I will sometimes ask you to assist with minor administrative tasks. Students are asked to keep their office area (which is combined with the chart room and the Education Room) neat and clean. Psychiatric Medications and Other Somatic Treatments to Learn for this Rotation but first….. My note to pharm reps from April 2005: Dear pharmaceutical representative – I have appreciated the information, samples, and service that you have provided this practice. However, due to wanting to preserve the privacy of the individuals, couples, and families in my psychotherapy practice, I am asking that pharm reps no longer come into the office. I am glad to accept information and invitations to speakers via e-mail (ddrakedo1@qwest.net), regular mail (1221 Center Street Suite 3, DSM 50309), voice mail (288.8000), or by fax: 288.4073. I am no longer accepting sample medications. Should your company come out with a new product, I am glad to receive literature via the means above and I will contact you should I wish to meet with you in person. Please contact me at any of the above means should you have any questions about this. Thanks. Sincerely, David E. Drake, D.O. Family Psychiatry I. Placebo Effect A. Part of every health care provider/patient interaction B. The ceremony II. Review of Medications: A. anti-manic meds: B. Antipsychotic (neuroleptic) meds: 1) Extrapyramidal Symptoms (EPS) Akathisia (inner restlessness) Oculogyric Crisis (eyes rolling up) Dystonia (muscle Contracture) 2) Tardive Dyskinesia (T.D.) a) giving informed consent – important in all branches of medical practice 3) Neuroleptic Malignant Syndrome (NMS) : according to Kaplan and Sadock in their psychiatry text, this is a “life-threatening complication of antipsychotic treatment and can occur anytime during the course of treatment. The symptoms include muscular rigidity and dystonia”, among other symptoms. “The autonomic symptoms include high fever, sweating, and increased blood pressure and heart rate.” C. Anti-Parkinson Meds: for potential/actual side effects from neuroleptic meds. D. Anxiolytics (for anxiety) E. Antidepressants 1) Light Therapy and Seasonal Affective Disorder (S.A.D.) 2) Review of the antidepressants 3) Vagus Nerve Stimulation (VNS) 4)ECT (electroconvulsive therapy) – sometimes called electroshock therapy. F. Hypnotics (for sleep) – most desirable if quick and short acting so as not to cause ‘hangover’ in the a.m. Psychiatric Medications to Learn for this Rotation Please have familiarity with the following classes of medications and the individual medications. I would like you to know the common indications and side effects, where specified, for each class listed. **Please understand that this listing is based on how the medications are marketed - that the actual uses are based on pharmacological effects. For example, Benadryl (diphenhydramine) is used for sleep, sometimes for anxiety, akathisia, and other possible side effects from a neuroleptic such as dystonia and oculogyric crisis, and for allergies/anaphylactic reactions. The SSRI's have a long list of possible uses. Valium (diazepam) is used for anxiety, sleep, muscle relaxation, and seizure control. I have listed the trade names first and generic names in parentheses, where I think it's important to know both. Your certification exam will probably use generic names, but in clinical practice you will ‘talk’ the trade names and read journals that use the generics. So, as you can see it’s important to know both. The PDR (Physician's Desk Reference) and your psychiatry reference book are both good sources of information. ***Get some practice in looking up a medication by its trade name in the pink section of the PDR. You will learn about its generic name, its mechanism of action, potential benefits/uses, side effects, routes of administration, and dosages. **Be sure to use the PDR on your own to look up at least one of the medications listed below – just to begin getting used to turning its pages as it will be an essential part of your reference library in the hospitals and in office settings while on rotation. Antidepressants: MAOI's (Monoamine Oxidase Inhibitors): Nardil (phenelzine) TCA’s: (Tricyclic Antidepressants: Elavil (amitriptyline), Pamelor (nortriptyline), Tofranil (imipramine) SSRI's: (Selective Serotonin Reuptake Inhibitors): Prozac (fluoxetine), Zoloft (sertraline), Paxil (paroxetine), Celexa (citalopram), Lexapro So-called 'SNRI's: (Serotonin Norepinephrine Reuptake Inhibitors): Effexor, Cymbalta. Cymbalta is increasingly used