Drafting Session Outcomes - Group on Earth Observations

DS-06 Disease Early Warning
Suggest change title to: “Human Health and Environment”
Definition (Note: This para was already agreed by Plenary)
Ensure access to human information and tools to support the global community of human health and environment experts. Increase the use of environmental information and tools to support decision making in epidemics and/or disease management and planning for well-being. Apply outcomes from other Societal Benefit Areas to improve health and well-being (Health
Strategic Target).
The CoP felt that the above does not capture the public health driven approach and would like to suggest replacing “improved” with “health relevant environmental”
Comments and observations:
1. Understand what are the human health problems that relate to the environment
2. Identify the relevant information for decision making
3. Training, capacity building
4. Promote the use of information
Gaps were identified over the first 5 years that more focus is needed on the first 3 items, particularly engagement of public health requirements and users.
Parking lot:
- risk factors; risk assessment; criteria for decisions
- “Environment” in public health could include radiation, food… etc which is not natural environment
- Disease burden should be considered (at present environmental factors are not needed to define burden) – burden could be used to identify observation priorities
- Need of qualitative deliverables
- Other SBAs state: - Standards of; systems of; network of; reporting mechanisms; standardized classifications; support for countries
- Institutional point of view needed: also political advocacy
- Geographic domain
- Linkages with other Societal Benefit Areas: Disasters, Biodiversity, ecosystem, and Water
Deliverables (2012-2015)
(General -- vertical)
1. Understand what are the human health problems that relate to the environment
2. Identify the relevant information for decision making
3. Training, capacity building
4. Promote the use of information
(Specific -- horizontal)
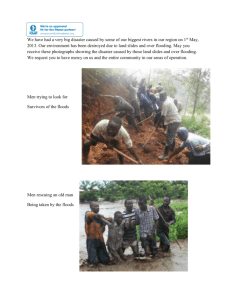
1. Advancing Tools and Information for Health Decision-making a. Vector-borne diseases (Ramesh and Murielle)
Malaria, RVF, Dengue, Lyme disease, (lepto)
Link to: Ecosystems and BD, Disaster (Floods, earthquakes cyclones, tsunami etc.) - malaria b. Water-borne diseases and risk (Juli, Kym, Eric)
Cholera and other vibrios, leptospirosis, harmful algae bloom, climate vulnerability on assessment of water sanitation access
Link to: Disaster (Floods etc) – cholera and leptospirosis c. Air-borne diseases (John/Richard, Michel) meningitis, influenza d. Air quality and aeroallergens (Kym, Hillel) sand and sust, AIRNow, pollen, asthma, cardio vascular diseases
Link to: Ecosystems and Biodiversity e. Pollutants and contaminants (Ana, Nicola)
Mercury, POPs
Link to: Disaster (Floods etc)
2. New Technologies for monitoring, surveillance and tracking
(Andreas)
In-situ sensor for health and environmental factors
Background Document Template
Each project to develop a background document justifying the need for undertaking projects to achieve the above mentioned.
- Engage health decision makers to identify the problem
- Understand what are the human health problems that relate to the environment
- Identify the relevant information for decision making
- What is the existing capacity and resources
- Training, capacity building
- Promote the use of information
- Global Status, Best practices
- Funding
Timeline
Template by 5 th April
Fist draft by 20 April
Circulate and review
Ramesh and others to present at 4-6 May Work Plan Symposium
Parking Lot - Write up by John on Influenza
Assess current activities, needs, and priorities in the use of Earth observations for the surveillance, modeling and prediction of seasonal influenza and the early detection of pandemic influenza (best practices meeting). The goal will be to identify observation priorities, gaps in knowledge, and overlaps in current activities -- while preserving overlaps that would lend to comparison and cross-validation of techniques.
Expand the availability, use, and application of environmental and influenza monitoring data among the respective members.
Fully engage end users including WHO, PAHO, CDC and others. Encourage participation of CoP in symposiums and conferences sponsored by end users.