Women - Dr John La Puma
advertisement

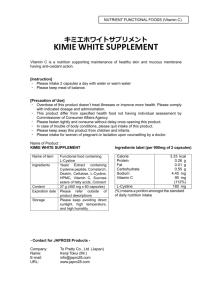
Women Three capsules contain: Vitamin E (as d-alpha tocopherol) 150 mg • Vitamin B6 (as pyridoxine hydrochloride) 6 mg • Vitamin B12 (as cyanocobalamin) 12 mcg • Folate (as folic acid) 400 mcg • Iron (as gluconate) 18 mg • Magnesium (as oxide) 400 mg • Zinc (as gluconate) • Selenium (as sodium selenate) 70 mcg • Proprietary Blend 1080 mg: Chasteberry (Vitex agnus castus standardized to .5% agnusides), Green Tea (Camellia sinensis standardized to 50% phenols), L-arginine. nfertility. There is some preliminary clinical evidence that taking chasteberry orally can increase the chance of getting pregnant in women who are infertile due to relative progesterone deficiency. However, chasteberry does not seem to work quickly. It can take from 3-7 months of treatment to achieve pregnancy (6500,7012,7077). Infertility. Some research suggests that daily consumption of folic acid 5 mg plus zinc sulfate 66 mg can increase sperm count in subfertile men. Further study is required to determine the effect of this combination on infertility (9334). Sem Hop. 1982 Jan 28;58(4):209-12. Related Articles, Links [Infertility and carbohydrate metabolism. A study of 93 cases (author's transl)] [Article in French] Pinget M, Dufour P, Gandar R, Jacques C, Bihr X, Goetzmann P, Dorner M. An oral glucose tolerance test was performed in 93 women with unexplained infertility (sterility or repeated abortions). An abnormal carbohydrate metabolism was found in 1/3 of the cases (32 patients). Advice on diet control, provided to all of these patients, was followed only by 13.9 of these, who conceived less than 6 months after initiation of the low carbohydrate diet, achieved full-term pregnancy. These results suggest a relationship between infertility and glucose intolerance. A glucose tolerance test should be performed in all women presenting unexplained infertility. Epidemiology. 2003 Jul;14(4):429-36. Related Articles, Links Risk factors for female infertility in an agricultural region. Greenlee AR, Arbuckle TE, Chyou PH. Marshfield Clinic Research Foundation, Marshfield, WI 54449, USA. greenlee.anne@mmrf.mfldclin.edu BACKGROUND: Recent studies have suggested that agricultural occupations or exposure to pesticides may impair female fertility. METHODS: The Fertility Risk Factor Study retrospectively examined agricultural and residential exposures and the risk of female infertility. Cases and controls (N = 322 each) came from women who sought treatment at a large group medical clinic in Wisconsin. Women and their male partners provided information on health, occupational and lifestyle exposures in response to a telephone interview during 1997-2001. RESULTS: Mixing and applying herbicides 2 years before attempting conception was more common among infertile women (odds ratio [OR] = 27; 95% confidence interval [CI] = 1.9-380), as was the use of fungicides (OR = 3.3; CI = 0.8-13). Residing on a farm, ranch or in a rural area during this time period was protective of female fertility. Households supplied with central Wisconsin groundwater were at less risk for infertility than households using municipal sources (OR = 0.6; CI = 0.4-0.9). Behavioral risk factors included alcohol consumption (OR = 1.8; 1.2-2.5), smoking (1.6; 0.9-2.9), passive smoke exposure (1.8; 1.2-2.5), steady weight gain in adult life (3.5; 2.0-6.1), and having a male partner over the age of 40 (4.5; 1.2-16.3). Drinking 3 or more glasses of milk per day was protective of female fertility (0.3; 0.1-0.7). CONCLUSION: These results suggest that certain agricultural, residential and lifestyle choices may modify the risk of female infertility Am J Epidemiol. 1997 Feb 15;145(4):324-34. Related Articles, Links Caffeine intake and delayed conception: a European multicenter study on infertility and subfecundity. European Study Group on Infertility Subfecundity. Bolumar F, Olsen J, Rebagliato M, Bisanti L. Department of Public Health, Alicante University, Spain. The effects of caffeine consumption on delayed conception were evaluated in a European multicenter study on risk factors of infertility. Information was collected retrospectively on time of unprotected intercourse for the first pregnancy and the most recent waiting time episode in a randomly selected sample of 3,187 women aged 25-44 years from five European countries (Denmark, Germany, Italy, Poland, and Spain) between August 1991 and February 1993. The consumption of caffeinated beverages at the beginning of the waiting time was used to estimate daily