Occupational Health Department - Oxford University Hospitals NHS
advertisement
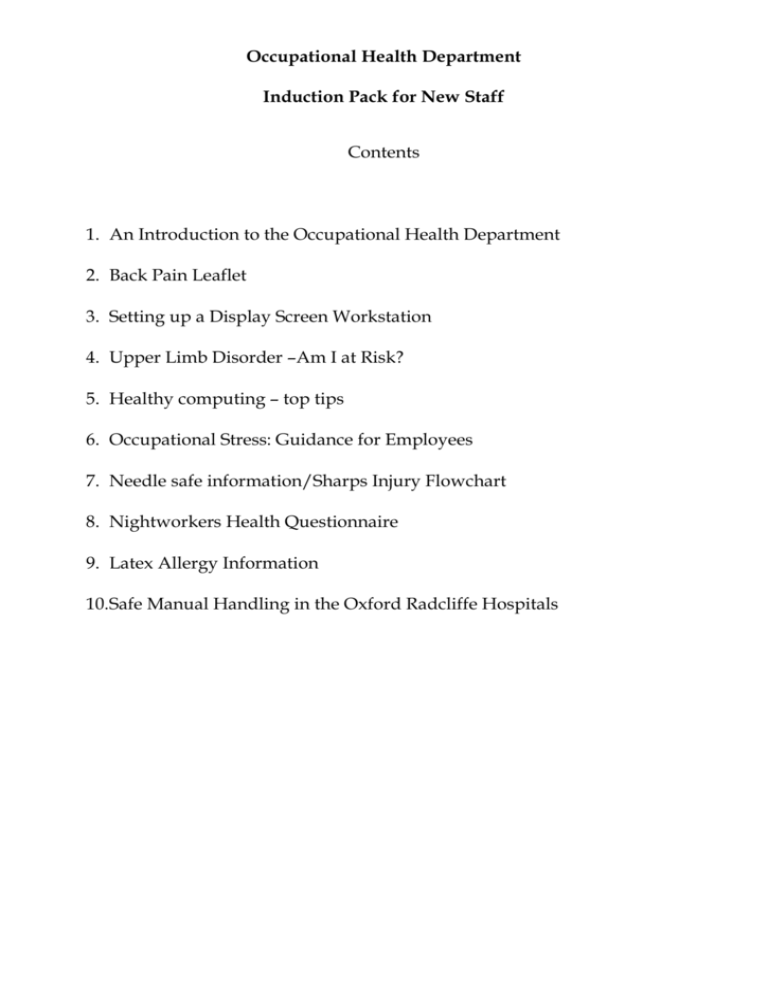
Occupational Health Department Induction Pack for New Staff Contents 1. An Introduction to the Occupational Health Department 2. Back Pain Leaflet 3. Setting up a Display Screen Workstation 4. Upper Limb Disorder –Am I at Risk? 5. Healthy computing – top tips 6. Occupational Stress: Guidance for Employees 7. Needle safe information/Sharps Injury Flowchart 8. Nightworkers Health Questionnaire 9. Latex Allergy Information 10.Safe Manual Handling in the Oxford Radcliffe Hospitals Occupational Health Department What is Occupational Medicine? Occupational medicine is the clinical speciality concerned with the diagnosis, management and prevention of disease caused or exacerbated by workplace factors. Who are the Occupational Health Team? The occupational health team consists of consultant occupational health physicians, specialist occupational health nurse advisers, experienced clinic nurses, physiotherapists, and ergonomic and back care advisers. The clinical staff are supported by our trained administrative team. What services are provided by the Occupational Health Department? The Occupational Health Department provides advice to employees and managers on issues regarding health at work. You can refer yourself to the Department or may be referred by your line manager. Our services include: 1. Pre-employment assessment 2. Advice to employees and managers on sickness absence issues Employees who have been off sick are likely to be referred to the Occupational Health Department by their line manager following the Trust’s Sickness Absence Policy. The referral letter and process should be discussed with you beforehand. 3. Physiotherapy triage service for staff who sustain a work related musculoskeletal injury Occupational health physiotherapy triage clinics provide fast access to advice on musculoskeletal work related concerns and injuries for staff. A physiotherapy treatment service is also available for work related problems including low back and upper limb disorders. Please contact the Department for an appointment. 4. Referral to counselling services Counselling for work related psychological ill health is available for all staff. This is provided by an external service and is not on-site. Please arrange an appointment with an occupational health advisor if you would like to be referred. 5. Assessment and support following exposure to blood borne viruses through needlestick/sharps or splash incident Any staff member who believes they may have been exposed to blood borne viruses (Hepatitis B, Hepatitis C, HIV) whether by splash or needlestick/sharps injury, need to attend the Occupational Health Department immediately. Out of hours needlestick injuries are dealt with by the on-call microbiologist who can be contacted by switchboard, informing the Occupational Health Department on the next working day. 6. Immunisations Health care workers and other staff who have contact with patients or body fluids will need to attend for assessment of their immunisation status as soon as possible. This will usually be on your first day. 7. Night Workers Health Assessment A night workers health questionnaire is enclosed with this pack and is offered to all staff undertaking night duty as outlined in the Working Time Regulations. The assessment is voluntary and employees are asked to send completed forms to the Occupational Health Department. 8. Health surveillance Staff exposed to certain workplace hazards are legally required to undergo appropriate health surveillance. For example allergy to latex is a key issue in the healthcare environment. Staff exposed to latex are asked to complete a latex screening questionnaire which will be reviewed by the Occupational Health team. The questionnaire is included in this pack. 9. Back Care and Manual Handling Training and Advice The back care and manual handling team provide specialist advice to all staff on manual handling and back care issues. This includes training for both clinical and non-clinical staff, advice on risk assessment and the investigation of incidents. 10. Advice on preventing ill-health at work including adjustments to the work environment 11. Guidance to managers and employees on occupational health aspects of relevant legislation Where are the Occupational Health Departments based and how can I contact them? John Radcliffe Hospital 01865 220798 (internal 20798) Monday – Thursday Friday 08:00 – 17:00 08:00 – 16:00 Horton General Hospital 01295 229442 (internal 29442) Monday, Tuesday, Wednesday and Friday 09:00 – 17:00 Please contact the Occupational Health Department at the John Radcliffe on Thursdays BACK PAIN Don’t suffer needlessly Occupational Health Physiotherapy Back Care Ergonomics Team BCET Office John Radcliffe Hospital Headington Oxford OX3 9DU Tel: 01865 740892 Intranet: Occhphysio-CH Julie Kelly MSc Health Ergonomics MCSP Cert OH Occhphysio March 2008 This leaflet is designed to aid your understanding of back trouble, and to help you recover quickly. The information is based on the latest evidence. THE FACTS Back