Management of mild preeclampsia
advertisement

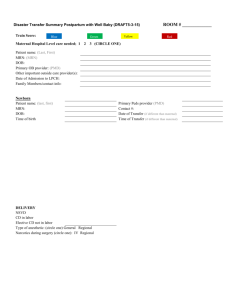
4 Diagnosis : Management of mild preeclampsia 1. BP 140/90 mmHg in previous normotensive patient 2. with proteinuria 300 mg in 24 hrs or 1 + from Dipstick of random Assess maternal status Assess fetal status Clinical of SPE Admit NST or FAS Ix: CBC, PT, PTT, Plt count, BUN, Cr, SGOT, +U/S for fetal growth, AF, placenta SGPT, 24-hr urine for protein & creatinine Non-reassuring MPE with reassuring fetal test fetal test Dx SPE GA < 37 wks GA 37 wks Consider delivery Serial maternal assessment Terminate pregnancy depend on GA Symptoms & signs of SPE Daily BW, & proteinuria BP qid, urine output Ripe or wait Unripe Other Serial fetal assessment cervix if clinical stable cervix OB indications Clinical - fundal height, FHS (GA 40 wks) Daily FMC NST/FAS twice a week , + U/S Induction - Beware of SPE Intrapartum - Steroid for GA < 34 wks - Continued assess mother Not response Response - Beware of SPE Maternal :develop SPE c stable maternal - Continuous fetal monitoring (clinical or lab Ix) & fetal conditn Fetal compromise Response Failed - Monitor until Induction If GA 37 wks Vaginal C/S any delivery conditions (close monitoring for OPD case) - ANC weekly (clinical, BP, proteinuria) - NST/FAS 1-2/wk - + U/S q 1-2 wk SPE management (if develop SPE) Stable patient Terminate Pregnancy Terminate Pregnancy 5 Management of severe preeclampsia Admit • Prevention of convulsion ( 1st line = MgSO4) • Antihypertensive Rx if diastolic > 110 mmHg or systolic > 160 mmHg* • Assess maternal status • Assess fetal status Ix : CBC, PT, PTT, Plt count, Clinical : fundal height, FHS BUN, Cr, LFT, U/A, NST + 24-hr urine for protein & creatinine +U/S : EFW, growth, AF volume, placenta, (If still not done) presentation, R/O hydrops fetalis, twins • IV fluid : Acetar 1000 cc rate 80 – 120 cc/hr • Record V/S q 1 hr, retain Foley catheter • Record urine output q 1 hr & Record I/O OD • Beware of eclampsia • No diuretics unless pulmonary edema is developed • Continuous fetal monitoring GA < 24 wks GA 24 - < 32 wks GA > 32 wks • Termination of pregnancy • Optional expectant Rx • Termination of pregnancy (after counseling (Only selected case ** - If GA < 34 wks :corticosteroid Risk & benefit) after counseling risk & benefit) - delivery within 24 hrs • corticosteroid 0f onset of symptoms Corticosteroid Favorable Other Continued anticonvulsant for 48 hrs cervix OB indications Closed monitor maternal & fetal status or Daily Ix : CBC, PT, PTT, Plt cont, Induction unfavorable LFT, BUN, Cr cervix Termination of pregnancy Response Failed If 1. GA > 32 wks induction or 2. worsening maternal or fetal condition Vaginal C/S delivery • Continue anticonvulsant Until 24 hrs postpartum or after seizure • Control BP, keep diastolic 90-105 mmHg (antihypertensive drug may be oral form) • Beware of late postpartum eclampsia • F/U 2 wk after discharge 6 ** Expectant Rx is NOT recommended in > 1 of the followings : 1. uncontrolled severe HT (systolic BP > 160 mmHg or diastolic BP > 105 mmHg despite max. recommended dose of antiHT) 2. eclampsia 3. platelet count < 100,000/µ1 4. AST / ALT > 2x upper normal limit with epigastric / RUQ pain 5. pulmonary edema 6. compromised renal function (rise in serum creatinine of 1 mg/dl over baseline level) 7. abruption placentae 8. persistent severe headache or visual changes 9. worsening fetal condition 10. HELLP syndrome 11. significant hematological, cerebral or liver abnormalities due to preeclampsia - If severe preeclampsia develops before GA 34 wks, antiphospholipid syndrome should he investigate. - If eclampsia develops, delivery should occur within 12 hrs of the onset of convulsions. Anticonvulsant therapy Drug Initial dose Maintenance Antidote Monitor Recurrent dose convulsion MgSO4 (1st line) 4-5 g (10% MgSO4) iv. rate < 1 g/min 20 g of 50% MgSO4 In 5% D/W 500 ml iv. drip 25-50 ml/hr (1-2 g/hr) 10% calcium gluconate 10 ml iv. Over 3 min a. patellar reflex = present b. urine output > 100 ml/ 4 hr or > 25 ml/hr. c. RR > 14/min Repeat 2 g of 10% MgSO4 iv. & recheck Mg2+ level Remarks - If next dose of MgSO4 cannot be given, reassess a., b. and c. q 30 mins. And retreat when a., b. and c. meet the above criteria. - If convulsion develops during giving maintenance dose of MgSO4 phenytoin 125 mg iv. (dose up to 250 mg iv. Over 3-5 min) or diazepam 10 mg iv. May be considered. - Mg2+ level * Therapeutic level of Mg2+ = 4.8 – 8.4 mg/dl * 8-10 mEq/L patellar reflexes lost * 10-15 mEq/L respiratory depression * 12-25 mEq/L respiratory paralysis * 25-30 mEq/L cardiac arrest - Renal disease * initial dose : safe * creatinine > 1.3 mg/dl im. Dose 50% iv. 1 g/hr. check Mg2+ level (ลดลง 50% ของ dose IM) 7 Antihypertensive therapy Dihydralazine ( Nepresal, Apresoline ®) Preparation : 25 mg/ml. Test dose : 1 mg iv. Over 1 min, monitor BP q 5-10 min (to avoid idiosyncratic hypotensive effect) Treatment dose: 5-10 mg iv. Over 2-4 min monitor BP q 5 min for 20 min later * If no effect (BP not ) : repeat dose. * If optimal effect – not repeat dose until diastolic BP > 110 mmHg Maximum dose : Total 30 mg – if can not control BP, then switch to another regimen Cardepine (Nicardipine HCl) Preparation : 2 mg/2ml ampoule Treatment dose : I. IV. Bolus : 2 mg/2ml ampoule + saline 2 ml. (o.5mg/ml) 0.5 mg (1 ml) iv. Over 1-2 min monitor BP q 5 min for 15 min * If no effect (BP not ) : repeat dose q 15 min * If optimal effect – not repeat dose until diastolic BP > 110 mmHg »» if patien’s BW > 80 kg, initial start dose @ 1 mg (2ml) «« II. IV. Drip : 10 mg in 5% D/W 100 ml. (0.1 mg/ml) start at 2 mg./hr (20 µd/min) * If no optimal effect (BP not ) : 2 mg/hr (20 µd/min) dose q 15 min) Maximum dose : 10 mg/hr Nifedipine (Adalat ®) Preparation : 10, 20 mg/capsule Treatment dose : 10 mg oral monitor BP q min for 15 min later Repeat dose in 30 min if necessary »» Beware of synergistic interaction with MgSO4 that causes severe hypotension. «« Maximum dose : 120 mg/d 8 Management of eclampsia Assess maternal status (same as SPE) Unstable Maternal condition Management According to Conditions Eclampsia Do not leave patient alone Call for help Left lateral position Oxygen Assess airway & breathing Check pulse & BP Pulse oximetry MgSO4 control convulsion Antihypertensive drugs as indicated Lab. Investigation Assess fetal status (same as SPE) Stable maternal condition Reassuring fetal status Non-reassuring fetal status * Plan to deliver (delivery within 12 hrs after onset of convulsion) Cervix Unripening Ripening of cervix * Induction of labor * IV fluid : LRS 80 ml/hr * Record vital signs q 1 hr * Record I/O OD, Record urine output q 1 hr * Beware complication of eclampsia * Continuous electronic fetal monitoring * GA < 34 wks : corticosteroid Response Failed induction C/S Vaginal delivery * Continue MgSO4 : 24 hrs postpartum or after last seizure * Control BP keep diastolic < 110 mmHg 9 เอกสารอ้างอิง 1. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap III L, Wenstrom KD. Williams Obstetrics, 22nd ed. USA: McGraw-Hill; 2006.p. 761-87,1210-20. 2. Roberts JM. Pregnancy-related hypertension. In : Creasy RK, Resnik R, editors. Maternal-fetal medicine : principles and practice. 5th ed. Philadelphia : Saunders; 2004. p. 859-93. 3. American College of Obstetricians & G7necologists. Diagnosis and management of preeclampsia and eclampsia. ACOG Pract Bull 2002;(33). 4. American College of Obstetricians & Gynecologists. Chronic hypertension in pregnancy. ACOG Pract Bull 2001; (29). 5. Clin Obstet Gynecol 1999;42:470-8. 6. Clin Obstet Gynecol 2004;47:118-273. 7. Gregg AR. Hypertension in pregnancy. Obstet Gynecol Clin N Am 2004;31:223-41. 8. The Royal Women’s Hospital. Clinical practice guidelines, pre eclampsia : management. Available on line at : http://www.rwh.org.au/rwhcpg/maternity.cfm?doc-id=3403 9. Tuffnell DJ, Shennan AH, Waugh JJ, Walker JJ. The management of severe pre-eclampsia. Royal College of Obstetricians and Gynecologists; 2006 Mar. 11 p. (Guideline; no. 1 (A))