caffeine intake, which was categorized as 0-100, 101-300, 301-500, and > or = 501 mg. Risk of subfecundity (> or = 9.5 months) and the fecundability ratio, respectively, were assessed by logistic regression and Cox proportional hazard analyses, adjusting for age, parity, smoking, alcohol consumption, frequency of intercourse, educational level, working status, use of oral contraceptives, and country. A significantly increased odds ratio (OR) of 1.45 (95% confidence interval (CI) 1.03-2.04) for subfecundity in the first pregnancy was observed for women drinking more than 500 mg of caffeine per day, the effect being relatively stronger in smokers (OR = 1.56, 95% CI 0.92-2.63) than in nonsmokers (OR = 1.38, 95% CI 0.85-2.23). Women in the highest level of consumption had an increase in the time leading to the first pregnancy of 11% (hazard ratio = 0.90, 95% CI 0.78-1.03). These associations were observed consistently in all countries as well as for the most recent waiting time episode. The authors conclude that high levels of caffeine intake may delay conception among fertile women. Human Reproduction, Vol. 16, No. 2, 370-373, February 2001 © 2001 European Society of Human Reproduction and Embryology Selected food intake and risk of multiple pregnancies Fabio Parazzini1,2,4, Liliane Chatenoud1, Gaia Bettoni3, Luca Tozzi3, Simonetta Turco3, Matteo Surace1, Elisabetta Di Cintio1 and Guido Benzi1 Abstract In order to explore the association between multiple birth risk and diet, data were analysed from a case-control study on risk factors for multiple births conducted in Italy between 1988 and 1998. A total of 185 cases (median age 30 years) were interviewed: 36 women delivered monozygotic and 149 delivered spontaneous dizygotic multiple births. The control group comprised 498 women who gave birth at term (>37 weeks gestation) to healthy infants on randomly selected days at the same clinic. Women were specifically excluded if they reported a history of multiple pregnancy or they had received treatment for infertility for the index pregnancy. No marked differences emerged in daily intake between cases and controls and a total of 35 foods items, including the major sources of beta-carotene, retinol, ascorbic acid, vitamin D, E, methionine folate and calcium in the Italian diet. Likewise intake of selected micronutrients was largely similar in dizygotic cases, monozygotic cases and controls, with the only exception of a slightly lower intake of folates in dizygotic pregnancies in comparison with controls: this difference was statistically significant (P < 0.05), but limited in quantitative terms (mean daily intake of folate 192.4, 183.2 and 191.4 µg respectively in monozygotic, dizygotic cases and controls). In conclusion, the results of this study do not support the role of diet in the development of multiple births. Key words: diet/epidemiology/foods/multiple births/risk factor Introduction Several observations have linked the intake of various nutrients/dietary factors to reproduction. There is now some evidence that low intake of salad or high intake of vitamin A increases the risk of malformations (Czeizel and Dudas, 1992 ; Czeizel et al., 1994a ). Further, deficiencies of proteins or vitamin A have been associated in animals with the risk of miscarriage (O'Toole et al., 1974 ) and in humans of hydatidiform mole (Berkowitz et al., 1985 ; Parazzini et al., 1988 ). With regard to multiple births, deprivation/low dietary intake during World War II has been suggested to explain the peak in twinning rates after the end of World War II observed in several countries (Parazzini et al., 1998 ; Bortolus et al., 1999 ). Otherwise, an association between vitamin supplementation and subsequent multiple birth has been reported in an Hungarian trial (Czeizel, 1993 ; Czeizel et al., 1994b ). However this finding has not been confirmed in the Medical Research Council (MRC) study and in the prospective study of nutrition, smoking and pregnancy outcome conducted in the UK (MRC Vitamin Study Research Group, 1991 ; Mathews et al., 1999 ). In order to explore the association between multiple birth risk and diet, data were analysed from a case control study on risk factors for multiple births conducted in Italy. Top Abstract Introduction Materials and methods Results Discussion References Materials and methods The general design of this study has been previously described (Parazzini et al., 1993 , 1996 ). Briefly, between January 1988 and March 1998, a case-control study was conducted on risk factors for multiple pregnancies. Trained