C-L Psychiatry Psychopharmacology Guide
advertisement

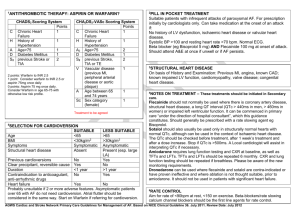
Sockalingam 2011 C-L Psychiatry Psychopharmacology Brief Guide General Principles: 1. Diagnostic clarity - understand both the underlying psychiatric disorder and comorbid medical conditions as much as you can 2. Clinicians should consider whether optimization of medical management or removal of potentially complicating medications is possible before initiating a new treatment. For instance, if the patient has insufficiently treated pain or nausea, that’s the first thing to get done, before starting a psych. medication for distress. Alternatively, if they’ve been on steroids, don’t need them anymore, and can be safely stopped, then get rid of those first, before embarking on a longer term course of a psych. med. 3. Target symptoms for proposed pharmacologic treatments should be identified. 4. Clinicians should consider possible drug interactions in vulnerable patient populations Careful consideration of the CYP450 system is paramount to minimizing drug-drug interactions. (see: http://medicine.iupui.edu/clinpharm/ddis/table.asp) 5. Pharmacologic parsimony is the ideal. Medications with favorable actions or side effects may be selected in specific scenarios. For instance, the oncology patient suffering from depression, nausea, weight loss, and sleep disturbance may benefit from pharmacodynamic properties of mirtazapine that address all these symptoms. 6. Psychopharmacology with the medically ill is shares a common approach with geriatric psychiatry – start low, go slow – but remember don’t stop until you have given an agent a full trial, unless side effects are limiting. 7. Drug information pharmacists at your institution and medical liaison officers from pharmaceutical companies may be very helpful in challenging cases. QUICK PEARLS: Renal Patients Some medications are affected by reduced renal clearance of active metabolites and should be avoided or require dose adjustment: o Almost completely: Lithium, gabapentin, topiramate Moderate-High: mirtazapine, venlafaxine, risperidone, paliperidone Delirious Patients Level II evidence (non-ICU) - Olanzapine, risperidone and haloperidol Level II evidence (ICU) – Quetiapine, IV haloperidol o NB: IV haloperidol is twice as potent as oral haloperidol Monitor the EKG for QTc when using antipsychotics – all antipsychotics can prolong QTc o QTc ≤ 450 msec – fine to proceed o QTc between 450 msec-500 msec – monitor closely and stabilize o IV haloperidol, Ziprasidone > other atypicals Hepatic Patients Hepatic function is key to metabolism and is measured by albumin, bilirubin, INR and platelets and is summarized by the Child-Pugh Score (Child-Pugh Sockalingam 2011 Calculators available online: http://www.mdcalc.com/child-pugh-score-forcirrhosis-mortality or ask medical team) General dosing adjustment for hepatic impairment using Child-Pugh Score: o Child A score – no dose adjustment o Child B score – 50%-75% o Child C score – 25%-50% Avoid benzodiazepines if possible if presence of hepatic encephalopathy Cardiac Patients Safety established for citalopram and sertraline Limit use of agents at risk of inducing cardiac arrhythmias when possible – TCAs or psychostimulants (unless risk/benefit assessed with cardiology involvement) HIV-Infected Patients Protease inhibitors (especially ritonavir) are potent inhibitors of CYP 3A4, so be careful with meds metabolized relying on this CYP450 pathway o Ex: Clonazepam, alprazolam