for persons with depression and chronic pain. Other classes: Wellbutrin (buproprion - an aminoketone); ***Zyban (is also buproprion and is Rx’d (prescribed) for smoking cessation); Desyrel (trazodone – a heterocyclic compound); Remeron – is a tetracyclic compound; St. John's Wort (hypericum perforatum) - an herbal remedy available in U.S. OTC (over the counter). It is available only by Rx (prescription) in Germany. Remeron can be a good choice for someone who is depressed, not sleeping well, and has been losing weight as it increases appetite, helps with sleep and depression. Obviously it would not be a good choice for someone who is already overweight. Anxiolytics: Benzodiazepines: Xanax (alprazolam), Ativan (lorazepam), Valium (diazepam), Klonopin (clonazepam); Librium (chlordiazepoxide). ***Note: Ativan can be given I.M. (intramuscular) or p.o. (by mouth) and is quick acting. Non-benzodiazepine anxiolytics: Buspar; Vistaril/Atarax (hydroxyzine). (Note: Atarax is commonly Rx’d by PCP’s and dermatologists for itching). ***Hydroxyzine can also potentiate a narcotic like Demerol for pain relief (e.g., following surgery) so that less of the narcotic can be used. Hypnotics: Benzodiazepine Hypnotics: Restoril (temazepam), Dalmane (flurazepam); Non-Benzodiazepine Hypnotics: Ambien (zolpidem)- and Ambien CR (controlled release); Sonata (zaleplon); Lunesta (eszopicione) – all the above three act through their interactions with a GABA-BZ receptor complex, and Rozerem (ramelteon)- a Melatonin receptor agonist. Antipsychotics (aka neuroleptic: literally 'to seize the neuron'): Typical High Potency: Prolixin (fluphenazine), Haldol (haloperidol), Navane. Note: Prolixin and Haldol come in short acting or long acting (decanoate) injectable (I.M.) concentrations. They can also be given p.o.. Typical Low Potency: Mellaril (thioridazine), Thorazine (chlorpromazine) Atypical: Clozaril (clozapine); Risperdal (risperidone); Zyprexa (olanzapine); Seroquel, Geodon, Abilify. Antiparkinson Agents: (used to treat/prevent EPS – extrapyramidal symptoms): Cogentin (benztropine); Benadryl (diphenhydramine) Note: Cogentin can cause pronounced dry mouth and is often given before general surgery as it dries up secretions that could accumulate in the lungs. Antimanic Agents: Eskalith (lithium carbonate); Klonopin (clonazepam); Depakote (valproic acid); Tegretol (carbamazepine). ***Note: Depakote,Tegretol,and Klonopin are also used for seizures. Neurontin (gabapentin),Lamicatal (lamotrigine), and Topamax (topiramate) are anticonvulsants with use for manic symptoms. Psychostimulants: commonly used for ADD/ADHD and sometimes as an adjunctive medication for depression. Ritalin/Metadate (methylphenidate); Dexedrine/Adderall (dextroamphetamine) Concerta is a long acting methylphenidate compound. Cylert (Pemoline) is a central nervous system stimulant that is structurally dissimilar to amphetamine compounds. Psychiatry Post Rotation Exam: I would get going on the exam preparation early on in the rotation. Students find it a challenging exam. (Note from DMU Dept of Behavioral Medicine on 2-15-08) Department of Behavioral Medicine All students are REQUIRED to take the post rotational psychiatry examination. To successfully complete the rotation students are required to receive a passing grade on the exam. Please make certain that students bring no materials to the examination – i.e., books, notes, graphs, study-guides. Palm computers are also not allowed. Printing of the exam is prohibited – please make certain the student does not have access to a printer or is in a supervised setting. My Note: Please call Debbie Bustad at the Behavorial Medicine Dept at DMU to set up the time to take the exam at DMU on either the Thursday or Friday of your last week. I will give you the morning off on your exam day for final exam preparation. When I have two students, one of you will take the exam on Thursday and one on Friday so one of you will be in the office at a time. Some sobering statistics from the DMU Faculty Development Newsletter, February 16ith, 2009: The Tolls of Med School Medical students are more likely to suffer from depression than the general population is, and black students in medical school are particularly prone to frequent suicidal thoughts, according to a new study published in Academic Medicine. Billed as the first large-scale study of its kind, the study examined surveys from more than 2,000 medical students and found some chilling results. The overall depression rate for medical students is 