interviewers identified and questioned cases and controls using a standard questionnaire. Multiple births in patients who received treatments for infertility (assisted reproduction techniques or treatment for ovulation induction) were not included. An effort was made to define the zygosity. Between January 1988 and February 1989, the cases included in the study were women who delivered different sex multiple births at the Clinica Luigi Mangiagalli (the largest maternity hospital in Milan). In the periods 1989–1990 zygosity was defined on the basis of chromosome polymorphism in leukocytes (Paris Conference 1971, 1972 ), consequently all monozygotic twins included in the study were collected in that period. In other calendar periods, cases collected were women who delivered different sex multiple births only. A total of 185 cases (median age 30 years) was interviewed: 36 women delivered monozygotic and 149 dizygotic multiple births. Of these, one delivered three babies. The control group comprised women who gave birth at term (>37 weeks gestation) to healthy infants on randomly selected days at the same clinic. Women were specifically excluded if they reported a history of multiple pregnancy or they had received treatment for infertility for the index pregnancy. A total of 498 control women (median age 30 years) were interviewed. Less than 2% of cases and controls refused to be interviewed. The present report is based on data collected until March 1998. Information was collected on general sociodemographic characteristics, personal habits, gynaecological and obstetric history. Further, the weekly frequency of consumption of 35 food items before conception diagnosis was elicited, including the major sources of betacarotene, retinol, ascorbic acid, vitamin D and E, methionine, folate and calcium. Information on portion size was also collected (small/average/large). The micronutrient intake of the food items considered was computed by multiplying the consumption frequency of each unit of food by the nutrient content of the standard average portions, using the Italian tables of food composition (Fidanza and Verdiglioni, 1988 ) integrated by other sources, when required (Souci et al., 1986 ; Paul and Southgate, 1988 ). Statistical analysis The odds ratios (OR) and their 95% confidence intervals (CI) were calculated as estimates of relative risk of multiple birth for selected factors including education, family history of multiple birth and parity. To account simultaneously for the effects of age and those factors, unconditional multiple logistic regression with maximum likelihood fitting was used (Breslow and Day, 1980 ). Means and SD of food intake items were calculated using age, years of education, parity and family history as co-variates. When means of micronutrients were calculated, total energy intake was added to the other co-variates listed above. The distribution of cases and controls according to selected characteristics is shown in Table I . Dizygotic cases were less frequently parous and less educated than controls. A family history of multiple birth was more frequently reported both from dizygotic and monozygotic cases. View this table: Table I. Distribution of cases and controls according to age and [in this window] selected factors [in a new window] Table II shows the estimated mean daily intake of considered foods. Mean values of selected micronutrients such as beta-carotene, folate and calcium for cases and controls respectively are shown in Table III . No marked differences emerged in daily intake between cases and controls of considered foods. Likewise, intake of selected micronutrients was largely similar in dizygotic, monozygotic cases and controls with the only exception of a slightly lower intake of folates in dizygotic pregnancies in comparison with controls: the difference was statistically significant (P < 0.05), but limited in quantitative terms. View this table: Table II. Mean and SD of weekly intake of selected food items [in this window] [in a new window] View this table: Table III. Mean and SD daily intake of selected micronutrients [in this window] [in a new window] Top Abstract Introduction Materials and methods Results Discussion References Discussion Limitations of this study should be considered. Dizygotic and monozygotic multiple pregnancies represent two different entities, thus any analysis of determinants of risk of multiple births should consider them separately. Unfortunately detailed information on zygosity was available only for cases interviewed during a limited