pain affects almost everyone at some point in their life. Usually it has a simple cause and often gets better quickly on its own accord. Resting, beyond a day or two, is generally not helpful. Worrying about the problem or about the future can make matters worse. Hurting does not necessarily mean harming. The back is designed to move and work; doing too little is probably as bad as doing too much. Back pain does not need to be a permanent problem- if you manage it properly. The amount of trouble you get can be affected by your reaction to the pain. TWO TYPES OR SUFFERER One who avoids activity, and one who copes. The ‘avoider’ becomes frightened by the pain. The ‘avoider’ rests a lot, takes tablets and worries about the future. The ‘avoider’ believes that hurting always means further damage- it doesn’t. The ‘coper’ realises the pain is temporary and behaves as normally as possible. The ‘coper’ accepts it will soon get better and has no fears for the future. The ‘coper’ deals with the pain by being positive and taking little time off work. WHO SUFFERS MOST? ‘AVOIDERS’ suffer the most. They have pain for longer, have more time off work and can become disabled. ‘COPERS’ suffer less at the time and they are healthier in the long term. Follow these guidelines – you really can help yourself. DO: Keep up daily activities. Avoid really strenuous things. It is important to stay active and continue as normally as possible. Try to remain at work or get back as soon as possible, even if you still have low back pain. Simple painkillers can be used to help manage your pain (follow instructions). A cold pack or local heat can be used for short-term relief. Speak to your manager if you feel there are issues relating to your job which affect your back. DON’T: Don’t worry. Back pain does not mean you will become an invalid. Don’t stay in bed. Remain active and positive, take control of the pain. Don’t let it persist. Speak to your GP, therapist and employer if you have not returned to work by about four weeks. REMEMBER… Contact Occupational Health for advice on back care at work. Back pain is common but rarely serious. Most back pain is only temporary; worrying will only make it worse. Gentle activity or light work is usually better than doing nothing. If you have severe pain that gets worse over several weeks, instead of better, see your GP. See your GP immediately if you have: Difficulty passing or controlling urine. Numbness around your back passage or genitals. Unsteadiness on your feet. DON’T FORGET- A POSITIVE, ACTIVE APPROACH TO BACK PAIN WILL MEAN LESS TROUBLE LATER. Setting up a Display Screen Workstation INTRODUCTION Improper use of Display Screen Equipment (DSE) or a badly set up workstation may result in musculoskeletal problems such as, tennis elbow, tendonitis, trapped nerves (pins and needles) and neck/shoulder pain. These symptoms can develop slowly, so please take time to complete a DSE risk assessment form with your departmental assessor so that your workstation can be altered to minimise the potential risk of problems. Please note that possibly the most useful advice that we can give is to avoid long periods doing the same task, therefore consider how you can rotate your tasks throughout the day as much as possible and take your rest breaks. There are regulations that govern how we should work with DSE. REQUIREMENTS OF THE DISPLAY SCREEN EQUIPMENT REGULATIONS 1992 Each DSE users workstation* must be assessed and any necessary changes made to minimise health and safety risks. The assessment will need to be reviewed if there is a change in task requirements, hardware, software, furniture, lighting or the workstation is relocated. *This includes workstations at home if this is recognised as part of the users work. Staff who need to move around working with laptops must receive training so they understand how they can prevent the development of musculoskeletal discomfort. Shared workstations must be fully adjustable so that each individual can adjust it for their own use. In summary:1. Rest breaks and task rotation must be incorporated into the working day. 2. The work chair must be fully adjustable, see below. 3. The screen must have a stable image, be adjustable and readable with no reflection or glare. The screen must not be too far offset to the right or left and be at a height where the user will be looking horizontally to the top of the display screen. (Users with glasses will need to ensure their head is not tilted forward or back to see the screen through the appropriate part of their lens) 4. The keyboard must be adjustable, detachable and legible. 5. The mouse should be kept within easy reach, immediately alongside the keyboard. 6. The work surface must be large enough for the work done by the user, allow flexible arrangements and be glare free. Some users may require a document holder. 7. There should be adequate contrast, no glare or distracting reflections on the screen. Up lighters can be helpful. 8. Adequate window coverings must be provided to eliminate reflection and glare from daylight 9. There should be space under the desk to allow leg room and sufficient space to allow postural changes. 