21.2%, more than double the commonly reported rate of about 10% for the general population. The article, “Depressive Symptoms in Medical Students and Residents: A Multischool Study,” drew upon surveys distributed to medical students and residents at six sites in 2003-4. The authors picked sites with higher than average minority populations, aiming for a sample that would reflect the growing numbers of women and members of minority groups in medical school student bodies. In addition to studying depression rates, the study examined the prevalence of suicidal thoughts among medical students and residents. Of the total sample, 5.7% reported having frequent suicidal thoughts. That figure is relatively consistent with the rate of suicidal thoughts in the general population, as reported in the National Comorbidity Study. Suicidal thoughts were particularly prevalent among black students, 13% of whom reported “suicidal ideation.” Indigenous students, including American Indians, Pacific Islanders and Alaskan Natives, had an even higher rate - 16.1%. The response rate for that cohort, however, was just 31 students - half the size of the black student sample. Deborah Goebert, the lead author of the article, said there are a number of factors inherent in the medical school experience that may contribute to the higher rates of depression the surveys detected. “Certainly it’s a stressful time,” said Goebert, associate director of psychiatry research at the University of Hawaii’s John A. Burns School of Medicine. “There’s a lot of learning and responsibility not just for yourself, but then you’re also caring for others. “A lot [of the stress], I think, is related to sleep cycles and expectations,” she added. “And the other thing is that the field is changing so rapidly, even while they’re there. I think that’s also an overwhelming aspect.” Charles Reynolds, senior associate dean of the University of Pittsburgh School of Medicine, said the study is yet another indication that medical schools need to step up efforts to provide mental health resources to students. Reynolds co-wrote a commentary in the February issue of Academic Medicine, referring to the new study as a “clarion call to action on the part of leadership in the nations’ schools of medicine and academic health centers.” “The time is right for strong leadership to change the culture of medicine,” Reynolds wrote, with co-author Dr. Paula Clayton, medical director of the American Foundation for Suicide Prevention. The “culture” in medical schools is in many ways analogous to that of the military, another institution that has struggled to erase the stigma of seeking mental health care, Reynolds said in an interview Wednesday. “We’re supposed to be strong, and to admit we may have a medical illness like depression just doesn’t come easily to us,” Reynolds said. Future doctors may also have reservations about reporting symptoms of depression, fearing it might affect their careers. Most state medical boards, however, no longer specifically ask about mental health issues or substance abuse, Reynolds said. Instead, physicians are asked whether they have any condition that will permit them from functioning on the job. As such, it’s less likely that self-reporting mental health problems will impact a doctor’s career, Reynolds said. “I wouldn’t say that it’s not a realistic concern at all,” he said. “My sense is that it’s less of a concern now than it used to be.” The data collected for the article in Academic Medicine, which is the journal of the Association of American Medical Schools, may also give new evidence about the most risk-prone years in the medical student experience. For medical students, the highest rates of depression - nearly 25% - occurred in the second year of study. For residents, the third year proved the most perilous, with 14.6% reporting depression. Over all, medical students reported rates of depression nearly twice as high as those of residents. Of the sample, nearly 22% of medical students exhibited signs of depression, compared with about 12% of residents. There were also significant differences in responses based on gender. Women had a 21.6% depression rate, compared with a 15.6% rate for men. To determine depression levels, the authors asked students to respond to surveys that included content from the Center for Epidemiologic Studies-Depression scale, a widely used self-reporting instrument to measure symptoms. The Primary Care Evaluation of Mental Disorders was also employed. –Inside Higher Education