period. Thus, although information was collected on about 185 multiple pregnancies, monozygotic pregnancies were only 36. Consequently, numbers were limited for formal statistical evaluation or inference on the differences between the two entities. Information was collected while women were in hospital for delivery. The food frequency questionnaire was tested for reproducibility (D'Avanzo et al., 1997 ), but not validated. However, any potential problem of validation is unlikely to have produced any major misclassification between cases and controls. In addition, at the time of data collection, the possible relationship between diet and multiple birth was almost certainly unknown to interviewers and most of the women interviewed. Only a small portion of the questionnaire was related to dietary factors, so the interviewers' and patients' attention was probably not concentrated on those aspects. Information was limited to only a few dietary items, in terms of usual number of portions per week. Still, the food groups investigated include the major sources of carotenoids and folates (vegetables and fruit), as well retinoids, vitamins and calcium (milk, cheese and eggs in Italy). Selection bias is also unlikely to have produced marked effects, especially since cases and controls were recruited in the same institutions and participation was practically complete. The choice of control women who delivered healthy infants at term may have introduced some potential bias. A low caloric intake may be associated with low birth weight infants. Since women who gave birth to low birth weight infants were not included in the control group, but were included among cases, an association between diet and multiple births may arise. However, the inclusion and exclusion of cases who delivered low birth weight infants did not markedly change the result of this analysis (data not shown). Further, allowance was made for potential confounders, including indicators of socio-economic status, and other major known or likely determinants of the risk of multiple births. Bearing in mind these limitations, the results of this study do not show any association between selected dietary factors considered including milk, cheese and potatoes and risk of multiple birth. Published findings on the relationship between diet/vitamin intake and multiple births are scanty and controversial. Nylander (Nylander, 1979 ) noted that in Nigeria the dizygotic twinning rate was four times higher in lower social class than in upper social class women. He suggested that such a high incidence might be due to the presence in the diet of oestrogen-like substances. Also, food storage conditions were suggested to have some influence on hormonal concentrations. For example zearalenone, a mycotoxin, may have an oestrogenic potency. Some findings from a Hungarian randomized controlled trial have suggested that periconceptional multivitamin supplementation may increase the rate of multiple births (Czeizel, 1993 ; Czeizel et al., 1994b ). Similar findings, although not completely consistent, also emerged from a re-analysis of data sets of three American studies on risk factors for congenital malformations (Werler et al., 1997 ). Other randomized studies, however, did not confirm these findings (MRC Vitamin Study Research Group, 1991 ; Mathews et al., 1999 ). No association was found between selected food intake (including major sources of vitamins in Italian diet) and risk of multiple births in the current study. In particular, estimated intakes of vitamins were not associated with the risk of dizygotic and monozygotic pregnancies. Although amounts of vitamins may be more elevated after supplementation than those due to diet intake, the results of this study do not support the existence of a major role of diet in the development of multiple births. Notes 4 To whom correspondence should be addressed at: Istituto di Ricerche Farmacologiche `Mario Negri', Via Eritrea 62, 20157 Milano, Italy. E-mail: parazzini@irfmn.mnegri.it Top Abstract Introduction Materials and methods Results Discussion References References Berkowitz, R.S., Cramer, D.W. and Bernstein, M.R. (1985) Risk factors for complete molar pregnancy from a case control study. Am. J. Obstet. Gynecol., 152, 1016.[ISI][Medline] Bortolus, R., Parazzini, F., Chatenoud, L. et al. (1999) The epidemiology of multiple births. Hum. Reprod., 5, 179–187.[Abstract] Breslow, N.E. and Day, N.E. (1980) Statistical Methods in Cancer Research, vol. 1. The Analysis of Case Control Studies. IARC Science Publishers, number 32. Czeizel, A.E. (1993) Controlled studies of multivitamin supplementation on pregnancy outcomes. Ann. NY Acad. Sci., 678, 266–275.