10. Distracting noise should be minimised. 11. The software must be appropriate to the task, adapted to the user, provides feedback on system status and no undisclosed monitoring. 12. Eye tests must be made available when appropriate, through the Trust nominated optician. SEATING AND POSTURE 1. Adjust the seat height so that the desk is at a comfortable height for paperwork or for working at the keyboard, angle at the elbow approximately 90o, with relaxed shoulders. 2. The seat back must be fully adjustable in height and tilt, independently of the seat. 3. The back rest should have a curve that should be adjusted to provide lumbar support to the 'small' of the back. 4. The seat should support the length of your thigh but not exert pressure behind the knees. The seat angle should ideally be parallel to the floor. Tilting mechanisms are available and will allow changes in posture during the day. (A slight forward tilt may be more comfortable for some individuals as it tends to promote a better posture but may make the user slide forward) 5. If you have arm rests they should support the elbows at 90o and also allow the chair to move under the work surface and allow access to the desk drawers. 6. A foot rest will be required if the feet do not rest firmly on the floor. 7. The screen height and angle should allow a comfortable head position with the head in the midline position, chin not raised or lowered. 8. The wrists should be in the midline position (straight) with minimal bending up, down or to the sides. 9. There should be sufficient space in front of the keyboard to support hands/wrists during pauses in keying. 10. There must be sufficient space and no obstacles under the desk so that the individual may change position/posture. 11. These principles apply to the set up of any DSE workstation, so do not forget to review your computer workstation at home! For further information and guidance please speak to your manager or local DSE Assessor. For additional support please contact your Divisional Back Care, Occupational Health or the Non Clinical Risk Advisors. To book onto the DSE course please contact your site Training department for details. Upper Limb Disorder Am I at risk? What is an Upper Limb Disorder? (ULD) The term upper limb disorder refers to a variety of symptoms which affect the muscles, tendons, nerves and blood vessels of the upper body commonly in the neck, shoulder, arms, wrists, hands and fingers. Symptoms may include pain, swelling, cramps, tingling, heaviness and difficulty moving which if left unchecked may result in long term problems. Where this is related to work it is often called work related upper limb disorder WRULD. What will put me at risk? If you have had a previous problem or injury to an upper limb you might be at increased risk. Work related risk factors include: Repeating a task or activity. This may sometimes involve small but frequent movements. Working in an awkward position i.e. above shoulder height, or the arm or joint is at a difficult angle, or having to hold a static position. Having to use force to overcome friction, resistance or hold a tool. Prolonged exposure to a repetitive activity. Working in a cold environment can alter your ability to grip items and may alter your sensation. Some work activities may expose an individual to vibration through the hand or arm. Is my manager aware of these risks? Your manager will have already considered which activities are performed in your department, have completed risk filters and where applicable full risk assessments as outlined in the ULD policy. After the risk assessment has been completed your manager will consider how to reduce the risk to the team and write a safe working procedure. Sometimes it may be necessary to change the way work is done or look at using different tools. Where it is not possible to make any changes then the work activity should be shared amongst staff so that the exposure of any one individual to the risk is reduced as much as possible. What action can I take? Be aware of the activities that may cause a problem and ensure you have been trained and use the safe procedures. If you have had a previous problem with your neck, shoulder, arms, wrists, hands or fingers before please be alert to the signs and symptoms of ULD and seek advice and assistance as soon as possible. Always take your rest breaks and change activities (using different muscles and parts of your body) throughout the day. If you think there is a work activity that should be reviewed or reassessed raise your concern with your manager. What should I do if I think I have a problem at work? Inform your manager and complete an incident form (this form is used to highlight hazards, concerns and near misses) You should also contact Occupational Health for their assistance and support. Please be aware that there are many hobbies and activities outside of work that may aggravate or cause similar problems. I.e. DIY, gardening, extra computer work, knitting! Manual handling and working for long periods of time with display screen equipment (DSE) and scanning equipment may also present similar