pubdoc_10_15902_381
advertisement

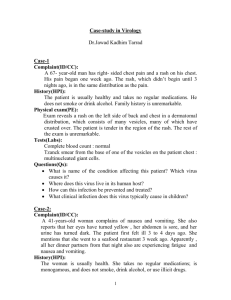
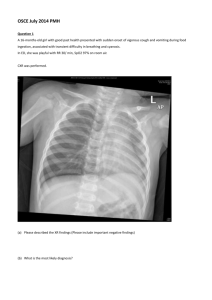
University of Babylon Case-study in Microbiology Dept. of microbiology College of Medicine _______________________________________________________________________________ Case-study in Bacteriology (Prof. Dr. Alaa Al-Charrakh): 1- Five children from the same school presented with abdominal pain and diarrhoea (streaked with blood) over a period of 3 days. Upon investigation it was found that one of the children had recently been abroad with his family. Fecal specimen was collected and sent to microbiology lab. Many pus cells on direct microscopy and non-lactose fermenting colonies were found on MacConkey’s agar. On motility test it was non-motile a. What is the identity of the organism? b. What is the mode of spread? 2- A 30 years old man presented to out-patient gastroenterology clinic with the complaints of: -Changed taste & bad breath -Recurrent epigastric pain & heart burn On gastroscopy he was diagnosed as having gastric ulcer. A biopsy was taken and sent to microbiology lab: a) What tests will be performed on the biopsy specimen? b) What is the likely organism causing the disease? c) What other lab tests will help to confirm the identity of the organism? 3- A previously normal, full-term infant developed bilateral conjunctivitis at 2 weeks of age. The conjunctivitis was followed by severe coughing, but the infant remained afebrile. When the infant was 4 weeks old, a chest X-ray showed bilateral symmetrical interstitial infiltrates. The white blood cell (WBC) count was 14,000/mm3 with 32% segmented neutrophils, 58% lymphocytes, 2% monocytes, and 4% eosinophils. Which of the following is the most probable infectious agent? A. Chlamydia trachomatis B. Streptococcus agalactiae C. Haemophilus influenza D. N. meningococcus 4. A 16-year-old girl was admitted to a Merjan teaching hospital because of hypotension, cyanosis, high fever (39.9°C), and bilateral, non-fluctuant, inguinal, and axillary lymphadenopathy. The patient died the same day. Blood cultures obtained on admission were positive for bipolar-staining, short, gram-negative bacilli. What is the most probable etiologic agent? A. Yersinia pestis B. K. rhinoscleromatis C. Francisella tularensis D. Brucella abortus 5- A woman brings her 2 ½-year-old child to the physician with complaints that the child is suffering ear pain and drainage, fever, lethargy and irritability. After examining the child, the doctor explains to the mother that the child has an ear infection. The physician prescribes a 7-day course of amoxicillin for the child. After 5 days, the mother and the child return to the physician’s office. The child’s condition has not improved and she still has pain and fever. The physician switches the infant to a 7-day prescription of amoxicillin/clavulanate (Augmentin) and the symptoms clear. What are possible explanations for this child’s initial lack of response to therapy and subsequent recovery? Case-study in Immunology: Q1/ An 18-year-old student with end-stage renal failure due to chronic glomerulonephritis was given a cadaveric kidney transplant. He had been on maintenance haemodialysis for 2 months, and on antihypertensive therapy for several years. His major blood group was A and his tissue type was HLA-A1, -A9, -B8, -B40, -Cw1, -Cw3, -DR3, -DR7. The donor kidney was also blood group A and was matched for one DR antigen and four of six ABC antigens. He was given triple immunosuppressive therapy with cyclosporin A, azathioprine and prednisolone. He passed 5 litres of urine on the second postoperative day and his urea and creatinine fell appreciably. However, on the seventh postoperative day, his graft became slightly tender, his serum creatinine increased and he had mild pyrexia (37.8°C). What is your diagnosis? How can you confirm it? Q2/A 48-year-old man was admitted for investigation of weight loss associated with intermittent diarrhoea. He had a history of pneumonia as a child and again as a young man working abroad. At the age of 33 he had developed chronic sinusitis, with persistent headaches. On examination he was thin but had no signs of malignancy. He had no clubbing and his chest was clear on auscultation. There was no lymphadenopathy and no hepatosplenomegaly. He was not anaemic, had a normal serum albumin and normal liver function tests. Immunological tests are shown in Table C3.3. No infective cause of the intermittent diarrhoea was found; barium enema was normal. Endoscopic examination of his maxillary sinuses showed considerable inflammation and hypertrophy of the mucosa. Serum immunoglobulins (g/l) IgG IgA IgM IgG1 IgG2 IgG3 IgG4 Antibody activity - post immunization IgG: tetanus toxoid diphtheria toxoid 7.2 <0.1 1.2 2.7 3.2 0.1 2.2 Negative [>0.85iu/ml] Negative [>0.2iu/ml] [6.5-12.0] [0.8-5.0] [0.5-2.0] [3.6-7.3] [1.4-4.5] [0.3-1.1] [0.1-1.0] pneumococcal polysaccharide Antibody activity - post exposure IgG: Rubella Measles Varicella zoster Blood lymphocyte subpopulations (x109/l) Total lymphocyte count T lymphocytes CD3 CD4 CD8 B lymphocytes CD19 Inadequate [>80U/ml] Not detectable Not detectable Not detectable 2.8 [1.5-3.5] 2.2 1.6 0.6 [0.9-2.8] [0.6-1.2] [0.4-1.0] 0.3 [0.2-0.4] *Normal adult ranges shown in brackets. What is your diagnosis? Q3/ A 25-year-old