[Abstract] Czeizel, A.E. and Dudas, I. (1992) Prevention of the first occurrence of neural tube defects by periconceptional vitamin supplementation. N. Engl. J. Med., 327, 1832– 1835.[Abstract] Czeizel, A.E., Dudas, I. and Metneki, J. (1994a) Pregnancy outcomes in a randomised controlled trial of periconceptional multivitamin supplementation. Arch. Gynecol. Obstet., 255, 131–139.[ISI][Medline] Czeizel, A.E., Metneki, J. and Dudas, I. (1994b) The higher rate of multiple births after periconceptional multivitamin supplementation: an analysis of causes. Acta Genet. Med. Gemellol., 43, 175–184.[Medline] D'Avanzo, B., La Vecchia, C., Katsouyanni, K. et al. (1997) An assessment, and reproducibility of food frequency data provided by hospital controls. Eur. J. Cancer Prev., 6, 288–293.[ISI][Medline] Fidanza, F. and Verdiglioni, N. (1988) Tabelle di composizione degli alimenti. In Fidanza, F. and Liguori, G. (eds), Nutrizione umana. Idelson, Naples, pp. 677–730. Mathews, F., Murphy, M., Wald, N.J. et al. (1999) Twinning and folic acid use. Lancet, 353, 291–292.[ISI][Medline] MRC Vitamin Study Research Group (1991) Prevention of neural tube defects: results of the Medical Research Council vitamin study. Lancet, 338, 131–137.[ISI][Medline] Nylander, P.P. (1979) The twinning incidence of Nigeria. Acta Genet. Med. Gemellol., 28, 261–263.[Medline] O'Toole, B.A., Fradkin, R., Warkany, J. et al. (1974) Vitamin A deficiency and reproduction in Rhesus monkeys. J. Nutr., 104, 1513–1524.[ISI][Medline] Parazzini, F., La Vecchia, C., Mangili, G. et al. (1988) Dietary factors and risk of trophoblastic disease. Am. J. Obstet. Gynecol., 158, 93–99.[ISI][Medline] Parazzini, F., Tozzi, L., Ferraroni, M. et al. (1993) Risk factors for multiple births. Acta Obstet. Gynecol. Scand., 72, 177–180.[ISI][Medline] Parazzini, F., Chatenoud, L., Benzi, G. et al. (1996) Coffee and alcohol intake, smoking and risk of multiple pregnancy. Hum. Reprod., 11, 2306–2309.[Abstract] Parazzini, F., Benzi, G., La Vecchia, C. et al. (1998) Temporal trends in twinning rates in Italy around World War II. Hum. Reprod., 13, 3279–3280.[Free Full Text] Paris Conference, 1971 (1972) Standardization in human cytogenetics. In Birth defects. Orig. Art. Ser., 7, The National Foundation, New York. Paul, A.A. and Southgate, D.A.T. (1988) The Composition of Foods. HMSO, London. Souci, S.W., Fachmann, W. and Kraut, H. (1986) Food Composition and Nutrition Tables 1986/87, 3rd edn. Wissenschaftliche Verlagsgesellschaft, Stuttgart. Werler, M.M., Cragan, J.D., Wasserman, C.R. et al. (1997). Multivitamin supplementation and multiple births. Am. J. Med. Genet., 71, 93–96.[ISI][Medline] Men Two capsules contain: Vitamin C as ascorbic acid 120 mg • Vitamin E as d-alpha tocopherol 150 mg • Vitamin B6 as pyridoxine hydrochloride 2 mg • Vitamin B12 as cyanocobalamin 6 mcg • Folate as folic acid 400 mcg • Zinc as gluconate 15 mg • Selenium as sodium selenate 70 mcg • Proprietary Blend 610 mg: L-Carnitine as tartrate, Dong Quai (standardized to .1% ferulic acid), Coenzyme Q10. Inactive Ingredients: Rice Flour Powder, Magnesium Stearate, Silica. Balercia G, Mosca F, Mantero F, et al. Coenzyme Q10 supplementation in infertile men with idiopathic asthenozoospermia: an open, uncontrolled pilot study. Fertil Steril 2004;81:93-8. Wong WY, Merkus HM, Thomas CM, et al. Effects of folic acid and zinc sulfate on male factor subfertility: a double-blind, randomized, placebo-controlled trial. Fertil Steril 2002;77:491-8. close window nfertility. Taking L-carnitine orally, in combination with acetyl-L-carnitine for 6 months seems to increase sperm motility in men with infertility (12352). Some pregnancies occured after taking these carnitines, but not enough to be statistically significant (12352). Taking L-carnitine orally, in combination with acetyl-L-carnitine and nonsteroidal anti-inflammatory drugs, seems to increase sperm count and motility in men with infertility caused by abacterial prostatovesiculoepididymitis; an inflammation of the prostate gland, seminal vesicles, and epididymis. L-carnitine supplementation should follow 2 months of treatment with nonsteroidal anti-inflammatory drugs (9791). Vicari E, La Vignera S, Calogero AE. Antioxidant treatment with carnitines is effective in infertile patients with prostatovesiculoepididymitis and elevated seminal leukocyte concentrations after treatment with nonsteroidal anti-inflammatory compounds Infertility. In one study, males