risks. There is legislation and Trust policies that give more detailed guidance on these activities. For further initial information please speak to your manager, Back Care Facilitator or departmental DSE assessor. Please note that the most useful advice that we can give is to avoid long periods doing the same task; therefore consider how you can rotate your tasks throughout the day as much as possible and take your rest breaks. For further information and guidance please speak to your manager or local Back Care Facilitator. For additional support please contact your Divisional Back Care Advisor, Occupational Physiotherapist, Occupational Health or the Non Clinical Risk Advisors. There are similar leaflets available on manual handling and DSE. Healthy Computing Top Tips for Healthy Computing 1. Know how to adjust your chair and adjust it to your needs every time you use it. The backrest should be raised to give your lower back support. The seat height should position your elbows just above the desk height to minimize neck and arm pain. 2. A footrest is required if your feet are unsupported to help maintain your posture. 3. Organise your desk to have frequently used equipment close by (e.g. your mouse and phone). Stretching your arm just a bit to reach for items can easily aggravate your neck and shoulder. 4. Our bodies are meant to move. Change your position frequently and take short frequent breaks instead of longer infrequent breaks. Get up and walk around at least every hour. 5. Try to vary the tasks you do, avoid prolonged sitting and perform frequent neck, shoulder and back stretches. Moving around while still working (eg getting up to retrieve items from a printer) can really help minimize or prevent aches and pain. 6. Have the computer screen directly in front of you, the top of the screen at about eye level, and the screen at about arm’s length away to prevent eye strain. Have your eyes checked every 1-2 years or more often if you experience problems. 7. Attend to aches and pains early- inform your manager and Occupational Health. Physiotherapy Triage is available through Occupational Health (Ext 20798). 8. A laptop is not for continuous use. A separate keyboard and mouse plus screen raise are required. 9. Keep physically fit and active by taking regular exercise. 10. Education and training is available on the risks associated with computer work. Speak to your manager or Occupational Health. NB: See the Occupational Health Physiotherapy webpage for more detailed information How to access the Occupational Health Physiotherapy webpage on the Trust internet: Go to the Occupational Health webpage located in the “A-Z of Intranet Sites”. Then click on “Occupational Health Physiotherapy” folder to access more detailed information on workstation set-up and computer use. How to access the recommended DSE e-learning: Go to the Occupational Health Physiotherapy webpage and click on the link for the “DSE e-learning Jan 09”. Occupational Stress – Guidance for Employees Who is this guidance for? 1. Anyone can be affected by stress. This guidance provides information and recommendations for employees on tackling occupational stress and its causes. Stress at work can have a considerable impact on your home life, so this guidance is also to help relatives and friends give support. Details of how to find other information to help tackle stress can be found in the final section. What is stress? 2. Stress is a normal part of everyday life. The Health and Safety Executive defines stress as “the adverse reaction people have to excessive pressure or other types of demand placed on them”. This makes an important distinction between pressure, which can be a positive state if managed correctly, and stress that can be detrimental to health. 3. Working under some pressure can improve performance and give satisfaction when challenging objectives are met. But when demand and pressure become too much, they lead to stress. Stress can be caused by problems at work or away from work, or both. This fact sheet is about work-related stress – stress that is caused by or is made worse by work. What causes stress at work? 4. The HSE has developed six management standards (i.e. six key areas of work design) that cover the primary sources of stress at work. These include: 4.1 Demands – e.g. workload, work patterns and the work environment 4.2 Control – e.g. how much say a person has in the way they do their work. 4.3 Support – e.g. the encouragement, sponsorship and resources provided by the organisation, line management and colleagues. 4.4 Relationships – e.g. promoting positive working to avoid conflict and dealing with unacceptable behaviour. 4.5 Role – e.g. whether people understand their role within the organisation and whether the organisation ensures that they do not have conflicting roles. 4.6 Change – e.g. how organisational change (large or small) is managed and communicated in the organisation. What should the Trust to be doing to reduce occupational stress? 