joiner presented with a 12-month history of an intensely itchy 'nettle rash' on his chest and back. The lesions appeared suddenly and lasted from 6 to 12h, to be replaced by new lesions at other sites. The lesions varied in size from a few millimetres to several centimetres. Attacks occurred two to three times each week. In addition, he had experienced four episodes of sudden swelling of lips which took 48h to subside. He said he looked as though he had been punched. He was unaware of any triggering factors and there was no personal or family history of atopy. His general health was excellent and he was not taking any medications. On examination, the lesions consisted of raised, red, irregular patches, some with white centres, and were typically urticarial. General examination was entirely normal. Laboratory investigations showed a normal haemoglobin and white cell count, with no eosinophilia. What type of immunological reaction is this case? Q4/ A 26-year-old West Indian man presented with a 24-h history of occipital headache and vomiting. He was pyrexial (temperature 38.3°C), confused, irritable and had marked neck stiffness with a positive Kernig's sign. There was no other history of serious infections. His immediate family were healthy. Lumbar puncture produced turbid cerebrospinal fluid (CSF) with a protein concentration of 4.5g/l (NR 0.1-0.4), glucose content of less than 0.1mmol/l (NR 2.5-4.0) and a leucocyte count of 8000/mm3 (97% neutrophils). Neisseria meningitidis was cultured from the CSF. A search was made for an underlying cause of his meningitis. X-rays of the skull and sinuses showed no abnormal communication with the CSF. The possibility of an underlying immune defect was then considered. What are you expect to find as an immunological abnormality in this case? Could it be a heritable disease? Q5/ A 77-year-old woman was referred from the Accident and Emergency Department, having been admitted overnight because of sudden onset of massive angioedema of her tongue associated with laryngeal stridor. She was treated with intravenous hydrocortisone only. This was her fifth such episode: an anaphylactoid attack 2 months earlier was severe enough for her to be intubated and ventilated on the Intensive Care Unit. She had no history of previous allergy and no family history of atopy. A drug history revealed that, in addition to oral prednisolone prescribed in the Accident and Emergency Department, she was taking oral frusemide and captopril. What is the cause of this case symptoms? How can you prevent it? Q6/ A 38-year-old woman was referred for investigation following an anaphylactic reaction whilst visiting a relative in hospital. She gave a 5-year history of recurrent conjunctival oedema and rhinitis when blowing up balloons for her children's birthday parties. In the year prior to admission, three successive visits to her dentist triggered marked angioedema of her face on the side opposite to that requiring dental treatment. The swellings took 48h to subside. On the day of admission, she visited a critically ill relative in hospital. The patient was being reverse barrier nursed and visitors were required to wear gown and gloves. About 20min after putting on the gloves her face and eyes became swollen, she felt wheezy and developed a pounding heart beat and light-headedness. Her tongue started to swell and she was taken to the Emergency Department where she was given intramuscular epinephrine (adrenaline) and intravenous hydrocortisone. She recovered rapidly but was kept under observation overnight. What is the diagnosis? What would you advise this patient? Case-study in Virology Dr.Jawad Kadhim Tarrad Case-1 Complaint (ID/CC): A 67- year-old man has right- sided chest pain and a rash on his chest. His pain began one week ago. The rash, which didn’t begin until 3 nights ago, is in the same distribution as the pain. History (HPI): The patient is usually healthy and takes no regular medications. He does not smoke or drink alcohol. Family history is unremarkable. Physical exam (PE): Exam reveals a rash on the left side of back and chest in a dermatomal distribution, which consists of many vesicles, many of which have crusted over. The patient is tender in the region of the rash. The rest of the exam is unremarkable. Tests (Labs): Complete blood count: normal Tzanck smear from the base of one of the vesicles on the patient chest: multinucleated giant cells. Questions (Qs): What is name of the condition affecting this patient? Which virus causes it? Where does this virus live in its human host? How can this infection be prevented and treated? What clinical infection does this virus typically cause in children? Case-2: Complaint (ID/CC): A 41-years-old woman complains of nausea and vomiting. She also reports that her eyes have turned yellow, her abdomen is sore, and her urine has turned dark. The patient first felt ill 3 to 4 days ago. She mentions that she went to a seafood restaurant 3 week ago. Apparently, all her dinner partners from that night also are experiencing fatigue and nausea and vomiting. History (HPI): The woman is usually health. She takes no regular medications; is monogamous, and does not smoke, drink alcohol, or use illicit drugs. Physical exam.