with asthenospermia or oligoasthenospermia, receiving oral vitamin E supplementation, achieved impregnation at a rate of 21% compared to none for similar patients receiving placebo (4695). In another study, males enrolled in an in vitro fertilization program who had previously had low fertilization rates were treated with oral vitamin E for three months. Fertilization rates increased significantly from 19% to 29% after one month of treatment (3583). In a crossover trial, males found to have elevated reactive oxygen species in their semen, which might be associated with infertility, were treated with oral vitamin E. After treatment, in vitro sperm binding to the zona pellucida was significantly increased (4693). Interestingly, high-dose vitamin E in combination with vitamin C does not seem to offer any benefit to sperm functionality (4696). Vitamin E plus selenium seems to improve sperm functionality, but doesn't improve fertilization rates (3585). Although vitamin E preparations used alone appear to offer some benefit in men with asthenospermia or oxidative damage to sperm, combining vitamin E with vitamin C or selenium does not appear to be beneficial. Studies did not differentiate between different forms of vitamin E. Sci Total Environ. 1998 Jun 18;214:165-74. Related Articles, Links Hong Kong male subfertility links to mercury in human hair and fish. Dickman MD, Leung CK, Leong MK. Ecology and Biodiversity Department, University of Hong Kong, Hong Kong. dickman@hkusua.hku.hk The focus of the present study was on the relationship between Hong Kong male subfertility and fish consumption. Mercury concentrations found in the hair of 159 Hong Kong males aged 25-72 (mean age = 37 years) was positively correlated with age and was significantly higher in Hong Kong subjects than in European and Finnish subjects (1.2 and 2.1 ppm, respectively). Mercury in the hair of 117 subfertile Hong Kong males (4.5 ppm, P < 0.05) was significantly higher than mercury levels found in hair collected from 42 fertile Hong Kong males (3.9 ppm). Subfertile males had approx. 40% more mercury in their hair than fertile males of similar age. Although there were only 35 female subjects, they had significantly lower levels of hair mercury than males in similar age groups. Overall, males had mercury levels that were 60% higher than females. Hair samples collected from 16 vegetarians living in Hong Kong (vegans that had consumed no fish, shellfish or meat for at least the last 5 years) had very low levels of mercury. Their mean hair mercury concentration was only 0.38 ppm Fertil Steril. 2002 Dec;78(6):1187-94. Related Articles, Links Role of environmental estrogens in the deterioration of male factor fertility. Rozati R, Reddy PP, Reddanna P, Mujtaba R. Assisted Conception Services Unit, Mahavir Hospital and Research Center, Hyderabad, India. drrozati@rediffmail.com OBJECTIVE: To evaluate the role of the environmental estrogens polychlorinated biphenyls (PCBs) and phthalate esters (PEs) as potential environmental hazards in the deterioration of semen parameters in infertile men without an obvious etiology. DESIGN: Randomized controlled study. SETTING: Tertiary care referral infertility clinic and academic research center. PATIENT(S): Twenty-one infertile men with sperm counts <20 million/mL and/or rapid progressive motility <25% and/or <30% normal forms without evidence of an obvious etiology and 32 control men with normal semen analyses and evidence of conception.Semen and blood samples were obtained as part of the treatment protocol. MAIN OUTCOME MEASURE(S): Evaluation of semen parameters such as ejaculate volume, sperm count, motility, morphology, vitality, osmoregulatory capacity, sperm chromatin stability, and sperm nuclear DNA integrity. RESULT(S): PCBs were detected in the seminal plasma of infertile men but not in controls, and the concentration of PEs was significantly higher in infertile men compared with controls. Ejaculate volume, sperm count, progressive motility, normal morphology, and fertilizing capacity were significantly lower in infertile men compared with controls. The highest average PCB and PE concentrations were found in urban fish eaters, followed by rural fish eaters, urban vegetarians, and rural vegetarians. The total motile sperm counts in infertile men were inversely proportional to their xenoestrogen concentrations and were significantly lower than those in the respective controls. CONCLUSION(S): PCBs and PEs may be instrumental in the deterioration of semen quality in infertile men without an obvious etiology.