5. The Trust has a legal duty to protect your health and safety at work. 6. The Trust should identify the causes of occupational stress, assess the risk and take preventive action before employees are made ill. 7. You, or your health & safety representative, should be consulted about workplace changes that affect your health and safety, including those that might lead to stress at work. 8. You should cooperate by following policies and procedures and helping to identify problems and solutions. How should I recognise stress? Stress can manifest itself psychologically, physically and/or emotionally. Whilst an individual may be more prone to certain symptoms, these vary from person to person and in different circumstances. Symptoms include: Psychological Emotional Indecision Irritability or anger Muddled thinking Anxiety Loss of memory Numbness Feelings of inadequacy Hypersensitivity Low self esteem Feeling drained and listless Physical Behavioural Tiredness Insomnia Indigestion and nausea Changes in eating habits Headaches Increased smoking or drinking alcohol Muscle tension Avoiding friends or family Palpitations Sweating Sexual problems, disinterest or unsafe sex How should I help to tackle occupational stress? 9. The Trust and employees are jointly responsible for preventing stress at work. Ideally you should work together with your manager and trade union or other employee representative to tackle stress at work. 10. Talk to your Manager and/or Human Resource Manager if there are problems. It may be helpful to involve your trade union or other employee representative. If you feel you have difficulties going directly to your manager, your representative may be able to raise the issue for you. 11. Consider getting involved with the stress risk assessment for your department 12. Make an appointment to discuss the situation in confidence with Occupational Health. 13. Go to see your General Practitioner if you are worried about your health. Ideas for working together to find solutions for stress at work: Atmosphere Try putting forward constructive ideas regarding possible improvements to the work place Demands Prioritise your work, and if there is too much, suggest what could be dropped, put on hold or passed on, without putting too many demands on others. Tell your manager or trade union or other employee representative if you are beginning to feel you cannot cope, and make suggestions about how the situation could be improved. Identify new tasks you could do if you want more variety. Ask for information about hazards in your workplace if you are worried. Make sure you follow relevant policies and procedures. Control Ask for more responsibility in planning your own work. Ask to be involved in decision-making about your work area. Support Ask for feedback on how you do your job. If you get criticism, ask for suggestions instead. Relationships If you think you are being bullied, take action early by talking to your manager, employee representative, or other supportive colleague. If your manager is part of the problem, perhaps talk to your manager’s boss. Be prepared to give evidence to back up your claim; this may include keeping a record of when you feel you have been bullied with details, e.g. diary entries. Make sure your behavior to others always sets a good example. Role Talk to your manager if the responsibilities in your job are not clear; consider working with your manager to clarify your job description. Change Ask for information about changes – how they might affect you, what the timetable will be and the likely benefits and disadvantages. 14. Look after your health and welfare. Maintain a healthy diet with plenty of fresh fruit and vegetables, and drink plenty of water throughout the day. Drink caffeine and alcohol in moderation and avoid cigarettes. Ensure you incorporate regular exercise into your daily routine. Prioritise your sleep and maximise your opportunity for a good night’s rest. Keep up with family and friends for mutual support. What should I do after a stress-related illness? 15. You should make an appointment with the Occupational Health Department to look at why you became ill and ways to prevent further problems in the future. If you have been off sick the Occupational Health advisors and doctors will liaise with your manager to plan a return to work program for you. How can I help my colleagues, family members or friends if they are suffering from stress at work? 16. Talk things through, share experiences and offer your support. Encourage your colleague, relative or friend to discuss problems with their manager, trade union, and other employee representative, Occupational Health Department, Human Resources or GP, as a first step. 17. If their manager is part of the problem, you may be able to represent your colleague or you could suggest another manager that could help to deal with the situation. It may be helpful to brainstorm possible solutions to the problem together. Where else can I get information on work-related stress and its causes? 