(PE): A low-grade fever is present, and the patient is jaundiced. Abdominal exam reveals right upper quadrant tenderness and mild hepatomegaly. Tests (labs): Hemoglobin: 14 g/dL(normal 12-1 6g/dL) Alanine aminotransferase(ALT): 100 IU/L(normal 1-21 IU/L) Aspirate aminotransferase(AST): 98 IU/L(normal 7-27 IU/L) Bilirubin, total 3-2 mg/dL(normal : 0.1-1 mg/dL) Bilirubin, direct 1.6mg/dL( normal 0.1-0.4mg/dL) Alkaline phosphatase 42 IU/L(normal 13-39IU/L) Urinalysis : elevated urobilinogen ; negative for glucose, protein, and bacteria. Hepatitis A IgM : positive Hepatitis B panel: negative Hepatitis C IgM antibody: negative Hepatitis D IgM antibody: negative Questions (Qs): Given her history and lifestyle, how many of the four hepatitis viruses listed would the woman be unlikely to contact? What is the route of spread of HAV? Is there a chronic state for this virus? How is HEV transmitted? What is the link between hepatitis E and pregnancy? Is there a chronic carrier state this virus? Case-3 ID/CC A 30-year-old male presents with a high fever and chills, headache , nausea, vomiting, and muscle aches. HPI Yesterday he had an episode involving abnormal movements of his right hand and face (focal seizure). He also has difficulty comprehending speech and has olfactory hallucinations. He has no history of psychiatric illness. PE VS(Viral signs): tachycardia, mild tachypnea, normotention. PE: confused and disoriented, papilledema; mild nuchal rigidity, Kernigʼs sign positive, paraphasic error in speech , deep tendon reflexes normal and bilaterally symmetric. Labs Cytology by LP(lumbar puncture): cells 400/µl which mononuclear pleocytosis. Biochemistry: mildly elevated proteins, and normal glucose. Bacteriology exam. Negative. CSF-PCR reveals herpes simplex virus type-1. Serology: serum complement-fixing antibody titer more than 1:1000. EEG(electroencephalography):spiked and show waves localized to temporal lobes. Imaging: CT: characteristic changes of encephalitis seen over temporal lobes. Gross pathology: Hemorrhagic , necrotizing encephalitis most severe along inferior and medial regions of temporal lobes and orbitofrontal gyri. Micro pathology Brain biopsy reveals Cowdry intranuclear viral inclusion bodies in both neurons and glial cells with perivascular inflammatory infiltrates. Treatment Intravenous acyclovir. Discussion:-------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------Case-4 Mr.Fadhil left his place of employment at 3:00 P.M complaining of headache ,fatigue, general achiness,runny nose, cough and distinct chill. Headache and severe muscular aches ensued , and a temperature rise to 120F was noted by early morning of following day. Laryngitis with hoarseness and cough and substernal soreness were noted. Epistaxis was also noted. Physical examination revealed slight tachycardia and somewhat lower than normal blood pressure. The lymphoid follicles of the soft palate were enlarged and dewy in appearance. The nasal mucous membrane appeared bright red and there were areas of hemorrhage. The patient complained of loss of appetite and experienced a sense of fatigue and weakness. Nausea, vomiting or diarrhea were not observed. 1. 2. 3. 4. 5. The disease is diagnosed as ------------- which similar in C/F of--------The most common complication is------------------------------------------A specific therapy for the disease is-----------------------------------------The most effective disseminators occur in age group--------------------The control measures against the disease include-------------------------- Case-5 Complaint A 32-year-old woman comes in for a routine Pap smear. She has no complaints, but has not had a Pap smear before and she saw a TV program on it recently , prompting her to make the appointment. History The patient is healthy and has no significant past medical history. She takes no medications and does not illicit drugs or alcohol. She smokes roughly one pack of cigarettes per day. The woman is heterosexual and has multiple previous sexual partner, using birth control pills and condoms sporadically. PE The PE reveals no significant abnormalities. Full pelvic exam and pap smear are performed. Lab.tests Urine pregnancy test: negative Pap smear: atypical cells Routine culture for gonorrhea and Chlamydia : negative Cervical biopsy: koilocytic atypia in cell of upper epithelial laver. Qs: Which infectious organism is likely responsible for the changes? What is koilocyic atypia? What common clinical condition does this organism cause? What is relationship between this organism and cancer? Case-study in Mycologyology (Dr. Kareema Amine Al-Khafaji): the Case No.1 : A young aged lady presented with small rounded erythematous scaly lesion on the forearm with a mild itching , increases gradually in size especially after application of topical steroid (see the photograph). Q1 what is your diagnosis? Q2.what is the important test is used to confirm the diagnosis? Q3.How can you treat this patient? Q4. Is the topical steroid is the treatment of choice in the treatment? A1. Tinea corporis (here called Tinea incognito due to treatment by steroid). CaseNo2. A young- aged chide presented with multiple erythematous scaly lesions on the scalp, with localized hair loss of three weeks duration.(see photograph). Q1. What is your diagnosis. Q2.what is second differential diagnosis? Q3.How you can confirm the diagnosis? Q4. How can you treat such a case?