18. http://agency.osha.eu.int Fact sheets are available in this series on stress, bullying and violence. www.hse.gov.uk/stress/index.htm www.nhsemployers.org/stress www.livinglifetothefull.com Be Needle Safe How to Protect Yourself & Others from Needlestick Injuries Needlestick injuries can lead to serious or fatal infections. Healthcare workers who use or may be exposed to needles are at increased risk of needlestick injury. All workers who are at risk should take steps to protect themselves from this significant health hazard. What infections can be caused by needlestick injuries? Needlestick injuries can expose workers to a number of blood-borne pathogens that can cause serious or fatal infections. The pathogens that pose the most serious health risks are: Hepatitis B virus (HBV) Hepatitis C virus (HCV) Human immunodeficiency virus (HIV) – the virus that causes AIDS. HBV vaccination is recommended for all healthcare workers (unless they are immune because of previous exposure). HBV vaccine has proved highly effective in preventing infection in workers exposed to HBV. However, no vaccine exists to prevent HCV or HIV infection. Preventing needlestick injuries is the best way to protect yourself and others from these infections WHO IS AT RISK OF NEEDLESTICK INJURY? Any worker who may come in contact with needles is at risk, including nursing staff, laboratory staff, doctors, housekeepers, porters & waste collection team. WHAT KINDS OF NEEDLES USUALLY CAUSE NEEDLESTICK INJURIES? Hypodermic needles Blood collection needles Suture needles Needles used in IV delivery systems WHEN DO ACCIDENTS OCCUR? During use After use & before disposal Between steps in procedure While re-sheathing (this should never be done) HOW DO I PREVENT A NEEDLESTICK INJURY? ALWAYS watch what you are doing and ignore distractions whilst using needle. ALWAYS get help with uncooperative patients. It only takes a slight movement on their part to endanger yourself and the patient. ALWAYS cover all cuts and breaks in your skin with waterproof dressings or gloves. Wear gloves if there is a risk of contact with a patient’s blood, mucous membranes or body fluids. ALWAYS plan for safe disposal. Have sharps’ container at the point of use before opening and using needles. Never have a container in a position where you have to walk to it. ALWAYS dispose of used sharps in a sharps’ container, NEVER in plastic waste bags or waste bins. ALWAYS pick up all dropped needles carefully, and dispose of safely ALWAYS ensure sharps’ containers are placed out of the reach of children at all times, and that other unauthorised people cannot gain access to them. ALWAYS Handle used sharps’ containers with extreme care. Carry containers by the handle, and hold away from you. ALWAYS place any damaged used sharps’ containers into a larger secure rigid container, and properly label the outer container. ALWAYS keep Sharps’ Containers closed between uses. NEVER wear open footwear in situations where sharp instruments or needles are handled. NEVER relax until you have disposed of used needles into the sharps’ container. NEVER carry out another task with a used needle in your hand. NEVER lay needles down on bed-lockers, window-sills or work surfaces, or leave lying amongst swabs, dressing towels, etc. on a trolley. They must be immediately disposed of into a sharps’ container. NEVER pass needles directly from hand to hand. Handling should be kept to the absolute NEVER bend of break needles prior to or after use, or re-sheathe used needles. NEVER attempt to retrieve items from sharps’ containers or press down upon sharps to make more room Hands must never be inserted into containers. NEVER fill sharps’ containers above the manufacturer’s marked ‘fill line’. NEVER place used sharps’ containers ready for disposal in yellow or black bags. What do I do if I suffer a needlestick injury? Encourage wound to bleed. Do not suck. Wash wound well with soap under running water. Apply waterproof dressing. Report the incident to the senior person on duty in your area. Assess the infection risk: Unused/Clean needle – NO risk of infection. Contact First Aider or Occupational Health for advice if needed. Complete Incident Form. b. Used Needle – Call the Occupational Health Department immediately on: a. JRH (20798) CH (25553) Horton (29442) who will then provide the relevant follow-up treatment and/or information. Out of hours, call the on-call Microbiologist via the JRH switchboard. Complete the Incident Form. WOULD YOU DO THIS and pass the tissue to someone else to dispose for you? THEN DON’T DO THIS and pass the needle to someone else to dispose for you! TAKE THE SHARPS CONTAINER TO THE POINT OF USE AND DISPOSE OF SHARP YOURSELF Further information can be obtained from the ‘Prevention & Management of Sharps & Splash Injuries Policy’, available via the Clinical Governance Intranet Site – Policies & Procedures section. CRM Leaflet 08-01 Night Workers Health Questionnaire The Working Time Regulations require the employer to offer an initial and an annual health assessment to all night workers. A night worker is classified as an individual who regularly works for more than three hours during the period of 12 midnight to 6am. The assessment is voluntary and additional to any other health assessment undertaken via the Occupational Health Department. Completed questionnaires, designed to identify possible areas of special need in relation to night work, are held in confidence within the Occupational Health Department. If necessary a member of the Occupational Health Department will contact you if further assessment is required after reviewing your questionnaire. If you would like to have a health assessment, please complete this questionnaire and return it to the Occupational Health Department. Surname:…………………………………….First Name:……………………………….. Date of Birth:………………………………..Post:……………………………………….. Work Area:…………………………………..Manager:………………………………….. Contact Number:…………………………………………………………………………... Do you suffer from any of the following conditions? Please answer YES or NO to each. 1. 2. 3. 4. 5. 6. Diabetes? Heart and circulatory disorders? Stomach or intestinal disorders? Any conditions which causes difficulty in sleeping? Chest disorders, especially at night? Any medical condition requiring medication to a strict timetable? 7. Any other health factors that might affect fitness for night work? If you have answered YES to any of the questions above, please provide further details relating to the question number(s) below. Signature……………………………………………..Date:………………………………….. Latex Allergy Occupational Aspects of management Evidence-based guidance for employees [Produced by Royal College of Physicians for NHS Plus] This leaflet is about what to do if you are allergic to latex used at work, and measures that can be taken to minimise any problems so that you can stay at work. It is written for employees and summarises evidence-based guidelines.* *NHS Plus, Royal College of Physicians, Faculty of Occupational Medicine. Latex allergy: occupational aspects of management. A national guideline. London: RCP, 2008. Introduction Latex allergy (LA) is quite common and may lead to uncomfortable symptoms but it is rarely life threatening. Symptoms include itchy rash on the hands or other parts of the body; itchy, runny nose or eyes; wheezing and difficulty breathing. This leaflet is a guide to some of the things that can help you have fewer symptoms at work. In this guide, latex refers to natural rubber latex and not to synthetic (man-made) rubber. Should I be at work with my symptoms? If you are experiencing symptoms of latex allergy at work, it is important that you and your employer work towards creating a ‘latexsafe environment’. This should take place as soon as possible so that your symptoms do not become worse because you carry on being exposed to latex. Most individuals with LA can continue their work if a few changes are made to the work environment. You will need to be careful to avoid latex both in your work and home life, by not using latex-containing materials yourself and by avoiding areas where powdered latex gloves are still being used. Many everyday items contain natural rubber. It is important that you learn to avoid the items that are most likely to trigger your symptoms. Generally, ‘dipped’ rubber products such as gloves, balloons and condoms are more likely to trigger symptoms than solid rubber products such as tyres. Lists of products that contain natural rubber latex are available on the Latex Allergy Support Group website (www.lasg.co.uk/latexallergy/latextlists.htm). If you need to use gloves for your job, it is important that your employer provides you with suitable latex-free gloves. Your occupational health department or manager should be able to help you get these gloves. You also need to work in environments where there is no latex dust, for example from powdered latex gloves, as this can trigger symptoms of latex-induced asthma in people with a history of LA. Your manager should encourage colleagues to keep your contact with latex dust to a minimum by using powder-free latex gloves or latex-free gloves. What else could be considered in planning my future work? You may wish to find out if your organisation has an up-to-date working policy on latex, and if not, you may be able to start one being developed and implemented. It is important that your coworkers understand your allergy and how to help you avoid natural rubber latex products. Keep a positive frame of mind. Support from family, friends or others with the allergy may help you come to terms with your condition and manage your allergy better. What problems can I expect? Most employers should be able to make reasonable adjustments to your work to help your allergy. In rare cases, you and your employer may need to consider relocating you to another job within your organisation (redeployment). Occasionally, employers may not be aware of their responsibility to protect your health at work. It is important to be aware of laws that are designed to protect you: The Disability Discrimination Act 1995 places a legal duty on employers to make reasonable adjustments to your work to support your disability. Employers also have a duty under health and safety law to protect your health as far as they reasonably can. The Health and Safety at Work Act 1974 puts a general duty on employers to keep employees healthy and safe at work. The Control of Substances Hazardous to Health (COSHH) Regulations 2002 places a duty on your employer to assess any substances used at work that are hazardous to health, including natural rubber latex (www.hse.gov.uk/latex/law.htm). What if my symptoms continue? Most people with LA can stay at work after small adjustments are made in the workplace. But some people with LA can no longer work because their symptoms are too severe. If your illness was caused by your work, you may be able to claim compensation from your employer. You do not have to be unable to work to receive compensation. You may also be entitled to various social security benefits, work-related or otherwise, because of the restrictions placed on you by your allergy. More information is available from Jobcentre Plus (www.jobcentreplus.gov.uk). For a full version of the guidelines for latex allergy, see www.nhsplus.nhs.uk/web/public/default.aspx?PageID=331 Other sources of information British Association of Dermatologists Patient Information Gateway on Latex Allergy: www.bad.org.uk/public/leaflets/bad_patient_information_gateway_leaflets/latex/ Safe Manual Handling in the Oxford Radcliffe Hospitals Q A What law applies to lifting? The Manual Handling Regulations 1992 (amended 1994) Q Does it apply to me? A Yes, the requirements of these regulations apply to every employee, every employer and all places of work. Q What is ‘manual handling’? A The term ‘manual handling’ includes any task which involves the transporting or supporting of a load* including the lifting, lowering, pushing, pulling, by hand or bodily force. *includes patients. Q What does the law require? A Where reasonably practicable the employer should avoid the need for employees to undertake handling tasks at work. This may be achieved by either eliminating the need for the task to be done or by ensuring that mechanical aids/equipment are used wherever possible. Where manual handling tasks still remain a risk assessment must be done to establish the level of risk to staff. Training must be given to staff to ensure that the risk is reduced to the lowest level possible. Q Who will do the assessments? A Prior to each handling activity you must assess the task, the load, the environment and consider your personal ability at that moment. Managers are responsible for ensuring that the written assessments are completed and to identify the options to eliminate or reduce the risk to staff. Staff must then be trained in the safe handling procedure. Q Q Do I have to do anything? A Yes. Employees are required to make full and proper use of any equipment/aids and new systems of work introduced to make the task safer. Why has the law been introduced? A Moving and lifting tasks has been responsible for many injuries to staff. These include neck, arm, shoulder and abdominal injuries as well as back injuries. Many of these injuries could have been avoided with better fore thought, planning and training. Q What can I do to safeguard myself? A There are many simple things that can reduce the risk of injury but these principles need to be practiced at home and at work. Always avoid manual handling wherever possible. Assess the task and situation and prepare the area. Get help if you need it. Make full and proper use of equipment/aids eg hoists, sack trucks, trolleys etc. Always find out information about load you are going to move. Eg weight, shape, sharp, hot etc Wherever possible divide the load up into smaller units, rather than moving a large load. Try to organise your area so that items to be lifted are at waist height, to avoid bending. Where the item is low bend your knees and hips rather than your back. Keep the heaviest part of the load close to your body. Ensure you have sufficient space to work and that obstructions/ hazards are removed. Offer constructive suggestions to your manager if you consider that a task could be avoided or made safer by a change in working practice. Q What is the Trust doing to comply with the law? A Managers have to review all the manual handling tasks that are taking place in the department and ensure that the risks to staff from these are eliminated or reduced to a minimum. There is a minimal manual handling policy in the Trust. Each department will have a copy for you to read. Back Care Facilitators are trained to assist the managers in risk assessment, staff training and audit. Training courses are provided both locally and centrally for staff to attend. Equipment will be provided for you to use where appropriate. Q Is there anything else I could do? A Learn how to handle loads/ patients safely and what postures and activities at home and work may present a risk. Always work within your own capability. Keep fit and active. If you do have a back problem seek help from your GP and/or consult Occupational Health. Never hesitate to ask for help. Consider how you can improve the safety of handling activities outside work. Consider how you can minimise repetitive stooping, twisting postures For Further information please contact your local Back Care Facilitator or your site Back Care Advisor. Mary Ashford Ext 22108 Paul Crookes Div B Ext 22096 Linda Ramsbottom Div A Ext 22097 Sylvie Rugg-Easey Div C Ext 22095 Please contact your site Training department for details of and to book onto courses.